Introduction
Worldwide, there were 36.7 million of people living with HIV (PLWH) in 2015, with women accounting for 51% of the total (Joint United Nations Programme on HIV/AIDS [UNAIDS], 2015).
Mexico has a concentrated HIV epidemic, with low prevalence in the general population (0.23% in 2015) (UNAIDS, 2015), but higher prevalence in key populations such as men who have sex with other men (MSM, 17.3%), male sexual workers (MSW, 24.1%), transgender women (TS, 15.5%) and intravenous drug users (IDU, 2.5%) (Centro Nacional para la Prevención y el Control del VIH y el sida [CENSIDA], 2015). While HIV prevalence in women has been historically lower, heterosexual transmission is increasing (Centro Nacional para la Prevención y el Control del VIH y el sida, 2015). Women represent the group with the highest prevalence increase in the last years, growing from 16% to 21% between 2000 and 2014 (Secretaría de Salud & Dirección General de Epidemiología, 2016).
Women are more vulnerable to HIV infection. This vulnerability has been associated with biological, social, cultural and economic factors, such as less access to education, employment and health services (García-Sánchez, 2004; UNAIDS, 2012).
On the other hand, men tend to engage in riskier behaviors such as unprotected sex, higher number of sexual partners and drug use (Bautista-Arredondo, Servan-Mori, Beynon, González & Volkow, 2015) MSM may also face stigma due to sexual orientation which can be associated with lower access to health services, rejection, higher drug use and sex work (Logie, Newman, Weaver, Roungkraphon & Tepjan, 2016).
An HIV diagnosis is regarded as a stressful experience that may negatively affect mental health status. Studies have shown that PLWH have more mental health problems than the general population, with a two to five times higher prevalence of depression, anxiety, and suicide, as well as higher harmful substance use (Brandt, 2009; Catalan et al., 2011; Parhami, Fong, Siani, Carlotti & Khanlou, 2013; Sherr, Clucas, Harding, Sibley & Catalan, 2011).
Anxiety and especially depression have consistently been associated with poor antiretroviral treatment (ART) adherence (Safren et al., 2016; Smith Fawzi et al., 2016; Tao et al., 2016; Tatum & Houston, 2016), and are linked to poor virological control and lower CD4 T cell counts (Amanor-Boadu et al., 2016; Herkenham & Kigar, 2016).
Few international studies about psychological variables and HIV show results by gender. Thus, only 7% of the studies on anxiety and depression in HIV focus on women, and less than 25% disaggregate their results by gender of participants (Bayon et al., 2012). However, the studies show that more women than men with HIV experience depression, anxiety and worse quality of life (Lartigue, Casanova, Ortiz, Aranda & Flórez, 2004; Nogueira Campos, De Fatima Bonolo & Crosland Guimaraes, 2006; Saadat, Behboodi & Saadat, 2015).
In Mexico, we found few studies about the status of mental health in PLWH (Galindo & Ortega, 2010; Soto & Cruz, 2014), and these not report results by gender.
The aim of this study was to describe and compare the frequency and severity of depression and anxiety symptoms between men and women in a sample of ambulatory PLWH who attend a specialized clinic in Mexico City.
Method
Design
Data for this study was derived from a cross-sectional survey on condom use and serostatus disclosure carried out between 2012 and 2013. For this analysis, we used sociodemographic data and data from depression and anxiety tests.
Participants
HIV positive individuals between 18-60 years old, receiving outpatient care at the HIV specialist clinic, were invited to participate in this study. Additional eligibility criteria included: being on ART at the moment of the evaluation and having available viral load (VL) and CD4 T cell count determinations within the last six months. Illiterate patients and those with a record of cognitive decline or dementia were not eligible. Individuals with incomplete psychometric evaluations were excluded from the analysis.
Sample size was estimated at 290 individuals, using STATS® and considering the total number of CIENI patients in 2014 with a .05 standard error, 95% confidence level and 80% statistical power.
Setting
The study was carried out in the Center for Research in Infectious Diseases (CIENI, for its acronym in Spanish) of the National Institute Respiratory Diseases (INER, for its acronym in Spanish) between November 2012 and May 2013. CIENI is a specialist HIV clinic in Mexico City that provided medical care for over 2 300 inpatients and outpatients in 2015.
