Introduction
Dual disorders is defined as the presence of an addictive disorder and a mental health disorder in an individual within a specific time (Volkow, 2007). This comorbidity is common, as indicated by epidemiological studies on general population (Kessler et al., 1997; Regier et al., 1990) and clinical samples (Weaver et al., 2003). The comorbidity is associated with a greater use of health services, different phenotypes, more severe symptoms, greater functional disability, and a worse evolutionary course (Burns & Teesson, 2002; Weaver et al., 2003).
There are very different subgroups comprised under the term dual disorders. The co-occurrence of alcohol and cocaine is frequently found in dual disorders samples, and it has been studied as a separate subgroup both in general population (Carroll, Rounsaville, & Bryant, 1993; Grant & Harford, 1990; Hedden, Malcolm, & Latimer, 2009; Johnson, Cottler, O’Leary, & Abdallah, 2010; Moss, Goldstein, Chen, & Yi, 2015; Stinson et al., 2005; Suttajit, Kittirattanapaiboon, Junsirimongkol, Likhitsathian, & Srisurapanont, 2012; Windle & Miller-Tutzauer, 1991) and clinical (Brady, Sonne, Randall, Adinoff, & Malcolm, 1995; Brown, Seraganian, & Tremblay, 1994; Heil, Badger, & Higgins, 2001; Vanek et al., 1996; Walsh et al., 1991) settings. Up to 60-80% of either alcohol or cocaine treatment-seeking individuals share both SUDs (Carroll et al., 1993). To date, results show that this comorbidity associates differential socio-demographic characteristics (Walsh et al., 1991; Windle & Miller-Tutzauer, 1991) and higher rates of drug use, depression, anxiety, and drug-related problems (Brown et al., 1994; Hedden et al., 2009; Moss et al., 2015; Stinson et al., 2005; Suttajit et al., 2012; Windle & Miller-Tutzauer, 1991) compared to single addiction.
There is little information about the prevalence of these disorders in Spanish population and specifically about the concurrence of alcohol and cocaine SUD. Likewise, a lack of information about its distribution between the two main healthcare networks in this regard is noticeable: the substance misuse and mental health service networks. The knowledge about the distribution of dual disorders and the characteristics of these patients can help to optimise health service resources. This information may serve also to hypothesize causal relationships and design further studies. In this work, we present data related to patients with concurrent alcohol and cocaine abuse or dependence criteria.
The aim of our study is to describe the co-occurrence of alcohol and cocaine SUD in Madrid’s healthcare networks. The main objectives are: measuring its prevalence in our healthcare settings, describing its socio-demographics, and analysing if the concurrence is associated to a specific or more severe psychopathology, compared to psychopathology found in individuals with only alcohol or only cocaine SUD.
Method
Design
We present a descriptive, cross-sectional study of outpatients under-treatment in the two main healthcare networks treating SUD, the substance misuse and mental health service networks. This is a post-hoc analysis from the results from a previous work. Material and methods are described in more detail in Arias et al. (2013a).
Sampling
The patients were consecutively screened by their own therapists in the substance misuse centres (Community of Madrid and Madrid Local Authority Substance Misuse Centres) and in the Community of Madrid Mental Health Centres. Usually, patients enter the Mental Health network referred both from public Primary Care assistance and public specialist assistance. Referral is normally motivated by the presence of any kind of psychopathology. Instead, patients enter the substance misuse centres by their own will, motivated by the existence of a SUD, and the main assistance relies on treating the substance problem. Still, we can find dual disorders patients in both settings as neither the existence of a SUD or the presence of psychopathology excludes a patient from receiving treatment respectively in the Mental Health and Substance Misuse Centres.
The individuals included were those older than 18 year who signed the informed consent. Whether they were attending for the first time or already had a follow-up schedule did not make a difference in the study. In order to get the highest number of patients and obtain stronger external validation, very few exclusion criteria were established. Patients were only excluded if they were not capable of filling the questionnaires due to cognitive deficits or a low educational level.
Measures/variables
A Data Collection Logbook was created in order to get socio-demographic variables. To determine the presence of lifetime mental disorders, the structured interview MINI (sensibility: .89; specificity: .92) (Lecrubier et al., 1997), that enables making diagnosis according to the DSM-IV (Diagnostic and Statistical Manual of Mental Disorders) and the ICD-10 (International Classification of Diseases) criteria, was used (Sheehan et al., 1998). MINI is an interview that allows the exploration of the main, current Axis I psychiatric disorders. Those disorders not evaluated on a lifetime basis by this tool were examined using the clinical interview. To determine the diagnosis of personality disorders, the PDQ4+ scale (Personality Disorder Questionnaire) was used (sensibility and specificity are yet to be determined) (Calvo, Caseras, Gutiérrez, & Torrubia, 2002). This tool combines a rapid and easy self-administered questionnaire together with a control observation of symptoms effect under the interview conditions.
