Introduction
Attention deficit hyperactivity disorder (ADHD) was recently incorporated into the neurodevelopmental disorder category. It is considered one of the main reasons for mental health consultation in children and adolescents (Biederman, 2005; Langley et al., 2010; Polanczyk et al., 2008). Epidemiological studies indicate that approximately 5.29% of the general population at any stage of life has this disorder (Polanczyk, de Lima, Horta, Biederman, & Rohde, 2007). The sex ratio distribution for men and women varies. In community samples, it has a 2 to 1 distribution and in clinical samples a larger difference is observed with a 9 to 1 distribution, with men appearing to be more affected in both cases (Biederman & Faraone, 2005; Polanczyk et al., 2007; Polanczyk & Rohde, 2007). The National Comorbidity Survey Replication (NCR-R) conducted in the United States (Kessler et al., 2006) showed that, in adults, the presence of ADHD is a marker of poor prognosis for the presence of comorbidity and from an earlier age of onset.
In the middle of the last century, studies on this disorder focused on the child population, since it was assumed that ADHD did not manifest in adulthood (Ramos-Quiroga et al., 2006). This perspective has gradually changed, and it is currently thought that a significant proportion of children affected by this disorder persist into adult life and have associated impairment during adulthood (Barkley, 2008; Biederman, 1998; Biederman et al., 1996; Matte, Rohde, & Grevet, 2012). Both the DSM-5 and the International Classification of Diseases 11th revision (ICD 11) have tried to capture the clearest clinical presentation of ADHD in adults in various contexts, mainly the clinical one (Faraone et al., 2006; Kessler et al., 2010; Matte et al., 2012).
Recent reports by longitudinal studies indicate that although ADHD persists into adulthood, it has not been observed in the expected proportion, Moffit et al. (2015) recently noted that 90% of adult ADHD cases lacked a history of childhood ADHD. Thus, ADHD may display different trajectories in its clinical presentation (Agnew-Blais et al., 2016; Asherson, Buitelaar, Faraone, & Rohde, 2016; Caye et al., 2016; Matte et al., 2012; Moffitt et al., 2015). The symptomatic expression of ADHD, including adulthood onset ADHD, depends on the context, in other words, the interaction between biological aspects such as neurocognitive resources and environmental aspects such as the familial, interpersonal, academic and work spheres in which the affected subjects develop (Lasser, Goodman, & Asherson, 2012). Other factors such as sex, age at the time of evaluation, differences in definitions of impairment or context (e. g., urban vs. sub-urban, traditional vs. non-traditional school, etc.) are known to influence the presentation of ADHD.
Nevertheless, scientific evidence published in recent years on adults with ADHD, highlights the lack of its recognition among mental health care professionals, probably associated with difficulties in its understanding and conceptualization. Errors and omissions in ADHD often prevent those affected from receiving timely and effective treatments for their condition, which ultimately leads to unnecessary health and general life consequences (Kooij et al., 2010).
Although there is scientific information about adults with ADHD in a clinical context of developing countries, as in the case of Mexico (Almeida et al., 2006; Fayyad et al., 2007”; Lara et al., 2009), we know very little about the implications of having ADHD in a Latin American clinical sample, or the relationship between executive functioning and ADHD in adulthood. It is for this reason that we decided to study a sample of adults in a clinical context who have ADHD compared with non-ADHD adults.
Method
Once the project had been approved by the corresponding scientific and ethics committees of the Instituto Nacional de Psiquiatría Ramón de la Fuente Muñiz (INPRFM), and after informed consent had been obtained, the sample included male and female adults ages 20 to 45, who voluntarily requested psychiatric medical care at the INPRFM. Participants were invited to the Clinical Research Program on lifetime ADHD (PROMETEO), a clinical research and human resource training initiative implemented since 2007, if they had less than one week of treatment and could read and write, so that they could be interviewed and complete the clinimetric instruments. All the subjects who completed the evaluations were included.
