Introduction
Although there are psychosocial-family interventions complementary to the biomedical treatment of schizophrenia, there is still little evidence of their effectiveness in Latin American countries.
Richardson (1948) described the role of family care in recovery from physical and mental health problems. Sometime later, a team of British social psychiatrists and sociologists, led by George Brown (Brown, Birley, & Wing, 1972), studied the relocation of long-stay residents at psychiatric hospitals in the community. In the late 1970s, Zubin and Spring developed the Theory of Vulnerability, providing the basis for significant development in the psychosocial therapeutics of schizophrenia. This explanatory model is based on the assumption that there is a predisposition to psychosis of a genetic or acquired nature, as a consequence of brain damage, which in turn is related to stress, which acts as a trigger (Zubin & Spring, 1977). The stress-vulnerability hypothesis is supported by neurodevelopmental theories that propose a physiopathological model, in which genetic components and stress are interactively integrated. Thus, in patients with schizophrenia, there is a faulty release of norepinephrine and adrenocorticotropin in response to physical stress, and an inadequate release of cortisol in response to stress caused by psychosocial factors, which would have consequences for clinical symptoms (Olivares, Arango, & Buchanan, 2000; Saiz, de la Vega, & Sánchez, 2010).
The origins of the concept of Expressed Emotion date back to the 1950s, with the seminal work of Brown (Brown, 1959). In 1956, in a study of 229 patients discharged from psychiatric hospitals, Brown noted that the strongest link between relapse and re-entry was the type of home patients returned to following their discharge. Patients who returned to the home of their parents or wives were more prone to relapses and readmissions, while patients who stayed with their mothers had a lower risk of relapse and readmission, when they and/or their mothers went to work. Accordingly, Brown developed the concept of “Expressed Emotion” (EE), proposing its five components: 1. critical comments, 2. hostility, 3. emotional involvement, 4. positive comments, and 5. warmth. EE is a concept that reflects the emotional atmosphere within a family nucleus expressed towards those who are sick or have behavioral disorders. High expressed emotion is defined as high levels of criticism, hostility, or emotional involvement towards the patient (Brown, 1959). In a review of 26 studies, Kavanagh (1992) found that the relapse rate was 48% for patients residing with relatives with high EE and 21% for those with families with low EE. An analysis conducted by Bebbington (Bebbington, Kuipers, & Ballenger, 1996) of data on 1,346 patients established a relationship between the expressed emotion of the family caregiver and relapses, as well as the protective function of reducing face-to-face contact for patients from families with high expressed emotion.
Family Behavioral Therapy in schizophrenia
Historically, schizophrenia has been one of the disorders most commonly addressed by family therapy. In the 1950s, the first family therapy approaches were provided by North American authors such as Bateson, Lidz, Wynne, and Bowen, for whom psychosis was a symptom of dysfunctional family interaction. Two large groups of researchers subsequently developed systemic family therapy, in Milan and Heidelberg. In the 1960s, there were various opinions about alterations of communication in parents of people with schizophrenia. Based on these studies, various models have proposed specific family approaches for schizophrenia, the most developed ones being the systemic, psychoeducational, behavioral, and psychoanalytic approaches. Falloon & Liberman (1983) published the general results of an intervention in families of people with schizophrenia, which they later called Family Behavioral Therapy (FBT).
FBT is based on the theory of social learning. Its effect is explained by the theory of vulnerability to stress through the concepts of deviant communication (DC), affective styles (AS), and expressed emotion (EE). FBT uses highly structured, directive behavioral techniques for skills development such as assessing the skills and shortcomings of each family member and the family group as a whole, education, repeated practice, objective formulation, modeling, behavioral rehearsal, reinforcement, and task assignment. Europe has had extensive experience with FBT in countries such as the United Kingdom, Spain, Italy, and Portugal, where it has proved to have favorable effects on social functioning and a decrease in relapses (Gonçalves-Pereira, Xavier, & Fadden, 2007). In England, this therapy has achieved an advanced level of development; FBT has demonstrated an association with better social functioning and a reduction of relapses in people with schizophrenia coupled with a decrease in expressed emotion in the primary caregivers. In Europe, Portugal is one of the countries that has achieved a high level of development in this area, through its liaison with and training in the MERIDEN Program (Gonçalves-Pereira et al., 2007; Burbach, Fadden, & Smith, 2010).
