Introduction
The attainment of gender identity is a complex process that, ultimately, guarantees the psychological well-being of the individual beyond the realm of personal identity and sexuality. This intricate process includes physical, psychological, social, emotional, and, for some people, spiritual domains. Therefore, biological and psychological aspects of human gender and sexuality are deeply intertwined as reflected, but not limited to, behaviour, desire, affects, roles, relationships, values, and culture (Lamas, 2012).
Clinical interventions to address sex and gender variance often aim to conform individuals to cultural values on the acceptable boundaries between the binary models including only two different categories: male or female. Thus, transgender people are defined as those whose identity and/or gender expression does not correspond to the social norms and expectations associated with their sex at birth (Pan American Health Organization, 2011). It also encompasses male and female impersonators, especially in the context of artistic performance; individuals who define themselves as bi-gender, gender queer, and gender variant, as well as anyone expressing gender characteristics that do not correspond with those traditionally associated with the sex assigned at birth (Bockting, Benner, & Coleman, 2009).
Although many transgender people are clear about their tastes, attractions, activities, and gender preferences from childhood, they often spend years trying to understand their own identity and may decide to keep it secret, usually to avoid adverse reactions from others (Robles et al., 2016). Some transgender people undergo hormonal and/or surgical treatment to change their bodies, while others do not wish to alter their bodies. Others may consider a legal change of sex as the ultimate evidence of their identity. The process that entails varied gender expressions can be as unique as the psychological needs or support that everyone may need throughout the lifespan.
It is during puberty, which is characterized by the overt development of secondary sexual characteristics, that transgender people often report discomfort with their bodies. Although this displeasure may disappear over time, it is a tenet in psychology and psychiatry that psychological and medical treatment is warranted (Hyderi et al., 2016). But given that this is a sub-specialty within each clinical field, it is not trivial for transgender persons to find qualified professionals while seeking psychological and medical support. When this need is not met, mental and physical health issues can lead to life-threatening situations intimately related to gender identity (United Nations Programme on HIV/AIDS, 2014).
According to current nosological classifications: ICD-10 of the World Health Organisation, and DSM-5 of the American Psychiatric Association (World Health Organization, 1992; American Psychiatric Association, 2013), transgenderism has been used to describe the experiences of all those located somewhere along the poles of male and female in the spectrum of sex and gender expressions. In ICD-10, for example, this condition is described as the “desire to live and be accepted as a member of the opposite sex, usually accompanied by feelings of discomfort or disagreement with one’s own anatomical sex and the wish to undergo surgical or hormonal treatment to make the body as consistent as possible with the preferred sex” (World Health Organization, 1992, pp. 168).
On the other hand, cryptorchidism is defined as the absence of one or both testicles in the scrotal sac due to an undescended or maldescended testis (Brinkmann, Schuetzmann & Richter-Appelt, 2007; American Urological Association, 2014). This condition can be expressed among 46, XY persons, and it does not necessarily reflect an intersex diagnosis. Its prevalence ranges from 0.7% to 8% in newborns and up to 30% among premature babies (Comité Nacional de Endocrinología, 2001; Garnelo & Caamaño, 2005; Secretaría de Salud, 2014). Testis descent can occur at three months of age, although this is less common (2% of reported cases) (Berkowitz et al., 1993).
Current medical treatment of cryptorchidism involves identifying the existence of the gonad and giving it a suitable location to reduce the risk of infertility, inguinal hernia, cancer, and testicular torsion (Ferguson & Agoulnik, 2013). Additionally, untreated cryptorchidism might be related also with long-term effects of hormonal therapy, recurring medical examinations, and manipulations, as well as with psychosocial negative outcomes (including anxiety, depression, social, and scholastic maladjustment, etc.) given that testicles may be symbols of strength, virility, fertility, aggressiveness, and sexuality (Sumfest & Kim, 2018). Thus, many clinicians believe that it should be performed as early as possible, when irreversible changes occur in testicular morphology (Nagar & Haddad, 1997; Docimo, Silver, & Cromie, 2000; Mayo Clinic, 2017); and current guidelines recommend early interventions in order to prevent cancer and infertility (Secretaría de Salud, 2014; American Academy of Pediatrics, 2000), and to reduce the anxiety of the family in defining the sex with which the baby should be raised.