Measurements
An ad-hoc questionnaire was designed to gather basic sociodemographic data including gender, age, education, marital status, occupation and sexual orientation. Time since HIV diagnosis, CD4 T cell counts and VL of the last six months were obtained from clinical records.
Severity of depressive symptoms was measured through the Beck Depression Inventory (BDI), a 21-item self-report scale (Beck, Steer, Ball & Ranieri, 1996), adapted to the Mexican population (Jurado et al., 1998) and to Mexican PLWH (Rodríguez et al., 2012). Cut-off points to categorize severity of depression are: none or minimal depression ( < 9 points), mild (10-16 points), moderate (17-29 points) and severe ( > 30 points); minimal and mild indicate absence of clinical depression symptoms. Frequency of depression was obtained with the percentage of participants in each category and with the number of participant with absence or presence of symptoms.
Severity of anxious symptoms was assessed through the Beck Anxiety Inventory (BAI) a 21-item self-report scale (Beck & Steer, 1991). In Mexico, BAI psychometric properties have been studied both in general and psychiatric populations (Robles, Varela, Jurado & Páez, 2001). Cut-off points to categorize severity of anxiety are: none or minimal anxiety ( < 5 points), mild (6-15 points), moderate (16-30 points) and severe ( > 31 points); minimal and mild indicate absence of clinical anxiety symptoms. Frequency of anxiety was obtained with the percentage of participants in each category and with the number of participant with absence and presence of symptoms.
Procedure
Outpatients receiving care at CIENI-INER who met the selection criteria and signed the informed consent form were invited to participate. A confidential psychometric evaluation was applied, including questionnaires about sociodemographic and clinical variables, serostatus disclosure, pattern of sexual behavior, antiretroviral treatment adherence and depression and anxiety symptoms (Caballero-Suárez et al., 2014). For this study, sociodemographic and clinical variables were used, together with data from the Beck Depression Inventory (BDI) and Beck Anxiety Inventory (BAI).
Data analysis
Chi-square test or Fisher’s exact test were used to compare categorical variables in men and women, and Mann–Whitney U test was used for continuous variables. We used a non-parametric test because the variables did not have a normal distribution. Spearman test was used to evaluate the association between clinical variables and affective symptoms (anxiety and depression). Odds ratios were calculated to evaluate an association between gender and depression and anxiety symptoms. Individuals with incomplete questionnaires were excluded from the analysis; thus there is no missing data. The significance level was established at p < .05. Statistical analyses were carried out using STATA version 12.
Ethical considerations
The study was approved by the Research and Ethics Committee of the INER.
Results
We invited 320 PLWH to participate in the study; 295 were recruited, 25 declined and four were excluded from the analysis because they did not complete the psychometric tests.
Sociodemographic characteristics of the study population
A total of 291 PLWH were included in the analysis, 13.10% (n = 38) were women. Male to female ratio was 7:1.
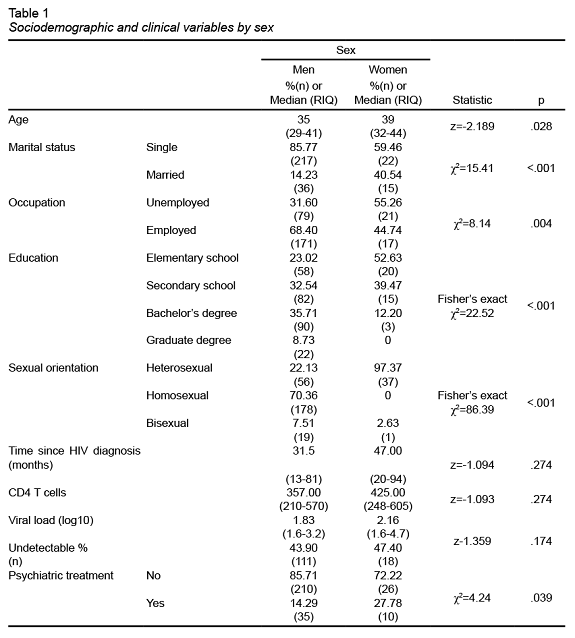
In bivariate analysis of sociodemographic variables, we found significant differences between men and women. All women self-identified as heterosexual, while only 22.13% (n = 56) of men did (χ2 = 86.39, p < .001). Women in the study were older than men (median age women = 39, men = 35, z = -2.18, p = .028); 40.54% of the women were married, compared to 14.23% of the men (χ2 = 47.32, p < .001). Women had significantly less years of schooling than men (52.63% of women had only studied up to elementary school versus 23.2% in men, χ2 = 22.52, p < .001). More women than men lacked a paid employment (55.26% versus 31.60%, χ2 = 75.99, p < .001), since a large percent of women self-described as housewives. As for clinical variables, we found no differences in viral load, CD4 T cell counts or time since diagnosis, but more women than men reported being under psychiatric treatment (27.78% of women versus 14.29% of men, χ2 = 4.24, p = .039) (table 1).