Procedures
Eighty-one interviewers took part (psychiatrists, psychologists, or general practitioners with broad addiction experience) from 64 substance misuse centres and 17 mental health centres. All the interviewers received training on how to administer the structured interview. Two one-hour-length sessions took place before data collection to explain the methodology of the questionnaires. Interviewer’s doubts about the process were resolved. No calibration procedure was made to control the results. Patients’ participation percentage was 87.2%. Non-response was mainly due to lack of collaboration once the patient was included. Socio-demographic variables were recorded first in a simple interview. Then, the MINI interview was administered. After that patients were given PDQ self-questionnaire and finally the second part (clinical significance scale) was administered by an interviewer. The study was approved by the Research Ethics Committee of the Gregorio Marañón Hospital in Madrid.
Statistical analysis
We compared the distribution of the variables of interest in two separate analyses. In the first one we tested differences between Alc + Coc and Alc patients, and in the second we tested how Alc + Coc patients differed from Coc group.
Descriptive parameters were calculated on all the variables: mean and standard deviation in the quantitative variables. The qualitative variables are expressed by means of relative percentage frequencies. To detect differences in the distribution of qualitative variables we used the chi-square test (χ2). We used the Student’s t test for the quantitative variables (in this study only variables related to age were quantitative). The tests were considered to be significant if p < .05.
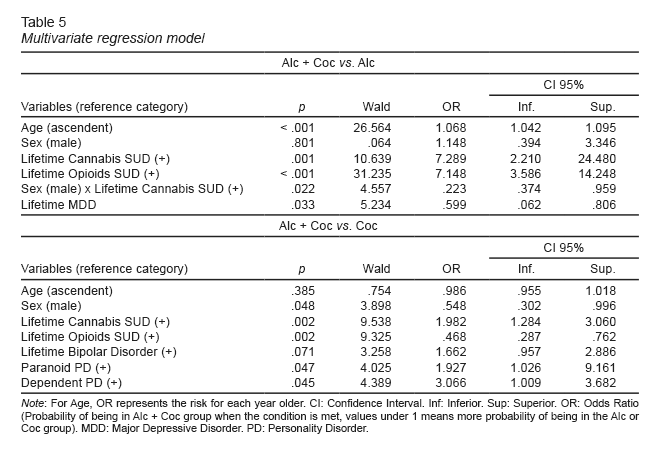
To control for possible confounding variables, a logistic multivariate regression model was conducted for each of the comparisons (Alc + Coc vs. Alc and Alc + Coc vs. Coc). In each case, the dependent variable was a dichotomous variable that represented the group membership. In the regression analysis, we included every variable that had shown significant differences between groups and also those variables that could have affected the results, as they are known to influence the presence of psychopathology or substance use (age and sex). A backwards stepwise regression model was obtained. We also tested possible interactions of the variables by including in the analysis those variables significantly correlated by Pearson’s test as an interaction factor. The statistical analysis was generated with the SPSS programme v.21.
Results
The study included 837 patients: 208 (24.9%) came from mental health centres and 629 (75.1%) from substance misuse services. There were 528 (63%) subjects with a lifetime alcohol SUD. Of these patients, 366 (69.3%) had a concurrent lifetime cocaine use disorder. Out of the whole sample, 488 (58.3%) subjects had a lifetime cocaine SUD, in which concurrence with alcohol SUD represented up to 75%. The sample was divided in three groups: Alc + Coc for the patients with concurrent alcohol and cocaine lifetime SUD, Alc for the patients with lifetime alcohol SUD but not lifetime cocaine SUD, and Coc for the patients with lifetime cocaine SUD but not lifetime alcohol SUD. There were 366 (43%) patients in the Alc + Coc group, 162 (19%) in the Alc group, and 122 (15%) in the Coc group. In the Alc + Coc, Alc and Coc groups of which 353 (96%), 51 (31%), and 117 (96%) came respectively from substance misuse services. Finally, 187 (22%) of the patients had no alcohol nor cocaine SUDs.