Specific objectives
To evaluate the effectiveness of FBT, with respect to usual care, in people with schizophrenia treated at the outpatient psychiatric department of a public hospital in Chile in relation to the social functioning, treatment adherence, and clinical symptomatology of the person with schizophrenia and the decrease in expressed emotion in the primary caregiver, after the intervention has been completed.
Hypothesis
-
People with schizophrenia who receive treatment with FBT display better social functioning, clinical symptoms, and treatment adherence than those receiving usual care, evaluated three months after the intervention has finished.
-
Primary caregivers of people with schizophrenia who receive treatment with FBT have lower levels of expressed emotion in comparison with those who receive usual care, evaluated three months after the intervention has ended.
Method
This was a quantitative, longitudinal study, which assumed the design of a Randomized Controlled Clinical Trial (RCCT) with pre-post, two-arm, parallel, single-blind measurements. A total of 61 people who received outpatient treatment at the psychiatric department of a hospital in the Health Service network in Chile between 2006 and 2014 were evaluated. The sample comprised men and women aged 18 to 64, diagnosed with schizophrenia, according to DSM-V criteria and their respective primary caregiver. Primary caregivers are understood as the persons in the family group who maintain the closest human contact with patients, and whose main function is to meet their physical and emotional needs. He/she is the person who accompanies a user to his/her medical check-ups.
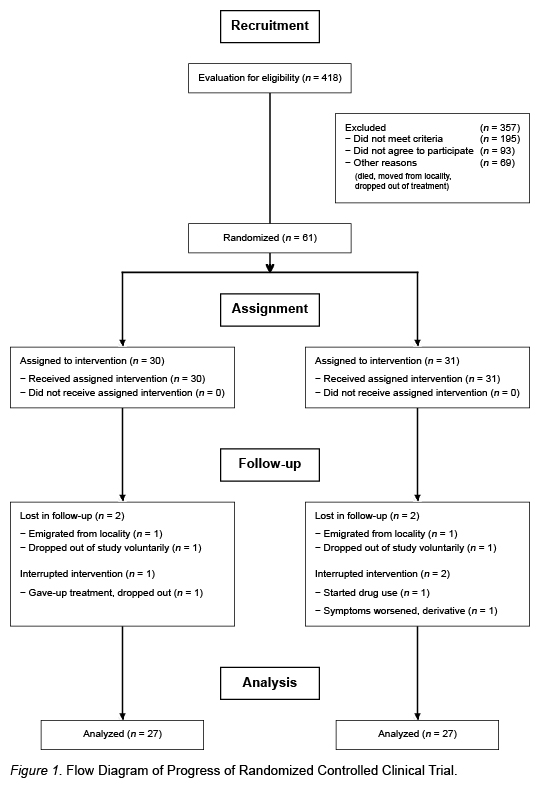
The study excluded subjects with mental retardation, the presence of severe neurological comorbidity that prevented their evaluation, to dependence to alcohol or other drugs, in accordance with DSM-V criteria. Sample size was calculated using the Ene 3.0 statistical program to detect differences in the contrast null hypothesis Ho: µ1 = µ2 through the bilateral student’s T test for two independent samples, considering a significance level of 0.05. This yielded a total sample of 56 people, 28 for the control group and 28 for the experimental group. When the percentage of loss was estimated, a total of 61 people was achieved. Subjects were assigned to two groups through a simple random procedure, using a table of random numbers that were not repeated. This procedure was performed by a professional social worker unrelated to the research project. The groups considered were: the experimental group (n = 31), which received the FBT, in addition to usual care, and the control group (n = 30), which received usual care. The final sample consisted of a total of 54 people: 27 in the control group and 27 in the experimental group (Figure 1). The contact and initial evaluation of the participants was performed in their homes and the instruments were applied in the psychiatric department mentioned earlier by recently-graduated professional social workers. The clinical evaluations were applied by psychiatrists after informed consent forms had been signed by potential participants. Socio-demographic and clinical data were obtained by reviewing the medical records. The instruments were applied at the initial moment and baseline measurement, while the post measurement was applied after a three months follow-up. The study was approved once the protocol had been approved by the Ethics Committee of the respective health service.