This clinical research program evaluation process was carried out in three stages, after respondents had answered the short, six-item version of the Adult Self Reported Scale ASRS V1.1. If they displayed at least three of the six positive items (Adler et al., 2006) or had a score of over 10 points (Ramos-Quiroga et al., 2009), they were invited to participate in the first stage of this clinical program. During this stage, diagnosis was confirmed by a clinician with at least five years’ experience using the Spanish version of Kiddie Schedule for Affective Disorders and Schizophrenia present and lifetime (K- SADS- PL) with DSM-IV criteria. Comorbid disorders were then evaluated in a second stage through the MINI International Neuropsychiatric Interview (M.I.N.I.). In addition to the interview, symptom severity was obtained from the ASRS-V1.1, 18-item version and executive functions were assessed through the Behavior Rating Inventory of Executive Function (BRIEF) self-reported version. As part of the second stage, difficulties in performance or the effects on the various areas of the individual, were evaluated by a questionnaire specifically developed for our clinical research program called the Sociodemographic and Clinical Questionnaire for Adults with Attention Deficit/Hyperactivity Disorder (SCQA-ADHD). Finally, in the third stage, each individual case was reviewed by a clinician with at least 15 years’ experience (L.P.C.) in ADHD diagnosis and comorbidities. After the full evaluation (the three stages previously described), patients who met the DSM-IV criteria for ADHD were categorically considered cases, while those who did not were considered non-cases. Non-cases may have any disorder but not ADHD.
Interviews and clinimetric instruments
ADHD Self-reported Rating Scale (ASRS-V1.1)
This self-report screening questionnaire, developed by the World Health Organization (WHO), is widely used (Kessler et al., 2005; Reyes et al., 2009) to identify ADHD symptoms in adults. This questionnaire was developed from the Composite International Diagnostic Interview (CIDI) (Adler et al., 2006) and is available in two versions. The long version consists of 18 questions corresponding to the DSM-IV criteria, which are related to the common manifestations of ADHD in adults. The short version includes the first six questions (section A), which constitute the most predictive symptoms of ADHD (Kessler et al., 2005).
Section A of the ASRS has shown that it has a better psychometric behavior than the 18-item version in terms of sensitivity (68.7% vs. 56.3%), specificity (99.5% vs. 98.3%), accuracy in diagnostic classification (97.9% vs. 96.2%) and clinical concordance with the diagnostic standard (Kappa, .76 vs. .58). The test-retest reliability of the full scale showed a Pearson Coefficient greater than .80 (Kessler et al., 2005). The Spanish version of the scale, which differs from the original method of rating with the template, establishes that the diagnostic threshold using section A alone establishes a cut-off point of 12 points, obtaining a sensitivity of 96.7%, a specificity of 91.1%, a positive predictive value of 91.6%, a negative predictive value of 96.5%, a Kappa index of .88 and an area under the curve of .94 (OR = 297.3; 95% CI[76.2, 1.159]). This provides further evidence of the advantages of section A of the ASRS as a useful tool for adult screening in a clinical context. Finally, ASRS V1.1 has proved its psychometric properties in various cultures with different cut-off points (Aragonès, Cañisá, Caballero, & Piñol-Moreso, 2013; Kessler et al., 2007; Ramos-Quiroga et al., 2009; Yeh, Gau, Kessler, & Wu, 2008).
Schedule for Affective Disorders and Schizophrenia for School Aged Children Present and Lifetime DSM-IV/Spanish version (Kiddie SADS PL)
The K-SADS-PL interview is a semi-structured, diagnostic interview based on the diagnostic criteria of the DSM -III_R and DSM-IV, which is useful for the cross-sectional and longitudinal clinical assessment of the onset of psychopathology in childhood and adolescence. The Spanish version of the K-SADS-PL has been adapted and validated in the clinical population (Ulloa et al., 2006). The inter-rater reliability study showed that the Kappa coefficients were maintained within the range of good to excellent for the current and lifetime mental health disorders evaluated, especially for ADHD; the Kappa coefficient obtained was .91. For our study, the K-SADS-PL was only used to increase the diagnostic accuracy of ADHD, and was determined as the diagnostic standard in our sample of respondents.
Sociodemographic and Clinical Questionnaire for Adults with Attention Deficit/ Hyperactivity Disorder (SCQA-ADHD)
In order to obtain information that could help us determine the difficulties in performance in various areas of the individual, a questionnaire was specifically designed for our study. The SCQA is a self-report questionnaire specifically designed by researchers in this program (SOL, AJM, PMV, and LPC) for our research program comprising 71 binary questions developed on the basis of scientific evidence, which includes different aspects related to: a) Academic area, b) Working area, c) Risk Behaviors area, d) Social area, e) Economic area, f) Mental health area, and g) Self/-perception. Each of the items in this questionnaire was framed as a Yes/No question.