Comparison of depression symptoms between women and men
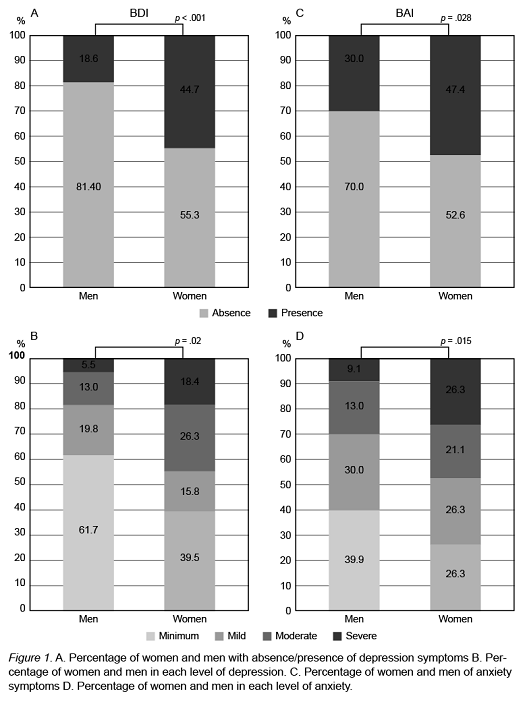
We found a higher frequency of depression in women than in men, measured as percentage of individuals with clinical depression symptoms (women: 44.7%, n = 17, men: 18.6%, n = 47; χ2 = 13.18, p < .001). Severity of depression was higher in women than men, median BDI score was 13 points for women (interquartile range [IQR] = 5-25) versus 6 points for men (IQR = 2-14, z = -3.08, p = .002) (figure 1A). Cut-off points to categorize severity of depression indicated that 18.42% (n = 7) of women versus 5.53% of men obtained scores that indicated severe depression, and 26.32% (n = 10) of women versus 13.04% (n = 33) of men with scores indicated moderate levels of depression (figure 1B).
In an unadjusted analysis, women had 3.5 times higher risk than men of presenting depression symptoms (OR = 3.54, 95% CI = 1.61-7.65, p < .001).
Comparison of anxiety symptoms between women and men
We found a higher frequency of anxiety in women than in men, measured as percentage of individuals with clinical depression symptoms. Clinical anxiety symptoms were present in 47.37% (n = 18) of women versus 30.04% (n = 76) of men (χ2 = 4.54, p = .028). Severity of anxiety was higher in women than men, BAI median score was 14.5 points (IQR = 3-35) in women and 8 points (IQR = 2-17) in men (z = -2.45, p = .014) (figure 1C). Severe anxiety levels were reported by 26.32% (n = 10) of women versus 9.09% (n = 23) of men. Moderate anxiety was present in 21.05% (n = 8) of women in comparison with 20.95% (n = 53) of men (figure 1D).
The unadjusted analysis showed that women had two times higher risk of having anxiety symptoms than men (OR = 2.01, 95% CI = 0.98-4.42, p < .033).
Comorbid anxiety and depression symptoms were found in 51 study participants (17.5%). Thirty-four percent (n = 13) of women had dual symptoms versus 15% (n = 38) of men (x2 = 8.41, p = .006). As expected, the BDI and BAI scores were associated with a coefficient in women of r = 0.59, p < .001 and in men of r = 0.69, p < .001.
Association of affective symptoms and clinical variables
We carried out an association analysis between anxiety and depression symptoms and clinical variables (CD4 T cell count and viral load). In women, but not in men, we found that a higher BDI score was associated with a higher viral load (women r = .48, p = .04; men r = .03, p = .68). Anxiety was not associated with CD4 T cell counts nor with viral load.
