Introduction
Mental disorders and addictive behaviors are becoming increasingly prevalent worldwide. They have clinical manifestations that vary according to the interaction of multiple genetic and environmental factors (McCrory & Mayes, 2015). Addiction to any type of substance is closely related to the presence of mental disorders and vice versa. Individuals with mental disorders are particularly vulnerable to using psychoactive substances and developing substance use disorders, compared to populations without these disorders (Reissner et al., 2012; Swendsen et al., 2010). Among those with severe addictive disorders, comorbidity with another mental illness is more common than expected (Reissner et al., 2012). In Iberoamerica, Szerman et al. (2013) have proposed the term dual disorders (DD) to refer to the coexistence of at least one addictive disorder with at least one other mental disorder (Casas, 2000).
The importance of the comorbidity of substance use disorders ‒SUD‒ with other psychiatric disorders has been evidenced in several studies due to its influence on clinical evaluation, evolution, and costs (Carey, Carey, & Meisler, 1991; Hunt, Bergen, & Bashir, 2002).
A number of epidemiological studies conducted mainly in the United States indicate that this comorbidity is very high, greater in subjects under treatment, and that the concomitant presence of several disorders has major clinical, evolutionary, and therapeutic implications (Compton, Thomas, Stinson, & Grant, 2007; Swendsen et al., 2010).Dual disorders have been associated with an increase in the number of psychiatric admissions (Hunt et al., 2002); violence (Soyka, 2000); suicidal behavior (Appleby et al., 1999), an increase in health expenditure (McCrone et al., 2000), greater medical comorbidity (Dickey, Normand, Weiss, Drake, & Azeni, 2002), poor adherence to treatment (Kamali et al., 2001), and limited results of the latter in both pathologies (Carey et al., 1991).
It has been pointed out that approximately 50% of individuals with psychiatric disorders will meet DSM-IV criteria for abuse/dependence on alcohol or intoxicants at some point in life (López-Ibor & Valdés, 2002; George & Krystal, 2000). Moreover, prevalence rates ranging from 25% to 80% have been found for SUD in psychiatric patients (Driessen, Veltrup, Wetterling, John, & Dilling, 1998; Margolese, Malchy, Negrete, Tempier, & Gill, 2004; Weaver et al., 2003). These ranges are so wide partly as a result of methodological aspects such as sample size, selection of subjects, criteria diagnosis, and the definition of SUD.
The dual disorders approach is complex and represents a major challenge as regards both diagnosis and pharmacological and psychotherapeutic treatment (Patel et al., 2015). It is therefore necessary to describe the association between the two pathologies in the methods used to treat mental illness in order to explain the associated factors and thereby improve the care of this type of patients.
Although there are a number of studies on DD in hospitalized psychiatric patients in the United States (Lehman, Myers, Corty, & Thompson, 1994); the United Kingdom (Barnaby, Drummond, McCloud, Burns, & Omu, 2003); France (Dervaux, Bayle, & Krebs, 2002); and Lebanon (Karam, Yabroudi, & Melhem, 2002), it is important to continue paying attention to dual disorders in this type of services in other cultural contexts.
We have limited data on the prevalence of DD in the population hospitalized for mental disorders in Colombia. Torres, Posada, Bareño, and Berbesí (2010); Peña-Salas, Bareño, Berbesí, and Gaviria (2014); and Castaño and Sierra (2016) have conducted studies on general populations, while Barrios-Ayola and Hurtado-Acosta (2012) have explored clinical populations. In Latin America, research on this topic has also been limited; authors such as Koldobsky (2010) in Argentina, Marín-Navarrete et al. (2015) in Mexico and Zegarra-Valdivia, Chino, and Cazorla (2016) in Peru have undertaken a number of studies. Knowledge about the distribution of dual disorders and the characteristics of those affected by them can help optimize and organize health resources.
