Salud Mental 2015;
ISSN: 0185-3325
DOI: 10.17711/SM.0185-3325.2015.004
Received first version: August 26, 2013. Second version: June 30, 2014. Accepted: July 2nd., 2014.
Clinical effectiveness of group cognitive-behavioural therapy for depressed older people in primary care: A randomised controlled trial.
Carmen García Peña 1 , Felipe Vázquez Estupiñan 2 , Fabián Avalos Pérez 3 , Leslie Viridiana Robles Jiménez 1 , Sergio Sánchez Garcia 1 , Teresa Juárez Cedillo 1
1 Unidad de Investigación Epidemiológica y en Servicios de Salud, Área Envejecimiento, Centro Médico Nacional Siglo XXI (CMN-SXXI), Instituto Mexicano del Seguro Social (IMSS), México.
2 Servicio de Psiquiatría. Hospital de Especialidades. CMN S XXI, IMSS, México.
3 Unidad de Medicina Familiar No 10. IMSS, México.
Correspondence: Carmen García-Peña MD, M.Sc., Ph.D., Unidad de Investigación Epidemiológica y en Servicios de Salud/Área de Envejecimiento, Edificio Corce, 3er piso, Centro Médico Nacional Siglo XXI, Av. Cuauhtémoc 330, Doctores, Cuauhtémoc, 06725 México, DF, México. Phone: (+52) (55) 5519-2724. Fax: (+52) (55) 5627-6900, ext. 21077. E-mail: carmen.garcia@imss.gob.mx
Abstract
Background. Depression is associated with an increased use of medical resources and reduced quality of life, cognitive functions, functionality and general health. The treatment of depression is limited by the scarcity of mental health professionals, as reflected in the mental health atlas of the World Health Organization.
Method. A randomised controlled trial that was not blinded was conducted. Family doctors referred patients older than 60 years who were suspected to have depression to the screening module. The PHQ-9 questionnaire, the Six-Item Screener, and previous diagnosis for psychiatric disorders were collected. Major depression was excluded. Those with a score from two to six on the PHQ-9 and with no comorbidities were referred to the Baseline Phase. A simple random process without blocking was applied. Groups of 7-10 participants engaged in weekly sessions over the course of three months. The control group was referred to their family physician. Reduction in depression score of the PHQ-9 was the main outcome.
Results and discussion. There were 40 patients in the control group (CG) and 41 in the intervention group (IG). 84% were women, 41% married and 41% reported at least primary education. The mean age for the GC was 69.7 years vs. 71.3 in the GI. The baseline mean MMSE score was 23.7 in the GC and 24.1 in the IG. No significant baseline differences between groups were reported. In the IG, 56% of the participants (n=23) displayed a decrease that was greater than or equal to 5 points on the PHQ-9 compared with 30% (n=12) in the control group. The CT group evidenced a marginal improvement.
Key words: Elderly, depression, cognitive therapy.
Resumen
Antecedentes. La depresión se asocia con un aumento en el uso de los recursos médicos y reducción de la calidad de vida, funciones cognitivas, funcionalidad y la salud general. El tratamiento de la depresión está limitado por la escasez de profesionales en salud mental, como se refleja en el atlas de salud mental de la Organización Mundial de la Salud.
Método. Se realizó un ensayo controlado aleatorio no cegado. Los médicos familiares referían a los pacientes mayores de 60 años con sospecha de depresión al módulo de detección. Se aplicó el cuestionario PHQ-9, la prueba de escrutinio de seis ítems, y el diagnóstico previo de trastornos psiquiátricos. Se excluyó a pacientes con depresión mayor. Aquellos con una puntuación de dos a seis en el PHQ-9 y sin comorbilidades fueron remitidos a la fase basal. Se aplicó un proceso aleatorio simple sin bloquear. Se integraron grupos de 7-10 participantes en sesiones semanales durante el transcurso de tres meses. El grupo control fue remitido a su médico familiar. El resultado principal fue la reducción en la puntuación de la depresión del PHQ-9
Resultados y discusión. Se estudiaron a 40 pacientes en el grupo control (GC) y 41 en el grupo intervención (GI). 84% eran mujeres, 41% casados y el 41% informó de al menos la educación primaria. La edad media para el GC fue 69.7 años vs. 71.3 en el GI. La puntuación media del MMSE fue de 23.7 en el GC y el 24.1 en el IG. No se registraron diferencias iniciales significativas entre los grupos. El 56% de los participantes del GI mostró una disminución que fue mayor que o igual a cinco puntos en el PHQ-9 en comparación con 30% del GC. El grupo CT demuestra una mejora marginal.