In contrast, there is also evidence that successful scrotal repositioning of the testis does not prevent the potential long-term issues of infertility and testis cancer (Comité Nacional de Endocrinología, 2009; American Urological Association, 2014), and according to Sumfest et al. (2018) there has been little research about the rest of the possible negative consequences, and even less information about issues of psychosexual identity derived from cryptorchidism´s treatment or absence of treatment (Conolly, 1959; Cytryn, Cytryn, & Rieger, 1967; Masi et al., 1999; Galifer, Kalfa, & Guibal, 2004). Thus, it has also been suggested that clinical intervention should wait for persons to develop their gender identity and be able to participate in the decision-making process. This is more so taking into account that gender identity is defined very early in childhood, approximately between the third and fifth year of age (Robles et al., 2016).
As can be seen, the decision of clinical interventions in the case of children with this condition becomes a dilemma between the child’s rights to determine their own sexual characteristics according to her/his gender identity (in the very near future) against the possible problems of living as a child with an indeterminate gender. In the case of the treatment of cryptorchidism, the decision of an early intervention is more unanimous and gender identity matters are considered more as a possible consequence of not treating the cryptorchidism than as a consequence of the its treatment.
Cryptorchidism, transgenderism, and sexual orientation
The variation between sex assigned at birth and the gender identity adopted by a person is not directly related to sexual orientation. Sexual orientation is defined, according to the Pan American Health Organization (2011, p. 13) as: the specific organization of eroticism and the emotional bond of an individual in relation to the gender of the partner involved in sexual activity, and can be expressed as behaviours, thoughts, or sexual fantasies, or a combination of these elements.
In other words, a transgender person may have any sexual orientation, and may or may not present a biological intersex condition. In turn, people with an intersex condition may regard themselves as transgender (Cabral, 2009), although most are not (Reisner et al., 2016). It is not clear how sexual orientation relates to intersex diagnosis, sex assignment at birth, and the medical treatment to which they were subjected to (Reiner & Gearhart, 2004). Therefore, although there may be cases in which intersexuality and transgenderism may coexist with non-normative heterosexual thoughts, fantasies, or behaviours, none of these is the sine qua non of the other. In fact, there is a wide range of possible combinations in relation to sex at birth, gender identity, and sexual orientation.
Specific medical and psychological treatment needs may also vary depending on these combinations. For instance, major surgical interventions in people with intersex conditions (as genitoplacia and gonadectomy) are different from those for a transgender person (Reisner et al., 2016). Nevertheless, they may share physical and psychological needs that primarily stem from medical treatments as well as from stigma and social rejection (Subhrajit, 2014), and mental health care professionals must be prepared to assist these sexual minority populations at any time during their lifespan (Leidolf, Curran, & Scout Bradford, 2008; Mayer et al., 2008).
In order to promote interventions that focus on the perceived needs of those directly involved rather than to parental and medical expectations, the aim of the present case study is to describe the clinical and life histories of a transsexual woman with a history of cryptorchidism at birth and examine the interplay between this relative common testicular problem at birth, and the gender identity and sexual orientation formation processes from her own perspective.
Methods
This is a qualitative study based on a case referred to an in-depth interview during a larger study: “Towards the Categories of Gender Discordance in ICD-11,” approved by the Ethics Committees of Research of the Instituto Nacional de Psiquiatría Ramón de la Fuente Muñíz. The interviews were conducted by the author, a female researcher with a master’s degree, who previously received training from a psychiatrist expert in qualitative methodology. The interviewer at the time of the study was studying a doctorate whose thesis project was about aspects of identity development in childhood. The person interviewed participated in a project on Categories of Gender Discordance in ICD-11, and at the end of her survey she was asked to participate in a project that delved into the process of transgender identity in childhood and was referred to participate in a semistructured interview. The interview was conducted at a care centre specialized in transgender person’s health attention in Mexico City, Mexico, at a private doctor’s office, and after explaining the purpose of the study and obtaining written informed consent to participate.
The participant was the only person to refer a medical history on her genitals. For this reason, she was asked to attend again to be interviewed and repeat the process to inquire about the possible impact of the medical condition on the development of her identity, and thus repeat the process. Duration of the interviews was approximately three hours; interviews were audio recorded and transcribed for a content analyses. The content of the interviews was analysed by three researchers.