The purpose of this study is therefore to explore the prevalence and sociodemographic and clinical factors associated with dual disorders in patients who were hospitalized for mental disorders in a general psychiatric hospital unit, a specialized center and a mental health service referral center in the public sector in Colombia.
Method
This is an observational, quantitative cross-sectional study of secondary sources (Álvarez-Hernández & Delgado-DelaMora, 2015).
Participants
The study included 224 clinical records of patients hospitalized for over 24 hours in a general psychiatric unit between January and June 2013, aged 18 to 65 years, diagnosed with a disorder related to drug or alcohol use (F10-F19), schizophrenia and other psychoses (F20-F29), mood disorders (F30-F39), neurosis and personality disorders (F40-F48/F60-F69), mental retardation (F70), or organic mental disorders (F00-F09) according to the ICD-10 diagnostic classification.
Sample size
Sample size was calculated using the formula for a proportion, with a confidence level of 1-α = 95%, an accuracy level of 5%, and a proportion of 45.7% (dual disorders prevalence of a pilot test performed on 50 clinical records of patients who had sought consultation in the past year prior to the study). The reference population (298) was approximately the average number of patients hospitalized in the past three years at a general psychiatric hospital in Colombia.
For a sample of 168 patients, and in order to control problems due to losses in the final sampling units, the sample size was adjusted, estimating a percentage of losses of 25%, and leaving a final sample of 224 patients.
Instruments
Information was obtained from the archive of physical and electronic medical records. The reports include treatment from general medicine, psychiatry, nursing, occupational therapy, psychology, and social work. Electronic medical records have compulsory standardized fields to ensure that the information is complete. As part of its quality standards, the hospital oversees the proper completion of medical records, thereby guaranteeing the quality of the data recorded.
The clinical history of a patient contains all the variables included in the study (sociodemographic variables, history of drug use and history of mental disorders, concomitant medical pathologies, treatment received for their mental or addictive disorder, and current diagnoses recorded in the clinical history according to ICD-10). Dual disorders was regarded as the presence of psychiatric diagnosis and a disorder related to drug or alcohol consumption according to the ICD-10 diagnostic classification, excluding tobacco (F10-F19), without specifying the substance involved. The diagnoses of mental disorders included schizophrenia and other psychoses (F20-F29), mood disorders (F30-F39), neurosis and personality disorders (F40-F48/F60-F69), mental retardation (F70), and organic mental disorders (F00-F09) (Bertolote & Sartorius, 1993). The support network and family functionality variables were recorded on the basis of the clinical history compiled by the social work department. At the center where the study was conducted, the social work department evaluated family functioning using the self-report scale FACES IV (Family Adaptability and Cohesion Evaluation Scales) to undertake the relational diagnosis (Ball, Tornaría, del Arca, & Olson, 2013; Olson, 2011) and the family APGAR, frequently recommended and used in Colombia (Cogollo, Gómez, de Arco, Ruíz, & Campo-Arias, 2009; Smilkstein, 1978), while also considering the support network as the patient’s perception of the help provided by his or her family and social environment at times of crisis. Minimum use of medical services was defined as attending at least eight of the 12 consultations scheduled for the year following discharge from hospital.
Variables included
The study made it possible to obtain variables grouped into sociodemographic and clinical factors, defined below, by group of factors:
Sociodemographic data: Age in completed years, recoded as age brackets (18 to 24, 25 to 34, 35 to 44, 45 to 54, and 55 or over), sex, marital status, schooling, social security, socioeconomic status, occupation (yes-no), support network (yes-no). Family dysfunction was defined according to the family APGAR score, “yes” being equivalent to less than 17 points, and “no” to between 18 and 20 points.
Clinical data: Number of days of first-time hospitalization recoded (less than a fortnight, a fortnight, or more), history of self-injury, history of hetero-aggression, medical illness, the main psychiatric diagnosis according to ICD-10 diagnostic classification, minimum use of medical services, number of consultations in the follow-up recoded by consultations in the follow-up with a cut-off point of four consultations, readmissions during the year after discharge, length of stay during rehospitalization recoded in a dichotomous manner (90 days or less, more than 90 days), family history of mental illness, and age of onset of mental illness in years.