Palabras clave: Anciano, depresión, terapia cognitiva.
Background
In developed countries, the prevalence of depression in the elderly has been found to range between seven and 36% in out-patients and to be nearly 40% in hospitalised patients.1 Prevalence estimates from developing countries are scarce. In Mexico, for instance, the few depression prevalence studies carried out have not focused on persons 60 years and older and, consequently, sample sizes have been insufficient to yield precise estimates. 2,3,4 A recent report revealed a prevalence of 21% in Mexican adults above 60 years old.5 Minor, mild and moderate depression have been reported as the most common varieties of depression in the elderly.6
Depression is associated with an increased use of medical resources and reduced quality of life, cognitive functions, functionality and general health.7 In addition, uncontrolled chronic diseases and many medically unexplained symptoms are related to the presence of depression, particularly in the elderly.8
The treatment of depression is limited by the scarcity of mental health professionals, as reflected in the mental health atlas of the World Health Organization.9 Moreover, antidepressants may cause adverse consequences such as falls and confusional states associated with hyponatremia.10 The medical literature has suggested that minor and mild depression are more responsive to psychosocial interventions. Cuijpers11 reported a systematic review of 25 randomised controlled trials and concluded that non-pharmacological, psycho-educational interventions are effective for the treatment and prevention of depression. Katon et al.12 reported a randomised trial of an intervention in which either a nurse or psychologist offered the patient the option of antidepressant medication or problem-solving treatment in primary care. The intervention was at the individual level and lasted one year. The authors concluded that problem-solving treatment results in substantial clinical benefits at a low increment in health care costs; however, the number of health personal required was not mentioned. Serfaty et al.13 reported an intervention trial of individual behavioural cognitive therapy provided by qualified therapists. After 10 months, they found improvements in the experimental group compared with the control group.
However, the implementation of such strategies at the primary care level is difficult. Obstacles such as the scarcity of specialised human resources are an important issue. In Mexico, there are only 2.7 psychiatrists per 100 000 habitants compared with the United Kingdom, which has 11 per 100 000. Nearly all of the psychiatrists in Mexico are located in urban areas and only 33% work in public institutions.9 In the Mexican Institute of Social Security, which covers 42% of the Mexican population, psychological and psychiatric services are mainly located in general and high technology hospitals.
Consequently, it is a priority to identify strategies based on primary care that enhance access. Nurses may deliver group psychosocial interventions to improve depressive symptoms in older patients, maintain their families and daily activities, combat feelings of isolation and promote the development of new social networks. Therefore, the aim of the current study was to determine the clinical and well-being effects of a group cognitive-behavioural intervention provided by nurses to elderly Mexican patients.
Methods
This was a randomised controlled trial that was not blinded. The Ethics Committee at the Mexican Institute of Social Securty (IMSS) approved the protocol (2001-785-015). The data reported here are from the last section of the “Integrated study of depression among elderly insured by the IMSS in Mexico City”.5
Setting
The trial took place at the Mexican Institute of Social Security (IMSS) in Mexico City. The IMSS is a mandatory social security system that offers a comprehensive package of benefits, including health care at all levels and economic benefits such as a retirement pension. IMSS-insured workers and their close relatives are affiliated to a Family Medicine Clinic based on their home address. The elderly who are insured by the IMSS are more likely to have six or less years of education than their non-IMSS-affiliated counterparts. There are 41 family medicine clinics located in Mexico City. From these, Family Medicine Clinic number 10 was selected because it is the only family medicine clinic with a psychiatric service, 27 family medicine clinic rooms, 54 family doctors, a population coverage of 13 000, and a schedule from 8 am to 8 pm.