Measuring instruments
-
Clinical, psychosocial, family, and sociodemographic background questionnaire, prepared by the researcher, including a history of the person with schizophrenia and his/her primary caregiver.
-
Personal and Social Performance Scale (PSP), to evaluate social functioning. The Spanish version, validated by García-Portilla et al. (2011), was used. The PSP uses a scale of 1 to 100 to evaluate the functioning of the patient according to four operating domains: 1. work/studies; 2. personal and social relationships; 3. self-care; and 4. disturbing and aggressive behaviors. Each of these areas is rated using a 6-point Likert-type scale of severity, ranging from 1 (absent) to 6 (very serious). The PSP provides scores for each of the four areas ‒higher scores indicate worse performance‒ and an overall score, in which higher values reflect better personal and social functioning. In their validation, García-Portilla et al. (2011) reported a Cronbach’s alpha of .874 and a test-retest reliability of .979 (95% CI). For the present study, a Cronbach’s alpha of .81 was obtained.
-
Positive and Negative Syndrome Scale (PANSS). This scale evaluates positive and negative symptoms in schizophrenia and general psychopathology. The PANSS, developed by Kay, Fiszbein, & Opler (1987), is based on the Brief Psychiatric Rating Scale (BPRS). In this study, we used the version validated in Spanish by Peralta and Cuesta (1994), who reported high internal consistency (Cronbach’s alpha of .73 for the positive scale, .83 for the negative scale and .87 for general psychopathology), and adequate test-retest stability. The intraclass correlation coefficient is approximately .80 for the three subscales. In the sample of the present study, a Cronbach’s alpha of .78 was obtained for the positive scale, .80 for the negative scale, and .82 for general psychopathology).
-
Five Minute Speech Sample (FMSS). This sample was used to evaluate expressed emotion in the primary caregiver. The FMSS, validated by Magaña et al. (1986), is based on the same construct as the Camberwell Family Interview (CFI); in other words: 1. critical comments, 2. hostility, 3. over-involvement, 4. affect, and 5. positive comments. A final score is obtained, following the classic score criteria of Vaughn (1986). Magaña et al. (1986) report an internal consistency of over .80 and a test-retest reliability of .64.
-
Morisky-Green test. This test was used to evaluate treatment adherence. Designed by Morisky, Green, & Levine (1986), it has predictive validity, concomitant with an alpha of .61. In the present study, an alpha of .64 was obtained.
Data analysis
The Stata Statistical Program (V.11.0) was used. A descriptive analysis of the sociodemographic and clinical characteristics of the total sample and of both groups was carried out separately. The Student’s t-test was used for independent samples with unilateral contrast at the time of the baseline measurement to detect differences between groups. The Shapiro-Wylkes test was applied to evaluate the normal distribution of the variables, only obtaining the treatment adherence variable as an exception to this condition, as a result of which it was analyzed using non-parametric statistics. For the hypothesis test, ANOVA of repeated measures was applied in order to establish the variation of variables over time, which made it possible to analyze intra- and inter-group variability, controlling for the different variables that might influence the results. In order to calculate the effect size, the change in follow-up was evaluated with respect to the initial score in the outcome variable, and Cohen’s guidelines (1992) en la página 73 were used as reference. The criterion used to determine the statistical significance of the results was α = .05. Data were analyzed according to “intention to treat.”