International Neuropsychiatric Interview for adults, plus version (MINI-plus)
The MINI-plus interview is the long version of the structured psychiatric diagnostic clinical interview for subjects over 18, jointly developed and validated in the United States and Europe for psychiatric disorders included in the fourth version of the diagnostic and statistical manual (DSM-IV) and the tenth international classification of diseases ICD-10 (Sheehan et al., 1997). This interview includes 23 diagnoses, and provides diagnostic exclusion questions, to sub-typify disorders, locate them chronologically by investigating the age of onset, thereby allowing hierarchical exclusions in the event that a patient has more than one disorder over time. For this research, this interview was used to determine comorbidity with the main mental health disorders of all the subjects in the clinical sample (Kumar, Faden, & Steer, 2011).
Inventory of behavioral evaluation of the Executive Functions (BRIEF self-reported version)
This instrument, designed by Gioia, Isquith, Guy, and Kenworthy (2000), evaluates executive performance in various areas (inhibition, shifting, emotional control, initiation, working memory, planning and organization, self-monitoring, organization of materials and task-monitoring) which presents with a reliability of .91 (Jarratt, Riccio, & Siekierski, 2005). It has two versions, a self-applicable one and one to be completed by an observer, preferably a close relative or a person living with the patient. The adult version contains 75 items and takes approximately 10 minutes to complete. For this study, we decided to use the self-applied version (BRIEF-A), due to its greater availability. The instrument is designed on the basis of a Likert scale, which yields raw scores that are subsequently converted to T scores. In this report we considered as a T score ≤ 65 as the cutoff point. This instrument ranks the result by showing the global score, called the composite global executive index (GEC), which comprises the sum of the scores of two sub-indices called Behavioral Regulation Index (BRI), and Metacognitive Index (MI). The BRI consists of four clinical scales called inhibition, shifting, emotional control and self-monitoring while the MI comprises five scales: starting an activity- initiating-, working memory, planning and organization, task monitoring, and organization of materials. This instrument has shown adequate validity and reliability. The BRIEF has been used in other countries for the concurrent validation of instruments that measure executive function such as the FLEC scale (The Frontal Lobe / Executive Control Scale) and the set of instruments called BASC (Behavior Assessment System for Children [Parent Rating Scales]) (Sullivan & Riccio, 2006). Lastly, its clinical utility in the evaluation of executive functions has been demonstrated in individuals with a range of health conditions in various age groups (Ciszewski, Francis, Mendella, Bissada, & Tasca, 2014; Cummings, Singer, Krieger, Miller, & Mahone, 2002; Mahone, Cirino, et al., 2002; Mahone, Zabel, Levey, Verda, & Kinsman, 2002; Shear, del Bello, Lee, Rosenberg, & Strakowski, 2002).
Statistical analysis
Initially, the values lost for each variable were replaced through the simple imputation method (Papageorgiou, Grant, Takkenberg, & Mokhles, 2018), provided the maximum value lost was 15% for each given variable. No variable amounted to 10% of lost values. Once the previous step had been completed, the distribution of the data was evaluated through the Kolmogorov-Smirnov test. We considered distribution to be normal when the p value was > .05 (Wallot & Leonardi, 2018).
In keeping with the objectives of our study, for the univariate or descriptive analysis of the categorical variables of the study such as sociodemographic variables, comorbid mental disorders, executive functions, psychosocial functioning, proportions and frequency distributions were used. For the bivariate analysis, in the case of the categorical variables, χ2 and Fisher’s exact tests were used through 2x2 tables and for the continuous variables, student T tests were used for independent samples. Unadjusted odds ratios (OR) and their 95% confidence interval (CI) was calculated. The diagnostic status of ADHD was determined as an independent variable. The main dependent variables were the symptomatology and clinical manifestations associated with ADHD, comorbid psychiatric disorders established according to DSM-IV, difficulties in various areas of functioning of adults and difficulties in executive functions according to BRIEF, p value < .05 was considered statistically significant. We used the SPSS program version 19.