Socio-demographics
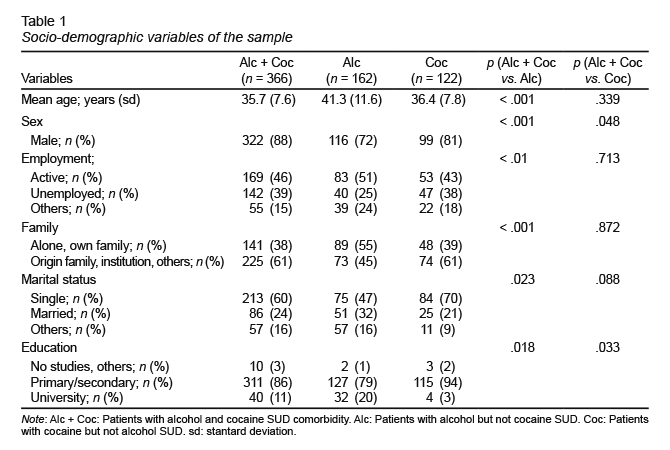
Table 1 contains patient’s socio-demographic characteristics and comparisons between Alc + Coc group and Alc group and between Alc + Coc group and Coc group as well. A majority of males was encountered in all groups. Compared to the Alc + Coc patients, subjects in the Alc group were significantly older, had a smaller proportion of unemployment, more of them were married and living with their own family, and had a higher level of education. A significant lower proportion of males was also encountered in this group. The only main difference found between Alc + Coc and Coc subgroups was the educational level, where the patients in the Alc + Coc group a higher proportion of individuals with university studies.
Prevalence of other SUD
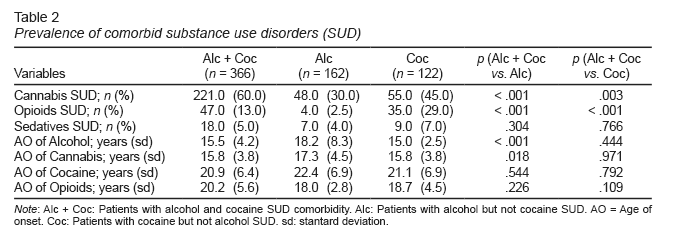
Table 2 shows the distribution of comorbid cannabis, opioids, and sedatives lifetime SUD in the three groups. Patients in the Alc + Coc group had a higher prevalence of lifetime cannabis and opioid SUD than those in the Alc group. On the other hand, although lifetime cannabis SUD was similar between the Alc + Coc and Coc groups, there was a significant higher proportion of patients with lifetime opioid SUD in the latter. There were no differences in sedatives consumption. Ages of onset of different consumptions were very similar between Alc + Coc and Coc groups. When comparing Alc + Coc to Alc, we found significant a lower age of onset of alcohol and cannabis.
Prevalence of mental disorders
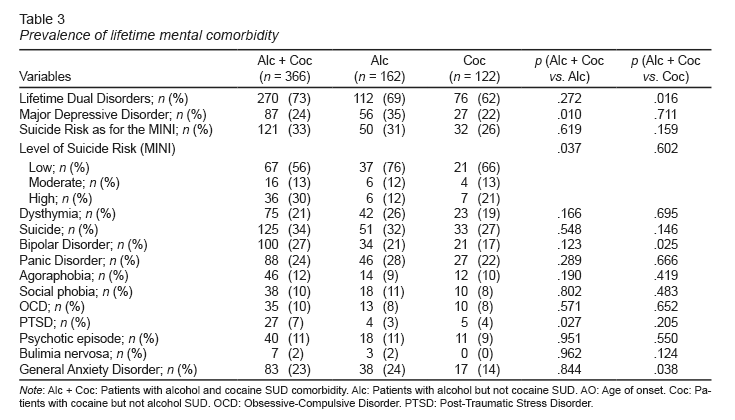
We found a high prevalence of dual disorders (60-70%) in the sample. The prevalence of lifetime mental disorders is shown in Table 3. A non-significant higher prevalence of dual disorders in the Alc + Coc than in the Coc group was observed for almost every category measured. The Chi-square test showed significant differences between Alc + Coc and Alc groups in major depression disorder (MDD) and dysthymia, which were higher in the Alc group. This group showed also a lower proportion of post-traumatic stress disorder (PTSD). Despite suicide risk being overall similar, Alc group had a lower proportion of individuals with high suicide risk than the concurrent SUD group. As for Alc + Coc and Coc groups, there was a significant lower proportion of bipolar disorder (BD) and general anxiety disorder (GAD) in the Coc group compared to the patients in the Alc + Coc.