Description of the intervention to be implemented in the treatment group: FBT
The intervention was based on and faithfully respected the form and content aspects of the Falloon FBT; only the frequencies of the sessions were adapted to increase the feasibility of the research. Although the original model proposes weekly, biweekly and monthly sequences, in this research, all the sessions had a weekly frequency. Twelve sessions distributed in four phases were developed: a) Psychoeducation: two sessions; b) Communication training: four sessions; c) Problem-solving training: four sessions; and d) Social skills and operant conditioning training: two sessions The intervention had a total duration of three months. All the sessions lasted one hour and were held at the home of the person with schizophrenia, with the participation of this person and that of members of the family group, including the primary caregiver. It was applied by psychologists and social workers trained by a qualified monitor accredited by the Meriden Institute of England. To ensure adherence to the protocol in the application of the therapy, retraining and monitoring sessions were conducted by two psychologists trained in the technique and with clinical experience in the management of patients with severe mental disorders. In addition, a manual specifying the contents of each session was reviewed and adapted. However, even though it is a structured intervention strategy, it has a certain amount of flexibility enabling it to be adapted to the pace and needs of each family.
Description of usual intervention
The intervention followed the indications of the 2005 Clinical Guide for the Treatment of Persons with a First Episode of Schizophrenia, which specifies the “Comprehensive treatment for people with schizophrenia according to the phase of the disease” (Ministry of Health, 2005).
Ethical considerations: Authorization was obtained from the Scientific Ethics Committee of the Health Service so that all the ethical requirements and safeguards stipulated in national and international regulations were met.
Results
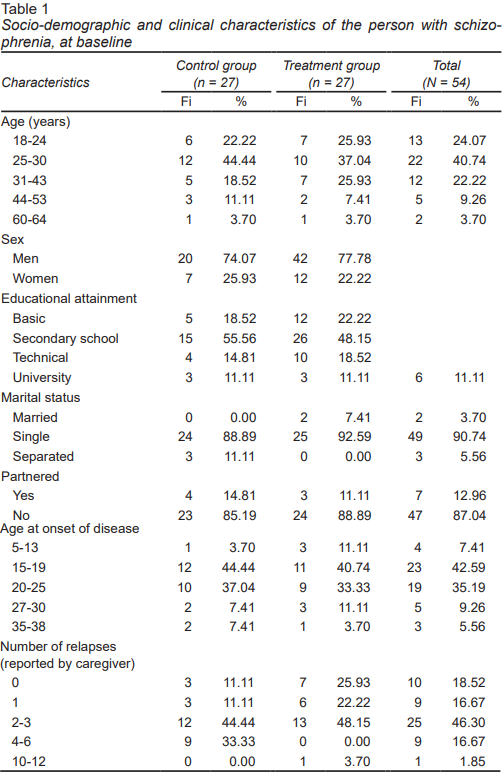
Sample description. In the population studied, a higher proportion of men than women was found in both the control group and the treatment group (CG = 74.07%, TG = 81.48%). For age, the highest frequencies in both groups were concentrated in the 25- to 30-year cohort (CG = 44.44%, TG = 37.04%). As for educational achievement, trends were similar for both groups, with the highest proportion of people being found in the category of middle school education (GC = 55.56%, GT = 40.74) (Table 1).
The population of primary caregivers was mainly middle-aged. In relation to the average hours of care reported by the caregiver, the highest percentage was in the 8- to 12-hour category (46.3% for the total sample), with similar percentages for both groups (CG = 51.8%; TG = 40.7%).