Results
Demographic and clinical characteristics of the study sample
The study sample included 151 subjects, 54.6% (n = 82) of whom had ADHD. Nearly 66% of the overall sample were women, with a mean age of 29.7 years (SD 6.6 years), who also had a mean of two psychiatric disorders (SD 1.2).
Demographic and clinical characteristics of adults with and without ADHD
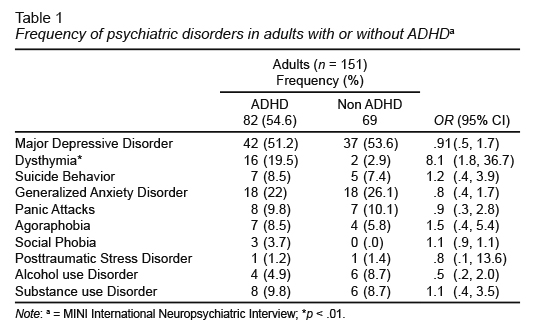
There were no differences in the proportion of women with and without ADHD (70.7% vs. 59.4% respectively, OR = .6; 95% CI[.3, 1.2]; p = .146). The average age in the group with ADHD was significantly lower than that of those who did not present with the diagnosis (28.1 SD 6.1 vs. 31 SD 7, respectively). Within the group with ADHD, 79.3% (n = 65) had at least one comorbid disorder. The average number of comorbid disorders was significantly higher in the group of adults with ADHD compared to the group without the disorder (2.5 SD 1.1 vs. 1.3 SD 1.0 respectively; F = .439; t = -6.621; gl = 149; p < .001). Only dysthymia had a significantly higher frequency in subjects with ADHD compared with those who did not have it (19.5% vs 2.9%, OR = 8.1; 95% CI[1.8, 36.7]) (Table 1).
Report of associated symptoms in adults with and without ADHD
When using the MINI Interview-ADHD Module to distinguish between clinical manifestations in childhood and adulthood, we only found that adults with ADHD reported having more difficulties in emotional regulation during their childhood (67.1% vs. 49.3% respectively, OR = 2.1;95% CI[1.1, 4.1]), which was no longer statistically significant in adulthood (89.0% vs. 79.7% respectively, OR = 2.1; 95% CI[.8, 5.1]) and behavioral problems (54.9% vs. 31.9% respectively, OR = 2.6; 95% CI[1.3, 5.1]). Specifically, in the data reported in adult life, we found that subjects with ADHD changed jobs more frequently than those without the disorder (45.1% vs. 29.0% respectively, OR = 2.0; 95% CI[1.0 to 4.0]). The remainder of the information showed no significant differences between groups.
Report on difficulties in various areas of psychosocial functioning between adults with and without ADHD
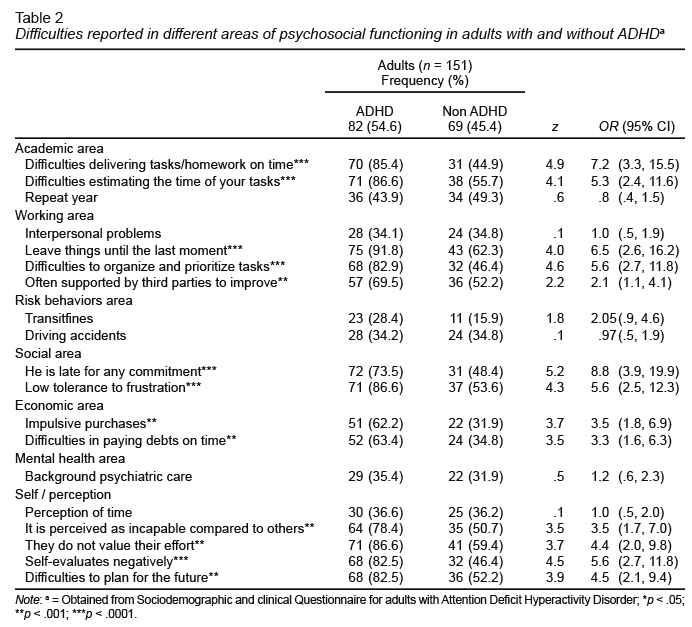
When comparing both groups in the report on difficulties in functioning in different psychosocial spheres (Table 2), we found that adults with ADHD had more difficulties in the workplace. Subjects with ADHD procrastinated more in different activities of their daily lives, had more difficulties organizing their lives and problems managing time and their finances. Finally, in aspects that may affect their performance in daily life, adults with ADHD reported difficulties planning their future and negative self-evaluation more frequently.