Results
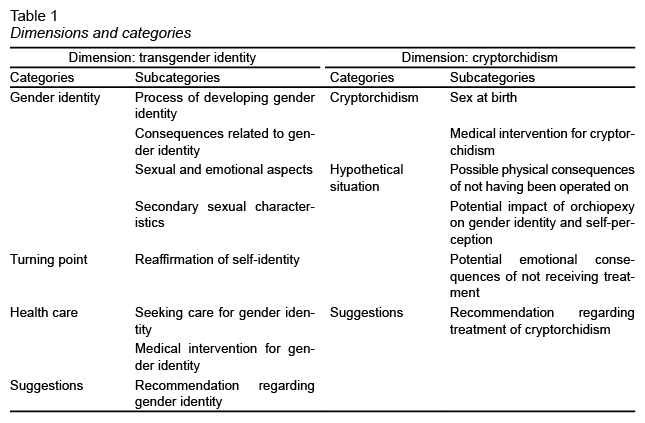
Due to the large amount of information obtained from the interviews, this article will present only the most relevant information. Data are organized in two dimensions: Transgender identity and Cryptorchidism with two categories and fourteen sub-categories ( Table 1 ).
Case description
Gia was 43 years-old at the time of the interview and was married and childless. She was assigned to the male sex and was diagnosed with cryptorchidism. She identified herself as a transgender woman and as lesbian. At the time of the interview, she had been undergoing hormone therapy for four years and had no plans for any sexual reaffirmation surgery.
Dimensions gender identity and cryptorchidism
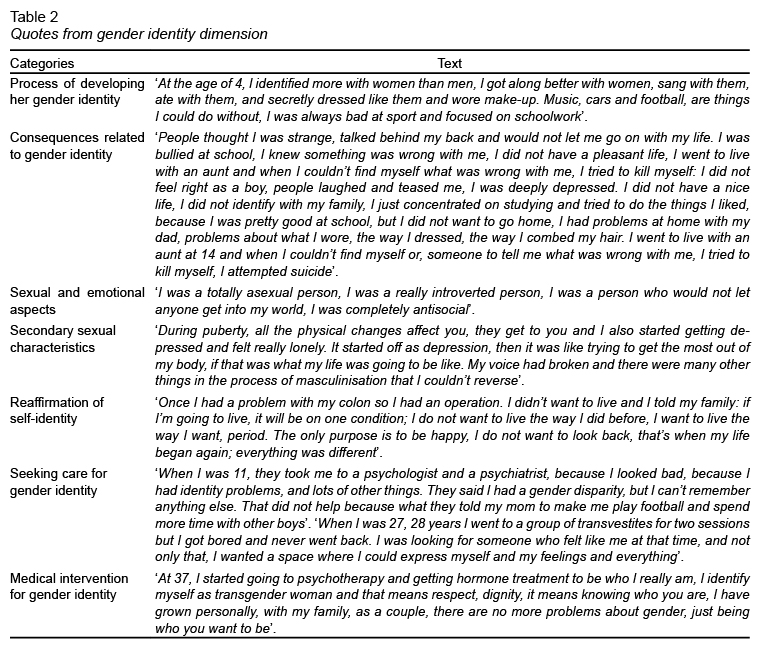
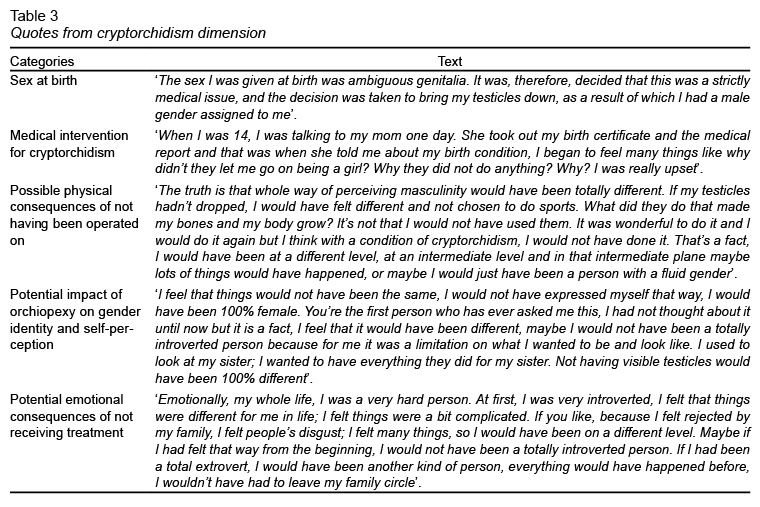
These dimensions describe events that the participant was reporting as they occurred in time. The dimension on gender identity ( Table 2 ) begins with the age at which the participant recognizes the beginning of the process that leads to the appearance of secondary sexual characteristics and their negative impact. Highlight the consequences related to the reactions of other people and not of the gender identity itself in childhood and adolescence, and a turning point in adulthood when she finally negotiates with her family and determines that she will live as she always wished or prefers to die. It also describes a little about her experiences in the search for help. The dimension of cryptorchidism ( Table 3 ) provides information on when and how the participant obtains information about her genitals condition at birth and the medical procedures to which she was subjected. And describe in and hypothetically way, how it would have benefited from not having been treated medically, from bodily changes, a better relationship with the family, an earlier and smoother gender identity transition, and less emotional conflicts.