Procedure
To obtain the information, medical records were compiled of patients aged 18 to 65 hospitalized in the psychiatric hospital center during the period from January to June 2013. After applying the inclusion and exclusion criteria, 201 clinical histories remained, from which the required data were drawn. These data were extracted from the reports from the general medicine, psychiatry, nursing, occupational therapy, psychology, and social work departments contained in the clinical history, for which an instrument for collecting information was designed. Subsequently, the database was constructed, which was analyzed using the statistical program SPSS version 22 (CES University License).
The quality of the data obtained is guaranteed by the implementation of the electronic medical record that requires filling in the data in compulsory standardized fields, in addition to the fact that since it is considered a legal document, every effort is made to ensure that it is properly completed. At the same time, the person who extracted the information is a specialist in psychiatry, which also guarantees the quality of the data obtained.
Statistical analyses
A descriptive analysis of the sample was carried out through the calculation of central tendency and dispersion measures according to the distribution of the quantitative variables; mean and deviation (normal variable), median and interquartile range (non-normal distribution) and absolute and relative frequencies for qualitative variables.
Qualitative variables were compared between dual and non-dual patients using the chi-square test or Fisher’s exact test when the frequencies observed at the crossing of variables were less than 5. For the only quantitative variable, the difference in medians was established using the Mann Whitney U test, since this variable did not have a normal distribution.
In order to explore the sociodemographic and clinical factors associated with dual disorders, we used the significant Pearson chi-square asymptotic test with p value < .05 (Manterola & Pineda, 2008), determining the odds ratio (OR) with its respect confidence interval of 95%. Taking into account the significantly associated sociodemographic and clinical variables in the bivariate analysis or those with probability values of < .25, the multivariate analysis was constructed with a logistic regression model, which makes it possible to control possible confounding variables, obtaining the adjusted or controlled OR for these probable variables. The logistic model is assumed to serve as a control for the confounding variables with the researchers’ criterion being used to determine the difference, and a change in the exponentials of the coefficients (OR) of over 10% (Gómez-Restrepo & Okuda-Benavides, 2006).
In order to determine the statistical power of the study, the power calculation was performed in the Epidat program using the rehospitalization factor, with a proportion of exposed cases of 59.5% and of unexposed cases of 37.3%, and a confidence level of 95%, for which a statistical power of 81.9% was reported.
Ethical considerations
This study was approved by the Research Ethics Committee of the psychiatric hospital where the study was conducted, and described as minimal risk since the data were obtained from a secondary source.
Results
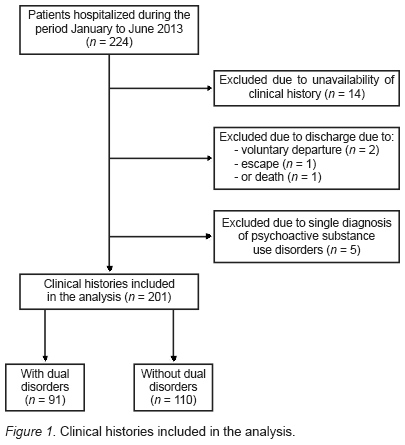
Of the 224 clinical records selected, 201 clinical histories were included. In the analyses, 23 records were excluded for a variety of reasons (the medical record was unavailable, the patient had been discharged from hospital due to voluntary departure, escape or death, or s/he had a single diagnosis of psychoactive substance use disorder) (Figure 1).