Perceived executive functioning among adults with and without ADHD
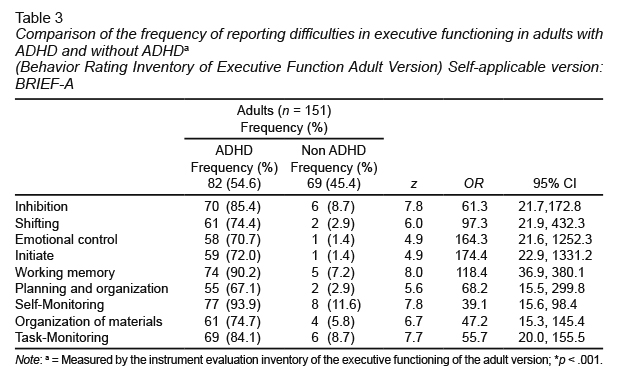
Regarding executive functions evaluated through the BRIEF self-report questionnaire, we found that the group of adults with ADHD had a higher level of executive dysfunction compared to those without the disorder (Table 3). Moreover, adults in the ADHD group reported more difficulties in the behavior regulation index (86.6% vs. 5.8% respectively, OR = 104.9; 95% CI[31.8, 345.7]; z = 7.65) and the metacognitive index (85.4% vs. 5.8% respectively, OR = 94.79; 95% CI[29.10, 308.76]; z = 7.56) than those without ADHD. As expected, a difference was also observed in the global executive functioning index between groups (87.8% vs. 4.3% respectively, OR = 158.40; 95% CI[1.78, 600.57]; z = 7.45).
Discussion and conclusion
This research allowed us to describe the clinical and neurocognitive characteristics of an adult sample with and without ADHD. In line with previous research, we found no differences in ADHD diagnosis between men and women (Agnew-Blais et al., 2016; Moffitt et al., 2015). A recent report by Ahnemark et al. (2018) on a Swedish adult population with a recent diagnosis of ADHD, indicated that 57% of the sample was female. Our finding sheds light on the fact that regardless of gender, people have the same risk of developing ADHD. Moreover, many studies (Caye et al., 2016; Moffitt et al., 2015) reported that in adulthood, the ratio of sex distribution observed in those with childhood onset, changes to a higher ratio for women with this disorder, although this does not mean that being a female is a risk factor for persistence (Caye et al., 2016).
It has been demonstrated that having ADHD throughout life has a negative impact on general health and mental health. It is a risk factor for presenting with other comorbid disorders in mental health (Kessler et al., 2006; Nierenberg et al., 2005) and diseases (Cortese et al., 2016; Liao, Lien, Wang, Huang, & Chen, 2016), even at an earlier age (Dunne, Hearn, Rose, & Latimer, 2014; Meinzer et al., 2013; Nierenberg et al., 2005). In our ADHD group, more than three quarters of the study sample had at least one comorbidity; and a higher average of comorbid disorders than those without ADHD. In this regard, in a study published by Polyzoi, Ahnemark, Medin, and Ginsberg(2018), based on the Swedish national register of patients, 52.6% of adults with ADHD had at least one comorbidity, mainly anxiety disorders, substance use disorders and affective disorders. Our findings support the scientific evidence that having ADHD is related to more severe clinical symptoms than in those who do not have the diagnosis (Barkley & Brown, 2008; Nierenberg et al., 2005).
When they suspect ADHD, mental health professionals must consider that the clinical expression of adult symptoms can be modified by the environment in such a way that the patient must be analyzed on the basis of the context in which s/he develops. In this respect, ADHD models, including DSM-5 (American Psychiatric Association, 2013; Steinhausen, 2009), a) describe hyperactivity as a ubiquitous/ universal behavior, b) predict that hyperactivity decreases throughout development, and inattention persists’ or c) differentiate between subtypes/ presentations according to perceived differences in hyperactive behavior or inattention. However, recent scientific data indicates that both hyperactivity/impulsivity and inattention in subjects with ADHD can be significantly influenced by environmental factors and cognitive/ executive functioning demands (Kofler, Raiker, Sarver, Wells, & Soto, 2016).