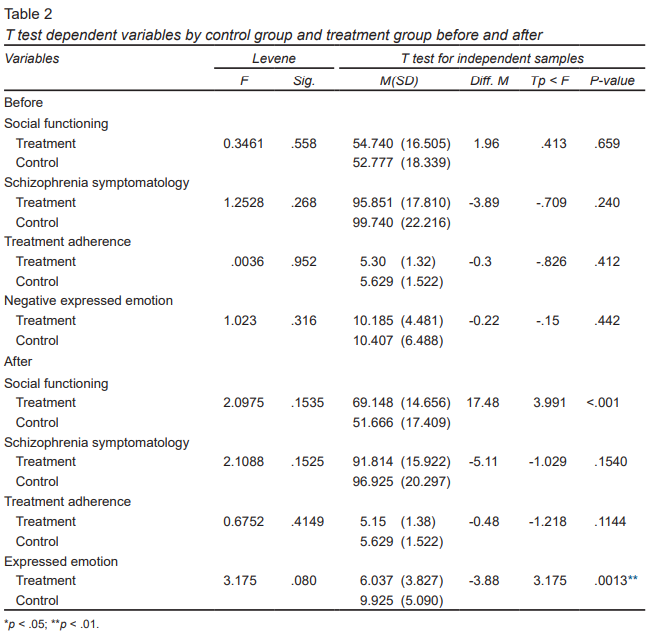
Table 2 shows that the comparison between groups at the time of the baseline measurement, using the Student’s t test for independent samples with unilateral contrast and analyzing equality of variances according to Levene, failed to show significant differences between the two groups for any of the four dependent variables studied. In the post-intervention measurement, significant differences were observed between the two groups for social functioning (t(52) = 3.991; p = .0001) and negative expressed emotion (t(10) = 3.175; p = .0013*). This difference showed that people with schizophrenia who received FBT achieved significantly higher scores in social functioning, in comparison with those who only continued with their usual treatment. Likewise, the caregivers of these patients showed a reduction in negative expressed emotion in comparison with those in the control group.
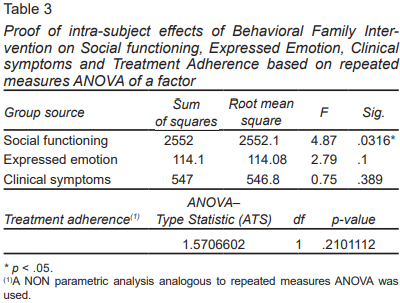
The test of intra-subject effects based on the repeated measures ANOVA of a factor, used for hypothesis testing, yielded a significance of .0316 (p <.05) for social functioning. No intra-subject effects (p = .389) for the clinical symptom variable ( Table 3 ) were observed, and although the treatment group favorably modified its post-intervention mean (GT:Mbefore = 95.85 (17.81); Mafter = 91.81 (15.92), dif M pre-post = 4.04) to a greater extent (Table 2), these differences did not prove to be statistically significant (p = .389) (Table 3).
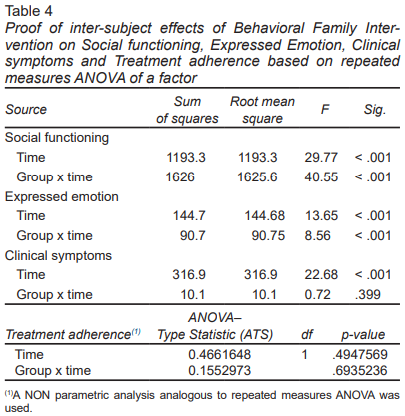
For social functioning, statistically significant differences are found in the test of inter-subject effects for time factor (1.37 e-0.6 for a p < .001). The same situation was observed when considering the interaction time × group (5.03 e-0.8 for a p < .001) (Table 4). A second finding was the effect of FBT on EE by the primary caregiver. The inter-subject effects test showed a significant effect, both when considering the time effect (p < .00053) and for the time x group interaction (p < .00053). In both cases, EE decreased in the treatment group in the post intervention moment. In the inter subjects test, an effect was found by time (p = 1.57e-0.5) (Table 3), with both groups decreasing their symptomatology at post measurement. No group × time interaction effect was found (Table 4).
Lastly, regarding the treatment adherence variable of people with schizophrenia, there is no evidence in either test, of intra- and inter-subject effects, of the effect of FBT on treatment adherence. Although the treatment group decreases its average score in the post measure, compared to the pre-intervention measurement (MA = 5.30; MD after = 5.15) (Table 2), which indicates greater adherence, this difference is not statistically significant (p = .2101112) (Table 3).