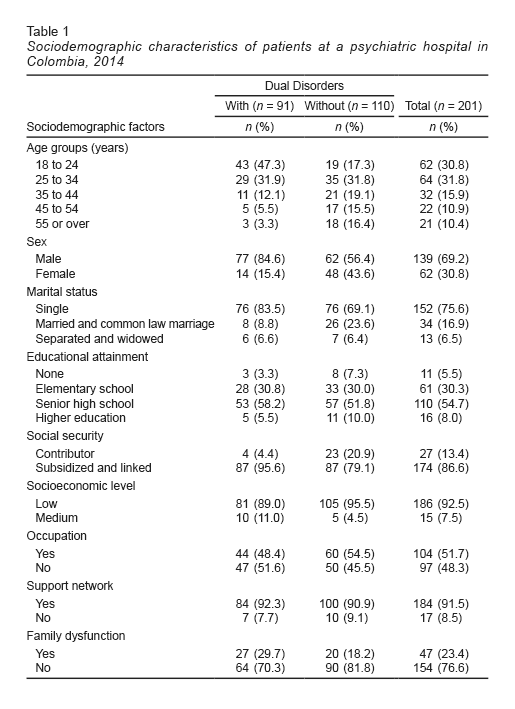
Of the patients analyzed, 45.3% had dual disorders (DD). Of all the patients who were part of the study, there was a male-female ratio of 2.24:1. The majority were single and over 90% had low socioeconomic status. A total of 62.6% of the patients were aged between 18 and 34 and over half had completed high school. With regard to support networks, according to their clinical history, most of them reported having a support network while over three quarters had proper family functionality according to the family APGAR.
For the group with DD, there was a predominance in the age group of those aged between 18 and 24; the predominant sex was male, with 84.6%; 89% had completed elementary or middle school studies, and had good support networks and no family dysfunction. Over half were unemployed (Table 1).
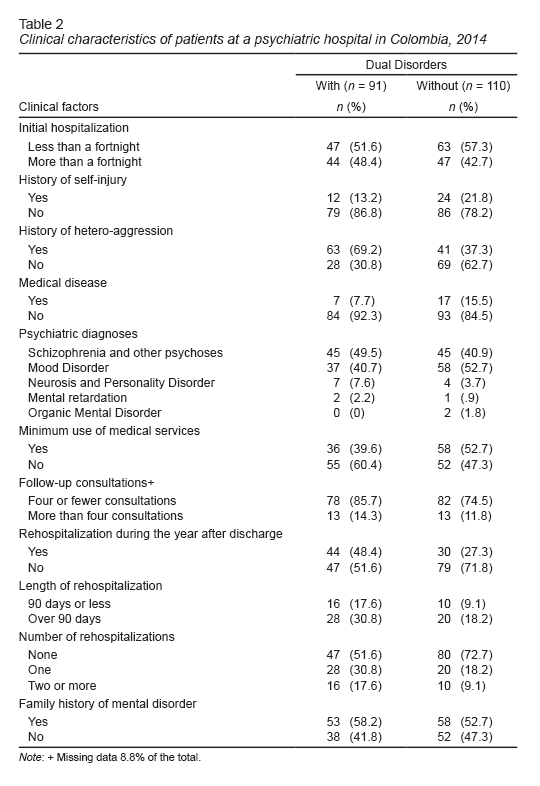
First-time hospitalization of over a fortnight was more common in patients with DD (48.4% vs. 42.7%); there was a history of increased self-harm in the group without dual disorders (21.8% vs. 13.2%); a history of greater heteroaggression in the group with DD (69.2% vs. 37.3%); a higher presence of concomitant medical disease in patients without DD (15.5% vs. 7.7%); minimum use of medical services, defined as attending eight consultations or more out of the 12 a year scheduled after follow-up, was greater in the group without DD (52.7% vs. 39.6%); the number of rehospitalizations during the year after discharge was higher in patients with DD (48.4% vs. 27.3%); the number of days spent at hospital during rehospitalization was over 90 in the DD group (30.8% vs. 18.2%); the number of readmissions was higher in patients with DD (17.6% vs. 9.1%) while a family history of major mental illness was more common in the group of patients with DD (58.2% vs. 52.7%).