Recruitment
Participants were men and women who were insured by the IMSS and registered with the Family Medicine Clinic number 10, located in the southwest area of Mexico City. The protocol was presented to the staff clinic, and the research team asked the family doctors to refer all patients above 60 years old who were suspected to have depression to the screening module. The screening module was run by two trained interviewers who applied the PHQ-9 questionnaire14,15 in the Spanish version developed by the original research group.16 The Six-Item Screener derived from the MMSE17 and integrates three-item recall (apple, table, coin) and three-item temporal orientation (day of the week, month, year). The scale has been reported valid and reliable to identify patients with cognitive impairment and dementia. Also, it was collected a self-report of previous diagnosis for alcoholism, dementia, psychosis, schizophrenia or bipolar disorder, and self-report of actual drug treatment with haloperidol, lithium, quetiapine, lamotrigine, olanzapine or risperidone. Participants with major depression (seven or more points on the PHQ-9) were referred to the psychiatric service.
Participants with a score from two to six on the PHQ-9, with three or more points on the Six-Item Screener, without self-report of psychiatric disorders or actual psychiatric drug treatment were referred to the Baseline Phase module. This module was run by trained interviewers who applied a full questionnaire that included sociodemographic variables, quality of life, and cognitive impairment, which was assessed with a previously validated Mexican version of the Mini-Mental State Examination (MMSE).18 A threshold of 23 points or less was used to indicate cognitive impairment. Anxiety, health services utilisation, morbidity, instrumental and daily life activities and social support networks were also measured.
Randomisation
A simple random process without blocking was designed using open access software. After informed consent was obtained by the social worker, the receptionist contacted the Central Module and the research assistant reported the participant’s group allocation, according to the consecutive list.
Intervention and nurse training
Three nurses were trained as group leaders in cognitive-behavioural therapy. The training consisted of 30 hours of class time and was provided by a clinical nurse specialist (CNS) in adult psychiatric-mental health nursing, with participation by a psychiatrist. The CNS was an experienced group therapist and provided supervision for the duration of the project. The nurses were “technical nurses” (graduates of non-university-based programs), two of whom had post-diploma certification as psychiatric nurses.
The nurses led groups of 10 elderly patients for a period of 12 weeks, with sessions held once per week and lasting one hour and a half. The treatment modality was a cognitive-behavioural therapy based on the program of Muñoz, Aguilar-Gaxiola and Guzman.19 Cognitive-behavioural therapy is based on the interconnection between thought, behaviour, and feelings. A didactic portion of the program covered how patterns of thought and behaviour influence feelings to worsen or improve depression. Participants were helped to identify depressive thoughts, substitute them for more realistic and positive thoughts and regularly measure their mood states. They were assisted in setting and attaining goals, developing pleasurable activities, improving social relationships, and forming and maintaining social support networks. Group members actively participated and at times, exceeded the expectations of the programmed activities by providing appropriate movies and food to share with the group.
Control group
Participants who were allocated to the control group were referred to their family physician to receive usual treatment.
Outcomes and measures
Reduction in depression, measured via the PHQ-9, was the main outcome. A secondary outcome was health-related quality of life (HRQOL), which was measured with a previously validated Mexican version of the 36-item Short Form Health Survey (SF-36).20,21,22 Scoring was performed using the RAND algorithm,23 which produces an overall SF-36 score and scores for 8 subscales (physical functioning, role limitations due to physical health or emotional problems, vitality, emotional well-being, social functioning, bodily pain and general health). Scores range from 0 to 100, with higher scores indicating better health-related quality of life. Anxiety was assessed by means of the Short Anxiety Screening Test (SAST).24 Designed by G. Sinoff et al. in 1999, this scale was developed to standardise the detection of anxiety in the elderly, including in the presence of depression. This instrument includes somatic symptoms, a common manifestation of anxiety in the elderly. It is composed of 10 questions and, thus, is relatively easy to administer in epidemiologic surveys.