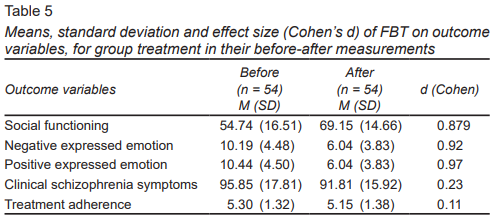
Analysis of the effect size of FBT on pre- and post-test measurements, with respect to the treatment group, shows a large effect size of FBT on the social functioning of the patient (d = .87) and negative expressed emotion of the caregiver (d = .92) variables. For the clinical symptom variable, a small effect size was observed (d = .23) (Table 5).
Finally, the therapeutic effect on the results obtained by each participant in the study was analyzed. The results did not show any statistically significant differences, making it possible to highlight the value of FBT as a standardized intervention strategy.
Discussion and conclusion
This is one of the few studies in Latin America to have evaluated the results of the application of FBT in patients with schizophrenia. The findings show the effectiveness of the use of a specific, standardized intervention model, based on a conceptual theoretical framework congruent with current intervention strategies and purposes for working with people with schizophrenia. The results indicate an increase in social functioning in the user and a decrease in EE in the primary caregiver, with a large effect size being observed in both variables (Table 5). These findings are consistent with what was reported by Roncone, Morosini, Falloon, & Casacchia (2002) in a study of 36 people with schizophrenia, who participated in an FBT program for three months and were evaluated six months later showed a significant increase in social functioning. They also agreed with the findings of Espina and González (2003), who, in a study of 36 people diagnosed with schizophrenia in the Basque Country, Spain, compared three types of intervention (Family Therapy [FT], Parent Support Group plus Group Therapy for patients [PSG+GT], and psychopedagogical therapy [PT]) and concluded that patients in the groups that received family therapy and the parent support group plus group therapy for patients showed statistically significant improvements in symptomatology and social adjustment, while those who received pedagogical therapy and the control group did not show the same effects.
Regarding the decrease in expressed emotion of the primary caregiver, since the pioneering studies of Brown (Brown, 1959; Brown & Rutter, 1966; Brown, Birley, & Wing, 1972), who associated the measure with the course of the evolution of schizophrenia, most subsequent studies have continued to explore this line. They have also associated the psychosocial intervention implemented in addition to pharmacological treatment with the decrease in expressed emotion (Vaughn, 1986; Gonçalves-Pereira et al., 2007; Bucci, Berry, Barrowclough, & Haddock, 2016; Grácio, Gonçalves-Pereira, & Leff, 2016; Leff, Kuipers, Berkowitz, Eberlein-Vries, & Sturgeon, 1982; Amaresha & Venkatasubramanian, 2012; McFarlane, 2016; Marvin, Miklowitz, O’Brien, & Cannon, 2016). As regards clinical symptoms, our study does not show a clear effect of FBT reducing them, which coincides with what has been reported by other previous studies (Lobban et al., 2013; Nilsen, Frich, Friis, Norheim, & Røssberg, 2016; Lobban & Barrowclough, 2016). However, it is important to highlight the fact that although there are no statistically significant differences in the post-intervention clinical symptomatology between both groups, when considering the differences in means within each of the groups, a larger favorable change was observed in the treatment group in post-intervention measurement, with no inter-subject effects being detected.
Finally, the results of this study do not show any effect of FBT on increased treatment adherence. Although the treatment group decreased its average score in the post measure, compared with the pre-intervention measurement, indicating greater adherence, this difference is not statistically significant. This result suggests the need for a more in-depth review in the future and for comparisons using a different measurement instrument.
There is evidence that systematic, protocolized support programs, in addition to usual medical treatment, contribute to improving low adherence (Cirici, 2002) and also, albeit to a lesser extent, improve clinical indicators and social functioning, which in turn contributes to decreasing clinical deterioration and the disability associated with severe mental disorders (Lobban & Barrowclough, 2016; Caqueo et al., 2015; Pharoah, Mari, Rathbone, & Wong, 2010).
Limitations
The main limitation of this study is the low sample size obtained after the selection of the study population. Likewise, the instrument used may have influenced the non-detection of significant differences between groups for the adherence variable.