Prevalence of personality disorders
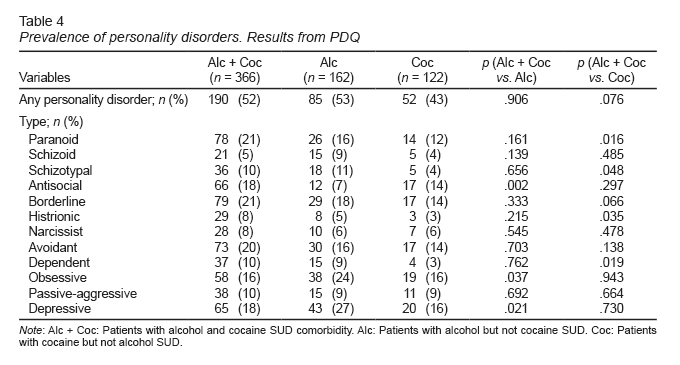
The prevalence of PD is shown in Table 4. In the same way as for the results found in mental comorbidity, the prevalence of PD was higher in the Alc + Coc group than in the Alc group. This was found in every diagnostic with the exception of obsessive and depressive PD. This higher prevalence reached statistical significance for the antisocial PD. Patients in the Coc group had less personality comorbidities compared to the Alc + Coc group. More specifically, these differences reached statistical significance for the paranoid, histrionic, and dependent personality disorders.
Multivariate regression model
Results from the multivariate regression model are depicted in Table 5. In the comparison between Alc + Coc group and Alc group, membership to Alc + Coc was significantly associated with older patients, the presence of lifetime cannabis SUD, and the presence of opioid SUD. MDD was significantly more associated to the Alc group. A significant interaction between the presence of lifetime cannabis SUD and males was observed. When comparing the Alc + Coc and Coc groups, there was a significant association between the Alc + Coc group and lifetime cannabis SUD, the presence of bipolar disorder, and the presence of paranoid and dependent PD. Female sex and lifetime opioids SUD was significantly more associated to the Coc group. The odds ratio and the confidence interval for these categories is shown in Table 5.
Discussion and conclusions
To our knowledge, the data from this study offers information about comorbidity between alcohol and cocaine SUD, and contains the highest numerous samples (837) of dual disorders patients undergoing treatment in our country. Our results are in concordance with previous studies in the distribution of socio-demographic, SUD, and mental comorbidity variables. Differences between the Alc group and the Coc group were not tested in this study since they had been published previously by our group (Arias et al., 2013b; Arias et al., 2013c).
Concurrent alcohol and cocaine abuse was associated with a poorer employment situation of the patients and being married in a lower proportion as well, and presented a lower degree of educational level compared to the patients in the Alc group. Interestingly, Alc - Coc patients showed similarities with the Coc group in terms of socio-demographic characteristics in all the variables except for educational level. Several studies have also addressed this existing socio-demographic differences (Brown et al., 1994; Hedden et al., 2009; Johnson et al., 2010; Walsh et al., 1991). Due to the cross-sectional design, we were not able to obtain causal relationships among these characteristics and the comorbid cocaine and alcohol addiction. Nevertheless, we believe this could be explained both from a social and biological perspective. From a social perspective, alcohol is widely used in a far larger proportion in our society; meanwhile, cocaine is less socially accepted. The Alc + Coc subgroup showed also earlier age of onset of alcohol and cannabis consumption, which has also been associated with social exclusion environments. Plus, people that use cocaine but not alcohol represent a small proportion of the patients under treatment. This subgroup shows highest opioid use percentages, a substance that is even less socially accepted than cocaine. From a biological perspective, we could say that cocaine is also associated with impulsiveness traits, carrying a handicap in terms of keeping a stable social situation.
We also registered higher rates of drug consumption in the Alc + Coc group compared to the Alc group, consistent with previous studies (Brown et al., 1994; Carroll et al., 1993; Hedden et al., 2009; Windle & Miller-Tutzauer, 1991). We found as well more prevalence of opioid SUD in the Coc group compared to the Alc + Coc group. This high prevalence (up to 29% in our sample) may reflect the existence of an specific subpopulation of cocaine and heroine users that could exhibit different characteristics. We also found more social-exclusion and different psychological characteristics in this group. Finally, we found significant earlier age of onset of alcohol and cannabis in the Alc + Coc group compared to the Alc group.