The most frequent mental disorders in patients with DD were: schizophrenia and other psychoses (49.5% vs. 40.9%); neurosis and personality disorders (7.6% vs. 3.7%); mental retardation (2.2% vs. .9%). The most frequent mental disorders in the group without DD were mood disorders (52.7% vs. 40.7%) and organic mental syndromes (1.8% vs. .0%) (Table 2).
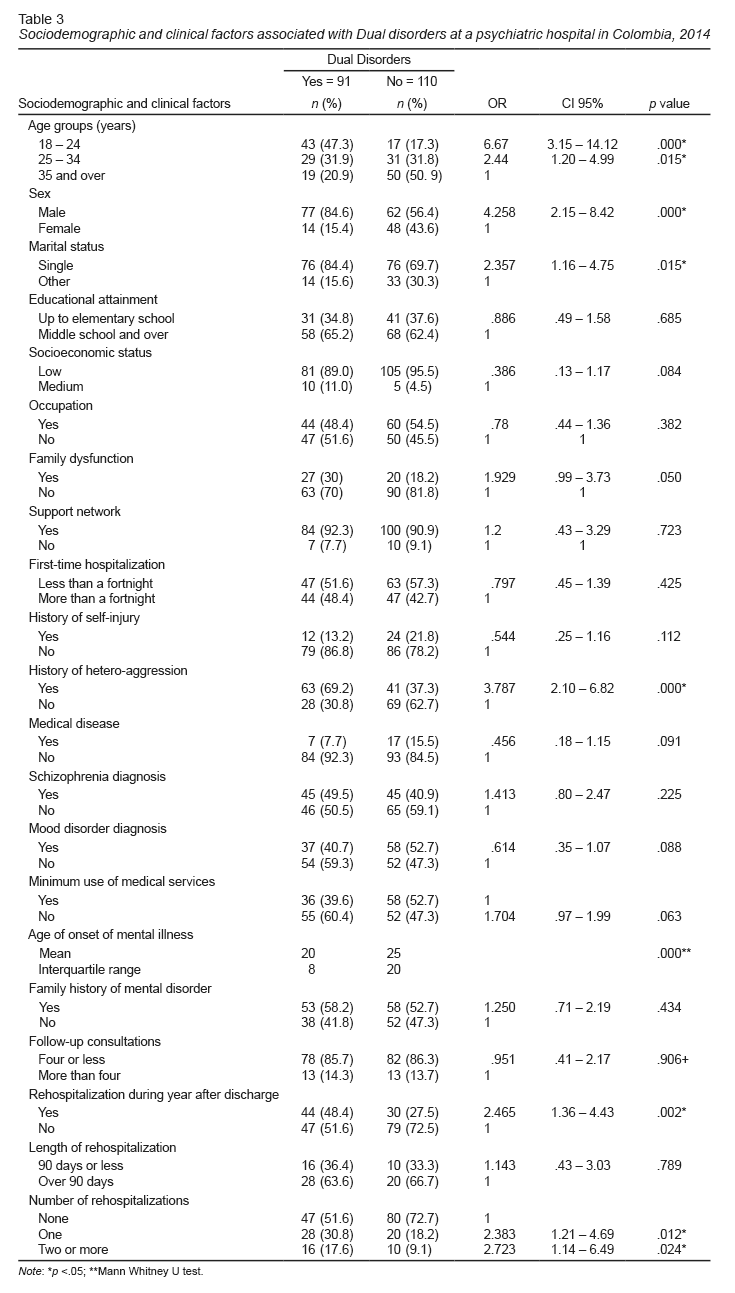
A bivariate analysis of the group of patients with dual disorders found significant statistical associations with the sociodemographic variables in the groups aged 18 to 34, which was higher in the younger group aged 18 to 24 (OR = 6.67, 95% CI [3.15, 14.12], p < .000). As for sex, single men showed the greatest association (male sex OR = 4.26, 95% CI [2.15, 8.42], p < .000 as did single marital status, OR = 2.35, 95% CI [1.16, 4.75], p = .015).