Since the current DSM-5 diagnostic criteria for ADHD is based on findings from the pediatric population (Applegate et al., 1997; Lahey et al., 1994), proper diagnostic criteria for adults is essential. The growing scientific evidence reported in recent decades has contributed to the concept and understanding of ADHD, which is at a stage of theoretical rethinking, from the initial notion of a specific form of brain dysfunction to a concept that includes variables such as neurodevelopment, a concept which involves the evaluation of symptoms throughout life (Almeida et al., 2013; Shaw, Gogtay, & Rapoport, 2010; Shaw et al., 2013), gene-environment interaction (Steinhausen, 2009), consideration of age of onset (Agnew-Blais et al., 2016; Moffitt et al., 2015), and clinical aspects. All of these leads us to consider that ADHD is a heterogeneous group of related phenotypic expressions (Taylor, 2009).
In our study, adults with ADHD reported difficulties in emotional regulation in childhood, and nine out of ten persisted with this problem in adulthood. There is currently a discussion about whether this psychopathological characteristic should be part of the clinical description of ADHD (Retz, Stieglitz, Corbisiero, Retz-Junginger, & Rosler, 2012) in children and adolescents as well as adults. Several empirical studies have confirmed a high prevalence of emotional dysregulation in adults, coupled with a reported frequency of central symptoms of inattention, hyperactivity, and impulsivity (Hirsch, Chavanon, Riechmann, & Christiansen, 2018).
Adults with ADHD versus those without ADHD have more difficulties in different areas of functioning. This finding adds to the accumulated scientific evidence on the clear relationship between ADHD and executive functioning (Antshel et al., 2010; Nigg et al., 2005; Seidman, 2006; Stavro, Ettenhofer, & Nigg, 2007). Adults with persistent symptoms reported more difficulties related with to executive functions, involving controlled attention, rather than hyperactivity and impulsivity symptoms (Barkley, 2008). Deficits in executive control that appear in the early stages of life of subjects with ADHD tend to persist into adulthood and are consistent with the reports of both the patient and informants, with respect to the behavioral manifestations of executive dysfunctions in everyday life (Barkley, 2012; Grane, Endestad, Pinto, & Solbakk, 2014; Karam et al., 2009).
Subjects with ADHD procrastinate more than subjects without the disorder. Procrastination is defined as the tendency to delay activities that must be completed before a deadline. Several psychosocial interventions designed for adults with ADHD include the treatment of procrastination, but there is very little information about its relationship with ADHD. In fact, procrastination is not officially recognized as a symptom related to this disorder. A recent study of 54 college students found that only inattention correlated with procrastination, once the hyperactivity/ impulsivity domain had been corrected for (Niermann & Scheres, 2014).
This research contributes to the study of ADHD in adulthood in a Latin American population. To our knowledge, this is one of the first studies of a Mexican clinical population, obtained from a research program located at Mexico´s INPRFM, whose main objective is the early detection and study of ADHD throughout life. Among the strengths of this study we can say that we confirmed or ruled out the presence of this neurodevelopmental disorder through a semistructured clinical interview undertaken by an experienced clinician. The limitations in this study, included the fact that executive dysfunction in adults with ADHD was based on a self-report, rather than performance. Convenience sampling was carried out, which reduces the possibility of generalizing results to other clinical populations. Sample size was small, and we did not have healthy controls to contrast our findings. These limitations imply the need to directly evaluate executive functions not only in a self report but with neuropsychological batteries and to use controlled samples rather than convenience samples.
As expected, adults with ADHD versus those without this neurodevelopmental disorder, but with other disorders such as anxiety or depression, were associated with different outcomes and clinical variables related to a more severe, dysfunctional clinical presentation. Special attention must be paid when evaluating women since they have the same risk of developing the disorder, particularly in adulthood. Subjects with ADHD had more comorbidities, were more likely to have difficulties in various psychosocial areas and therefore a more severe prognosis. As reported in previous studies, our research showed that ADHD in adulthood is associated with various executive and non-executive difficulties. Future studies in this sample will help us to understand the clinical course of adults with this neurodevelopmental disorder.