Health care utilisation was assessed through two questions about health care use during the previous six months (“for any reason” or “because of emotional problems”) and questions about the type of healthcare facilities attended in each case (whether at specific IMSS healthcare facilities or any healthcare institution). A self-report of chronic and acute diseases and the Charlson index for comorbidity25 were also collected.
Data collection began in December 2009 and concluded in May 2010.
Statistical analysis
The main outcome was the clinically relevant modification in the PHQ-9 score. Intervention effectiveness was defined as a decrease of at least 5 points on the PHQ-9 after 12 weeks. The statistical significance of the differences in mean changes of numerical variables in the intervention and control groups was assessed using t-tests, following verification that the distributions were reasonably represented by the Gaussian model. The statistical significance of the differences in changes in proportions (gender, previous diseases, death of a first degree relative, chronic disease status) was assessed by logistic regression of the modification in the PHQ-9 score (more or less than 5 points controlling for the initial PHQ-9 proportions by inclusion in the model).
Most analyses excluded subjects who dropped out before the final assessment; however, intention-to-treat analyses that include all subjects are also reported for key comparisons.
Results
A total of 143 participants were referred by the family physicians to the screening module. Of these patients, 126 completed their appointments. Of those who completed their appointment, 43 were excluded (29 patients had a score lower than two on the PHQ-9 and 14 had a score of major depression or were under psychiatric treatment). Eighty-three patients were scheduled for a baseline interview, and one patient did not show up. Then, 82 patients were consecutively randomised into the two groups, 41 patients were assigned to the intervention group (IG) and 41 to the control group (CG).
The participants’ baseline sociodemographic characteristics are presented in table 1. There were no significant differences between the groups. More than 80% of the participants were women (85% in the IG and 80% in the CG), and the mean age was 70.8 (s = 7.4) (70.39 in the TG and 70.15 in the CG). Marital status, level of education, number of inhabitants in the participant’s household, insurance status, religion, paid work, main occupation, and income source did not significantly differ between the two groups (p>0.05).
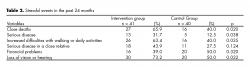
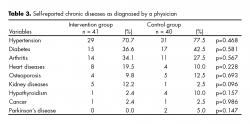
Regarding stressful events, there were more close deaths in the IG (27) than the CG (16). Furthermore, a major proportion of patients in the IG reported serious disease in the past 24 months (13 vs. 5), increased walking difficulties (26 vs. 16) and loss of vision or hearing (30 vs. 20) (table 2). The number and type of chronic diseases were similar in the two groups (p>0.05). Hypertension was present in 29 patients in the IG and 31 in the CG, and diabetes was present in 15 in the IG and 17 in the CG ( table 3).
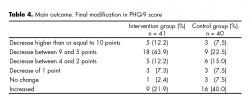
Regarding the outcome of depression, differences were classified according to Korenke K et al.14 In the IG, 56% of the participants (n = 23) displayed a decrease that was greater than or equal to 5 points on the PHQ-9 compared with 30% (n = 12) in the control group. A decrease between 4 to 1 points was obtained by 19.5% (n = 8) of the participants in the IG versus 22.5% (n = 9) in the CG. None change or increase of up to 5 points were reported in 10 participants (24.3%) in the IG and 19 (46.3%) in the control group (table 4). Item number 4 (Feeling tired or without energy) was reported with a reduction of 1 to three points in 22 participants (53.6%) of the IG compared with 10 (25%) in the CG (p = 0.02). A reduction of 1 to 3 points was found in the Item 6 (Feeling bad about yourself) for 20 participants (48.7%) in the IG and 8 (20%) in the CG. Differences in reductions were not found statistically significant.
Discussion
Late-life depression has been linked with high rates of health services utilisation, poor quality of life, loss of functionality and even increased death;26,27 thus, it is an important health public issue.