Clinical variables with the greatest statistical significance in the DD group were having a history of hetero-agression (OR = 3.78, 95% CI [2.10, 6.82], p < .001), having been rehospitalized during the year after discharge (OR = 2.46, 95% CI [1.36, 4.43], p = .002), and having had two or more readmissions (OR = 2.72, 95% CI [1.14, 6.49], p < .024). Another variable analyzed was the age of onset of mental illness, where there were significant differences between their medians with p < .000 value, with those in the group with DD being younger (Table 3).
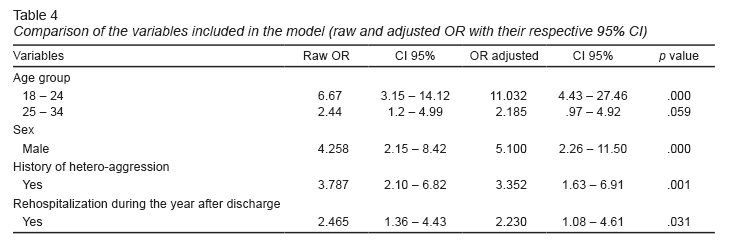
After entering all the variables that were significant with a value of p < .05 and those with a value of p < .25 in the bivariate analysis, the logistic regression model was adjusted with the Nagelkerke R2 of 41.2%, the variability explained in the dual disorders by the variables included in the model.
Variables that were statistically significant with a value of p < .05 in the bivariate analysis, with the exception of the number of rehospitalizations, continued to be significant in the multivariate model. In order of importance, these included being aged 18 to 34 with an OR = 6.67 to an aOR = 11.03 (95% CI [4.43, 27.46]), being male with an OR = 4.26 to an aOR = 5.10, (CI 95% [2.26, 11.50]), previous history of hetero-aggression with an OR = 3.79 to an aOR = 3.35 (95% CI [1.63, 6.91]), and rehospitalization during the year after discharge with an OR = 2.46 to an aOR = 2.23 (95% CI [1.08, 4.61]) (Table 4).
Discussion and conclusion
Most studies on dual disorders conducted on the population with mental disorders have consistently confirmed the high comorbidity of SUD and psychiatric illness in both ambulatory and hospitalized patients. Although most studies conducted analyze the comorbidity of SUD with severe disorders from axis I of DSM-IV, especially with psychotic disorders and depressive/bipolar disorders, studies have also been conducted with other pathologies from axis I (Otto, Pollack, Sachs, O’Neil, & Rosenbaum, 1992) and axis II (Dulit, Fyer, Haas, Sullivan, & Frances, 1990).
Studies conducted on the hospitalized population with mental disorders have shown that the prevalence of concurrent SUD is between 12% and 60% (Barnaby et al., 2003; Brady, Casto, Lydiard, Malcolm, & Arana, 1991; Margolese et al., 2004).These lifetime prevalences of SUD are higher than those of the general population, which range from 15% to 20% (Regier et al., 1990).
The finding in this study of a prevalence of 45.3% of DD is within the range found by some authors (Cantwell et al., 1999; Margolese et al., 2004), although it should be noted that other studies report lower prevalences. For example, Brady et al. (1991) found that 29 out of 100 patients admited to a psychiatric unit for acute cases met the DSM-III-R criteria for SUD in the 30 days prior to their admission. Likewise, in a sample of patients admitted to two psychiatric hospitals in London, Barnaby et al. (2003) found that 22% had alcohol dependence and that 27% had used drugs in the previous 30 days. At the same time, Barrios-Ayola and Hurtado-Acosta (2012) report a prevalence of 19.5% in a sample obtained from three psychiatric institutions in two cities in Colombia. The discrepancies between the results obtained in this paper and previous studies may be due to the place where study subjects are recruited. Our study was conducted at a general psychiatric hospital that admits both acute and chronic patients, the latter being those that most often present dual disorders, hence its high prevalence.