Discussion and conclusion
Our study provides evidence that HIV positive women in this center have a higher frequency and severity of anxiety and depression symptoms than men, and that more severe depression symptoms are associated with higher viral loads in women, in an unadjusted analysis.
Our results are in line with international studies showing that affective and anxiety disorders are the most common psychiatric comorbidities related to HIV-AIDS (Salters et al., 2016). Depression and anxiety rates in PLWH range between 20% and 70% (Berger-Greenstein et al., 2007; Elliott, 2003; Nogueira Campos et al., 2006) and 10% to 40%, respectively (Bayon et al., 2012; Wolff, Alvarado & Wolff, 2010). Estimated prevalence varies widely due to differences in the measurements used and in the sociodemographic profiles of the populations evaluated (Moore et al., 2016).
In our study, in both male and women participants, anxiety symptoms were more frequent than depression symptoms. This contrasts with previous studies in outpatient PLWH, where depression has been shown to be more frequent (Bayon et al., 2012; Berger-Greenstein et al., 2007; Elliott, 2003; Nogueira Campos et al., 2006; Salters et al., 2016; Wolff et al., 2010); it could be explained due to time since HIV diagnosis of our sample, depression is more frequent after diagnosis. Women in our study not only showed higher vulnerability due to mental health issues, but also had social and economic vulnerability. In our sample, women were older than men, had lower levels of formal education and lower paid employment, the majority of them being housewives. These variables suggest social inequality (low education and low income), which has been linked to lower access to health services (UNAIDS, 2012). Our results show that the vulnerability profile of HIV positive women described in countries of low income is also present in HIV positive women in Mexico City (García-Sánchez, 2004; UNAIDS, 2012).
The strong association between anxiety and depression symptoms found in both men and women in our study is well documented in other studies (Adams, Zacharia, Masters, Coffey & Catalan, 2016; Li et al., 2016). This association is reflected clinically in the percentage of individuals with anxiety and depression comorbid symptoms, and further highlights the importance of providing mental health interventions that complement medical care.
In our study, higher levels of depression symptoms were associated with higher viral loads, a finding consistent with other studies (Amanor-Boadu et al., 2016; Herkenham & Kigar, 2016). However, this association was only found in women, the group with a smaller sample size. It will be important to confirm these results with a larger sample, and analyze them in light of other variables, such as ART adherence, to determine if adherence is a mediator variable between depression and higher VL.
Programs designed to decrease the mental health morbidity in PLWH are necessary to improve adherence, retention in care and quality of life. Appropriate responses require systematic information on mental health status of PLWH and comprehensive approaches considering the sex differences in mental health issues and other socioeconomic vulnerabilities. These results serve as a starting point for the design of gender-sensitive mental health interventions, yet additional research is required on a larger sample to confirm these results and further detail specific needs and vulnerabilities in women living with HIV.
Limitations
This comparative study used data from a cross sectional survey evaluating condom use and serostatus disclosure. The study and the sampling strategy were not designed to compare differences in variables by gender. However, the percentages of women and men in this analysis mimic the national proportion of women living with HIV in Mexico (Secretaría de Salud & Dirección General de Epidemiología, 2016), and the proportions seen at the clinic. Moreover, the study collected a limited amount of social and economic variables, and other variables may be important to further understand the vulnerability profile we have found in women living with HIV.
In the other hand, some PLWH that were invited did not accept to participate in this study and this could represent a bias of sample selection in our data.
Data analyzed come from a cross-sectional survey, yet it is well established that levels of depression and anxiety can change over time and according to the stage of HIV infection. For example, they can increase after an HIV diagnosis but improve after individuals learn to cope and adapt to the diagnosis. In further studies it will be important to include stage of HIV infection (recently diagnosed, starting treatment, etc.) as well as to follow individuals longitudinally to obtain a more accurate picture of frequency of anxiety and depression in this population overtime.
Funding
This study did not receive specific financial support.
Conflict of interest
The authors declare that there is no conflict of interest.
Acknowledgments
Authors are gratefully indebted to the people living with HIV who participated in this study; the Psychosocial team, the Virological Diagnostics Laboratory, and the administrative staff of the CIENI-INER for the facilities provided during data collection.