Categories recommendations from life experience
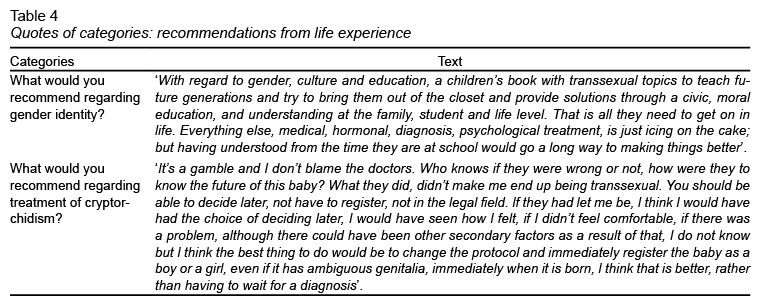
The categories recommendations from life experience ( Table 4 ) provide information about the need to provide information and education on the subject of gender identity from schools, family counseling, medical personnel, and society in general. Regarding cryptorchidism, the participant clearly understands that it is a dilemma and that there is no causal relationship between cryptorchidism and a transgender identity and the importance of considering that the person can decide on her diagnosis and treatment.
Discussion and conclusions
Regarding gender identity, as happens with most transsexual people (Bradley & Zucker, 1997), Gia began to become aware of her gender discordance in childhood. She had clearly different tastes and preferences from what was culturally expected for the sex assigned at birth right after the intervention due to her intersex condition. In many cases, this is related to the presence of family, social, and emotional problems resulting from stigma and discriminatory attitudes. In keeping with the findings in the scientific literature (Steensma et al., 2011), adolescence was one of the most difficult life stages to cope with for Gia; social maladjustments were exacerbated by gender discordance due to the emergence of unwanted secondary sexual characteristics in relation to her gender identity.
Gia consulted health professionals who failed to help her; it was not until she was 37 years-old that she was able to begin her body reconfiguration to adjust her self-representation as a transgender woman. The consequences of inefficient or even damaging interventions caused by medical and psychological treatments shows the urgent need for the development of standardized protocols or algorithms for health care professionals.
Cryptorchidism and transgender identity
Although it is not possible to conclude that Gia’s gender identity is related to her antecedent of cryptorchidism, as she reflected on her medical and life histories, she could only imagine what would have been different for her if there were no clinical interventions in her early development. She concluded that her gender trajectories and her life in general would have been completely different from what she came to feel and to express as a female.
In this sense, the case illustrates that, despite the good intentions of her parents and the medical team, clinical management can violate bodily autonomy and human dignity (Kessler, 1997). The central argument justifying current clinical protocols assumes that the same biological processes that determine and differentiate genital anatomy also play a role in the processes that leads to gender identity formation. The paradoxical term ‘embryology of gender’ has been proposed to highlight this faulty logic that lacks scientific evidence (Jorge, 2010). Thus, in some clinical practice guidelines for the diagnosis and treatment of cryptorchidism, which involve the participation of paediatricians, urologists, surgeons, endocrinologists and other medical professionals (Hughes et al., 2006), no mention is made of mental health staff or of the parents’ involvement during the decision-making process (Jorge & Agramonte, 2013).
Given that the attainment of gender identity is a complex process that guarantees the well-being of the individual beyond the realm of sexuality, it is of critical importance that psychological support is in place to accompany people through clinical interventions. The notion that transgenderism, intersexuality, and genital abnormalities are medical and social emergencies is outdated as we have come to appreciate a spectrum of valid genital anatomies and gender identities that express themselves in thoughts, fantasies, desires, and behaviours that are intrinsic to the human experience as sexual beings. Therefore, we advocate for a psychological algorithm that embraces inter-professional communication specifically designed for people with sex/gender variance focusing on supportive guidance rather than adjustment to parental and medical expectations.
Many urologists and paediatricians might be convinced of the emotional impact of cryptorchidism in children, resting importance to possible negative consequences of its early treatment. However, as it is clearly seen in the case presented here, some people could benefit from not receiving any treatment, and the possible complications of not receiving treatment remain unknown.
Disclosure statement
No potential conflict of interest was reported by the authors.
Funding
The Consejo Nacional de Ciencia y Tecnología (CONACyT) through doctoral scholarship (T. R.).