Lastly, Zegarra-Valdivia, Chino, and Cazorla (2016) report a prevalence of 49% at a specialized psychiatric center in Arequipa, Peru, which is similar to our findings, as is the type of hospital unit where the study was conducted.
Regarding the sociodemographic and clinical characteristics of the sample, it was observed that there was a higher proportion of young male patients, with a predominance of single males, in the DD group. In addition to our findings, the predominance of males has also been pointed out by other authors (Cantor-Graae, Nordström, & McNeil, 2001; Mueser et al., 2000), together with a greater frequency of single men (Drake & Mueser, 2000). Accordingly, it has been said that the condition of being a man or a woman influences the prevalence of psychiatric diseases, pathoplasty, symptom expression, course, prognosis, demand and response to treatment. In this regard, recent decades have seen growing interest in the influence of gender on mental illness and SUDs. Most studies have evaluated sex differences in samples from patients with mental pathology and SUD separately, with few studies being conducted on patients with dual disorders. So far there are discrepant data due to the variability of the results that could be related to the heterogeneity of the studied populations, the diagnostic tools and the evaluation of use, and the psychopathological state of the subjects. Although it is believed that men can more frequently present a comorbid addictive disorder in conjunction with another mental illness, it is considered that women are at greater risk for developing both pathologies (Miquel, Roncero, López-Ortiz, & Casas, 2011).
Conversely, Rodríguez et al. (2008) report that in general psychiatric units there are more dual men than women. However, when samples of patients are studied in detoxification units or in the ambulatory follow-up of addictions, the ratio is reversed, with a higher percentage of dual disorders being observed in women than men, with mood, anxiety and mood disorders, eating behavior disorders, together with the use of alcohol, tobacco, and cannabis being more frequent (Marín-Navarrete et al., 2015; Miquel et al., 2011).
With respect to the longer average length of hospital stays obtained in the DD group found in this study, this has also been observed in other studies (Swindle, Phibbs, Paradise, Recine, & Moos, 1995), although other authors have noted the opposite (Farris et al., 2003). This longer average stay can be partly explained by the fact that patients with dual disorder evolve worse during treatment (Casas et al., 2008), and also because it has been suggested that dual patients in the mental health network have more severe psychopathology (Primm et al., 2000).
Rehospitalizations and the extent to which they occur are also more frequent in the DD group, which tallies with the findings of Woody (1996), who mentions longer, more frequent hospitalizations in this type of patients, and those of Hintz & Mann (2005), who note that comorbidity leads to an increase in relapses in both the disease and drug use, an inability to adhere to treatment programs and a greater number of hospitalizations and long-term costs.
On the other hand, although a higher prevalence of dual disorders in patients with low socioeconomic status and low educational achievement has been noted, no significant differences were found in this study in relation to these variables. This discrepancy may be due to the fact that in the sample in this study, both the DD and the group with mental disorders and without DD (MD group) have medium/low socio-economic status and have completed minimum compulsory schooling (elementary and middle school education) due to the context where this research was undertaken ‒Colombia‒ (Jiménez-Castro, Raventós-Vorst, & Escamilla, 2011).
Likewise, the socioeconomic sedimentation constitutes a bias that prevents the emergence of possible differences in this variable.
Regarding the psychiatric diagnosis present in patients with dual disorders, the predominance of schizophrenia and other psychoses is striking, reaching prevalences of 49.5% compared to 40.9% of patients in the group with mental disorders. This data is comparable with the studies conducted by Fenton (2001), Margolese et al. (2004), and Rodríguez et al. (2008) describing the close association between drug use and psychiatric disorders.