The prevalence of dual disorders was high and reached 70% in all the groups. Patients in the Alc + Coc group showed this diagnosis, both actual and lifetime, in higher proportions compared to the Alc and Coc groups. This higher proportion was not significant for all the variables measured, but there was a general tendency towards more frequent psychopathology. Patients in the Alc group showed however significant a higher proportion of MDD and a lower proportion of PTSD compared to the Alc + Coc group. These findings support previous results in the United States (Brady et al., 1995; Hedden et al., 2009; Johnson et al., 2010; Moss et al., 2015; Stinson et al., 2005) and in the Thai samples (Suttajit et al., 2012). This higher proportion of dual disorders renders concurrent alcohol and cocaine SUD patients more vulnerable. Moreover, complexity of SUD treatment increases significantly with the presence of psychopathology. Furthermore, there was as well a significant difference in the level of suicide risk, which was more frequent in Alc group, but a higher risk was found in the concurrent subgroup. Besides that, compared to Coc group, Alc + Coc group showed more proportion of BD and GAD, a difference also described previously (Heil et al., 2001).
While reviewing previous literature, we noted a high heterogeneity in the design of the studies. This heterogeneity could explain the differences with results obtained in our study. In this respect, individuals with both alcohol and cocaine SUD were previously associated (Moss et al., 2015; Suttajit et al., 2012) with higher proportion of depressive disorders than alcoholics without cocaine SUD, and this was not replicated in our sample. This difference could be explained by the fact that MDD is linked to female sex and ageing, which is present in higher proportion in the Alc group. However, this difference persisted after controlling for sex and age in our regression model. Alternatively, this difference might be explained by differences in the origin of the groups. Most of the patients with cocaine dependence (Alc + Coc, Coc) came from drug misuse centres. In Madrid it is at these units that cocaine users are mainly treated, whereas patients with MDD are usually followed in a mental health centre.
We found very few studies with personality disorders evaluation in individuals with cocaine and alcohol SUD. The Alc + Coc subgroup showed a higher prevalence of PD compared to the Coc group in hardly every diagnostic category and a similar prevalence to the Alc group. In previous literature, cocaine has been associated with higher prevalence of antisocial personality (Moss et al., 2015), and we could see similar results comparing Alc + Coc to Alc group. There was also, a higher prevalence of depressive PD in the Alc group. Compared to the Coc group, Alc + Coc showed a significant higher proportion of paranoid and dependent PD.
In the multivariate regression analysis, only a few of the significant differences found by the univariate test remained in the model. We must take into account that the influence exerted by poly-consumption and interrelationships that exist between different diagnostic categories, such as depressive PD and MDD or dysthymia, could affect the results. Nevertheless, we thought that our model could better highlight the disorders that could be influencing more heavily membership to Alc + Coc group.
Limitations
The SUD diagnosis was made by means of clinical interview. Neither the toxicological analysis nor the use of other sources or information were included in the protocol. This means that lifetime SUD diagnosis rely on the information provided by the patients, which could have influenced by means of their interest and the inevitable impact of bad memory. In this sense, most of the patients were known to substance misuse centre carers and therefore patients’ statements could be confronted when apparently false. In these centres urine testing is regularly carried out and this partially compensates the limitation.
Another limitation of the design of the study is the difficulty found in hunting specific psychopathology associated to concrete SUD, since poly-substance abuse is the norm among treated patients in mental health and substance misuse units. In this study extern validation was one of the objectives and so we did not use poly-substance abuse as an exclusion criterion.
We made two separate analyses (Alc + Coc group vs. Alc group and Alc + Coc group vs. Coc group) without using a p value correction for multiple analysis. This increases the probability of obtaining a false positive result, so significant differences should be regarded with precaution.
The results obtained in this study can be extrapolated only for samples of treatment-seeking patients in the Mental Health or Drug Misuse services. The treatment centres for these patients must be equipped to carry out the detection and associated management of these comorbid mental disorders. We believe the information here stated will help detecting the comorbidity amongst our patients, taking into account the more frequently associated psychopathology and targeting treatments towards more specific issues.
In conclusion, we have conducted a descriptive analysis of the comorbidity of alcohol and cocaine in a big sample of patients under treatment. We have found that both Alc + Coc and Coc groups shared a worse socio-demographic status. Likewise, patients in the Alc + Coc group had higher proportions SUDs compared to the patients in Alc or Coc groups, with the exception of opioids SUD, which was higher in the Coc group. Finally, concurrent alcohol and cocaine SUD was associated with more frequent psychopathology as for the MINI and the PDQ, which makes these patients vulnerable and susceptible of specific treatments.