This report presents results from a pragmatic trial based on a feasible primary care intervention. A group cognitive-behavioural therapy carried out by trained nurses reduced the depression levels of elderly participants. A significant clinical reduction of greater than or equal to 5 points on the PHQ-9 was obtained for more than 50% of the patients in the IG after a 12-week program. Our main aim was to test a non-pharmacological treatment that can be transferred into health services. Similar individual interventions based on cognitive therapy have been tested.13 However, the number and extent of resources utilised make knowledge transfer into usual clinical practice quite difficult in countries with financial limitations such as Mexico. Thus, innovative strategies for care are an urgent necessity.
Although the current findings warrant attention, several limitations must be noted. The number of participants referred to the screening modules was surprisingly low. Family physicians were encouraged through clinical sessions and pamphlets to refer patients who were suspected to have depression and no additional work load was requested. The underestimation of depression may be explained by the stigma and prejudice of family physicians. In addition, the short duration of the consultation may have led patients to underreport emotional and mental symptoms that they attribute to physical health causes and assume are a normal consequence of aging. Also patients had no assessment of visual and auditory acuity. We recognize the importance of having obtained such sensory characteristics and thus be able to assess the level and capacity of reception and understanding of cognitive behavioral strategy used.
Participants’ and researchers’ blindness to the intervention was not considered. However, the main researcher was not involved in the progress of the intervention and the baseline and final interviewers were not aware of the participants’ assigned group. The effect of nurse characteristics such as age, personality or greater allegiance was not analysed; however, such characteristics may have a differential impact on the outcome. In this trial, three nurses provided therapy and received constant supervision by the psychiatrist and the nurse specialist. Special sessions were implemented to discuss concerns and issues that arose during the group sessions. Consequently, we believe that the potential differential impact of nurse characteristics was not relevant. However, the implementation of such an intervention in the health services arena must consider a highly reliable screening process and psychiatrist supervision to detect major mental health problems that require specialised pharmacological treatment and/or hospitalisation.
More women were involved in the trial than men. A previous report5 showed that women reported a higher proportion of depressive symptoms (24.7%) than men (16.2%). However, the higher participation of women is not only explained by the higher prevalence of depression. It seems that women are more willing to participate and express their feelings openly in a group. Women engage well in group treatments.
If this intervention is reproduced and extended to an integral care plan for the elderly, the opportunity cost must be considered and financial and human resources must be reallocated. Recognition that the elderly’s health can be promoted has increased in the last few years; however, the notion that health promotion strategies for the elderly will save money is simplistic. Health policy makers must understand that these strategies will incur extra cost but will also represent future benefits in terms of a better quality of life, decrease in disability and the possibility of successful ageing.
Funding
No author of this paper has specific financial interests.
Conflict of Interest
No author of this paper has a conflict of interest, including specific financial interests, relationships, and/or affiliations relevant to the subject matter included in this manuscript.
Acknowledgements
The authors are grateful to Patricia Morales Esponda and Douglas C Nance, for their logistical assistance during the fieldwork. This project was supported by grants from CONACyT (Mexico) 2002-CO1-6868 and Mexican Institute of Social Security (IMSS 2002-382).
REFERENCIAS
1. Gallo JJ, Lebowitz BD. The epidemiology of common late-life mental disorders in the community: Themes for the new century. Psychiat Serv 1999;50:1158-1168.
2. Wagner FA, Gallo JJ, Delva J. Depression in late life: A hidden public health for Mexico? Salud Pública Mex 1999;41:189-202.
3. Medina-Mora ME, Rascón ML, Tapia R, Mariño M et al. Trastornos emocionales en población urbana mexicana: resultados de un estudio nacional. An Inst Mex Psiquiatr 1992;3:48-55.
4. Caraveo J, Martínez N, Rivera B, Polo A. Prevalencia en la vida de episodios depresivos y utilización de servicios especializados. Salud Mental 1997;20:15-23.