With respect to other mental disorders present in patients with dual disorders, this study found that neurosis and personality disorders were higher in this type of patients (7.6% vs. 3.7%); while mood disorders were more frequent in the group without DD (52.7% vs. 40.7%). Not all studies agree on this point, with anxiety disorders being those with the greatest frequency (65%) followed by affective disorders (33%) and antisocial personality disorder (28%) (Tómasson & Vaglum, 1995). In Spain, affective disorders were the most common type of disorder in drug-dependent patients (21.6%), followed by anxiety disorders (11.7%) and schizophrenia (3.1%) (Gual, 2007). Conversely, DiNitto, Webb, and Rubin (2002) and Sanabria, Díaz, Varela, and Braña (2002) have also reported that in patients diagnosed with SUD, affective disorders were the most prevalent psychiatric disorder (DiNitto et al, 2002; Sanabria et al., 2002).
In relation to family history, it is striking that no significant differences were found between both groups in relation to a higher prevalence of family history of mental disorders (MD) in the DD group. A higher prevalence has been observed in certain studies (Comtois, Tisdall, Holdcraft, & Simpson, 2005), suggesting that MD contain a significant family component (biological and/or psychosocial) not only among the general population but also among the clinical population with drug use disorders (McGrath, 2000).
Our study also found a greater statistical association with heteroaggression in patients with dual disorders, which has also been reported by other authors (Mueser et al., 2009; Pereiro et al., 2013).
Although self-harm has also been described in this group of patients, this association was not found in the present study.
Lastly, this study found that the median age of onset of mental illness is lower in the DD group (20 vs. 25), with a statistically significant association mentioned by other authors (Brown, 2005; Levin & Hennessy, 2004), which could support the hypothesis of common vulnerability, where genetic or neurobiological factors or childhood disorders contribute to the emergence of both disorders.
The results of this research, in which significant prevalences of dual disorders of 45.3% were detected in the clinical population of a general psychiatric hospital in the city of Medellín, support the need for major efforts to implement specific strategies and resources for the management of dual disorders in Colombia. They also call for the promotion of proper human resource training and the provision of comprehensive care services, since care for this type of patients in this country has been organized under the parallel or sequential model. This has been associated, as has already happened in other parts of the world, with low treatment adherence, inadequate management of the most frequent problems related to this comorbidity and an increase in healthcare costs (Arias et al., 2013; Pettinati, O’Brien, & Dundon, 2013; Szerman et al., 2013). Accordingly, the implementation of specific integrated services and resources for patients with dual disorders poses a major challenge for health professionals and managers.
Limitations of this study include the fact that it is a retrospective study involving the review of medical records, with the inherent biases of this type of article. In general, clinical diagnostic criteria were used, with only standardized measurement instruments habitually employed in everyday treatment being utilized. We also consider that the figure obtained for the prevalence of dual disorders in patients hospitalized in a mental health unit is striking and underlines the importance of the problem. However, since the data were drawn from clinical histories and retrospectively, figures may have been underestimated (Weaver et al., 2003).
The size of the sample that included individuals was between the ages of 18 and 65 years is another limitation of the study. It is a well known fact that in groups ages 14 and 18 years, the prevalences of dual disorders is high (Giaconia, Reinherz, Paradis, & Stashwick, 2003). This may mean that a significant number of patients of these ages, who were hospitalized at this treatment center during the period when the data were obtained, were excluded.
On the other hand, the fact that the population served has a predominantly medium-low socioeconomic status means that it would be advisable to repeat this study in population samples from different socioeconomic strata.
By way of a conclusion, this study is important for Colombia since the prevalence of dual disorders observed is much higher than in other studies. Castaño and Sierra (2016) found prevalences of 7.2% in the general population; Peña-Salas et al. (2014) found a prevalence of 5.9% of alcohol dependence and a prevalence of 7.8% of abuse in a group of patients with social phobia, whereas Barrios-Ayola and Hurtado-Acosta (2012) reported a prevalence of 19.5% in a sample collected at three psychiatric institutions in two cities in Colombia. These differences may be due to the different population groups where the studies were carried out, the centers from which the samples were taken, and the mental and drug use disorders included, which should prompt further research on the characteristics of these comorbidities in general populations and clinics, in order to develop appropriate intervention proposals for local socio-cultural and demographic contexts.