5. García-Peña C, Wagner FA, Sánchez-Garcia S, Juárez-Cedillo T et al. Depressive symptoms among older adults in Mexico City. J Gen Intern Med 2008;12:1973-1980.
6. Lapid M, Rummans T. Evaluation and management of geriatric depression in primary care. Mayo Clin Proccedings 2003;78:1423-1429.
7. Beekman A, Deeg D, Braam A, Smit J et al. Consequences of major and minor depression in later life: a study of disability, well-being and service utilization. Psychol Med 1997;27:1397-1409.
8. Prince M, Patel V, Saxena S, Maj M et al. No health without mental health. Lancet 2007;370:859-77.
9. World Health Organization. Mental health Atlas. Geneva: WHO Press; 2005.
10. Mottram PG, Wilson K, Strobl JJ. Antidepressants for depressed elderly. Cochrane Database Syst Rev 2006;25: CD003491.
11. Cuijpers P, Muñoz R, Clarke GN, Lewinsohn PM. Psychoeducational treatment and prevention of depression: The “coping with depression” course thirty years later. Clin Psychol Rev 2009;29:449–458.
12. Katon WJ, Schoenbaum M, Fan MY, Callahan CM et al. Cost-effectiveness of improving primary care, treatment of late-life depression. Arch Gen Psychiatry 2005;62:1313-1320.
13. Serfaty M, Haworth D, Blanchard M, Buszewicz M et al. Clinical effectiveness of individual cognitive behavioral therapy for depressed older people in primary care a randomized controlled trial. Arch Gen Psychiatry 2009;66:1332-1340.
14. Kroenke K, Sptizer R, Williams J. The PHQ 9 valdity of a brief depression severity measure. J Gen Int Med 2001:16:606-613.
15. Pinto-Meza A, Serrano-Blanco A, Peñarrubia MT, Blanco E et al. Assessing depression in primary care with the PHQ-9: Can it be carried out over the telephone? J Gen Int Med 2005;20:738–742.
16. Spitzer R, Kroenke K, Williams J et al. Validation and utility of a self-report version of PRIME-MD: The PHQ primary care study. JAMA 1999;282(18):1737-1744.
17. Callaham C, Unverzagt F, Hui SL, Perkins A et al. Six-item screener to identify cognitive impairment among potential subjects for clinical research. Med Care 2002;40:771-781.
18. Reyes de Beaman S, Beaman P, García-Peña C, Villa MA et al. Validation of a modified version of the Mini-Mental State Examination (MMSE) in Spanish. Aging Neuropsychol Cognition 2004;11:1-11.
19. Muñoz RF, Aguilar-Gaxiola S, Guzmán J. Manual de terapia de grupo para el tratamiento cognitivo-conductual de depresión. Santa Monica: The RAND Corporation; 2000.
20. Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36): I. Conceptual framework and item selection. Med Care 1992;30:473-483.
21. Zuñiga MA, Carrillo-Jimenez GT, Fox PJ, Gandek B et al. Evaluación del estado de salud con la Encuesta SF-36: resultados preliminares. Salud Publica Méx 1999;41:110-118.
22. Hays RD, Sherbourne CD. RAND 36-Item health Survey 1.0 Scoring Manual. Santa Monica, CA: The RAND Corporation; 1992.
23. Lehtonen R, Pahkinen E. Practical methods for design and analysis of complex surveys (statistics in practice). 2nd Ed. West Sussex: John Wiley & Sons LTD; 2004.
24. Sinoff G, Ore L, Zlotogorsky D, Tamir D. Short anxiety screening test- a brief instrument for detecting anxiety in the elderly. Int J Geriat Psychiat 1999;14:1062-1710.
25. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987;40:373-383.
26. Rowan PJ, Davidson K, Campbell JA, Dobrez DG et al. Depressive symptoms predict medical care utilization in a population-based sample. Psychol Med 2002;32:903-908.
27. Gallo JJ, Bogner HR, Morales KH, Post EP et al. The effect of a primary care practice-based depression intervention on mortality in older adults. Ann Intern Med 2007;146:689-698.