Introduction
Depression and anxiety are considered the most frequent mental disorders in the world; they cause disability, mortality, and loss of productivity (Klumpp & Shankman, 2018).
Mental and behavioral disorders account for 14% of the global of disease burden and are one of the leading causes of disability worldwide, collectively accumulating more than 40 million years lost due to disability among people aged 20 to 29 during 2010 (Institute for Health Metrics and Evaluation, Human Development Network, & World Bank, 2013).
People whose work involves caring or assisting other people suffer from emotional exhaustion, depersonalization, and under personal achievement that make them more susceptible to depressive disorders (Maslach, Jackson, & Leiter, 1996).
In medical students it has been reported that tobacco use is higher when they have depression or anxiety compared to those who do not have it (31% vs. 19%, p < .007) (Romero, Santander, Hitschfeld, Labbé, & Zamora, 2009).
In another study, medical residents responded that they felt excessively tired and that the workload did not allow them to care for other areas of their lives (Saravanan & Wilks, 2014).
In Mexico, Martínez-Lanz, Medina-Mora, and Rivera (2005) reported that 47.5% of medical residents have depressive symptoms, 16.4% have high stress levels, 55% use tobacco, 65% use alcohol, and 23% have used any drugs.
Fahrenkopf et al. (2008) reported that mental disorders affect job performance because concentration capacity decreases (residents with depression have up to 70% difficulty in concentration compared to 38% of residents without depression). Burnout was also common among resident physicians and was associated with self-reported suboptimal patient care practices (Shanafelt, Bradley, Wipf, & Back, 2002).
In a study about depression over an academic year, it was observed that residentes with depressive disorder had a personal history of depression (Jiménez-López, Arenas-Osuna, & Angeles-Garay, 2015).
Although mental disorders and physical discomfort from the academic and work burden of residency have been extensively studied, their association has only been superficially investigated. The aim of this study is to know the association of depression and anxiety with characteristics related to the training of medical residents.
Method
Place
The study was carried out at the Unidad Médica de Alta Especialidad (UMAE), Centro Médico Nacional La Raza. 50% were in a medical specialty, 37% in a medical-surgical specialty, and 13% in a surgical specialty; 75% were in second or third grade.
Subjects
This study included all of the medical residents that were working at the UMAE at the time of the study (542). The sampling method was not probabilistic with a sample size of 423 calculated for an unknown proportion; an expected proportion of .50, 95% safety level and 10% losses were considered.
Measurements
The DSM-IV criteria were used for the confirmation of the diagnosis of depression and anxiety through the Mini International Neuropsychiatric Interview (MINI), in its version adapted at the Instituto Nacional de Psiquiatría Ramón de la Fuente to Latin American Spanish by Heinze, Sheehan, & Cortés (2000). Alcohol consumption, tobacco use, and emotional exhaustion were assessed with validated scales (Alcohol Use Disorders Identification Test, Fagestrom test and Maslach Burnout Inventory, respectively), the rest of the characteristics related to training (specialty, grade, frequency of guards, work fatigue, and reduction of work performance by unsatisfactory sleep) as well as the personal history of anxiety and/or depression and the presence of medical illness were obtained through direct questions.
Alcohol Use Disorders Identification Test (AUDIT), Spanish versión, consists of 10 questions that explore the frequency and intensity of consumption of alcoholic beverages. The first three questions inquire about the frequency of consumption, number of drinks on a typical day, and excessive consumption. It includes three questions of dependency symptoms and the last four relate to problems by consumption; questions have five answer options (from 0 to 4) and the last two, three options (with values 0, 2 and 4). The minimum rating is zero and the maximum is 40 (Medina-Mora, Carreño, & de la Fuente, 1998).
The Fagerström Test for Nicotine Dependence (FTND) assesses nicotine dependence, scores range from 0 to 10. Scores of 2, 4, 5, 7, and 10 represent cut-points of very low, low, moderate, high, and very high nicotine dependence, respectively (de Meneses-Gaya et al., 2009).
The Maslach Burnout Inventory (MBI) evaluates three domains of burnout: 1. emotional exhaustion, which is measured with a subscale of nine items; 2. depersonalization, which is measured with a subscale of five items; and 3. personal accomplishment, which is measured with eight items. On the basis of the MBI responses, independent subscale scores are calculated for each of the three domains of burnout (Maslach et al., 1996).
Procedure
Each clinical department was asked to list the names of medical residents assigned to that service and appointments were scheduled in groups of no more than five. Participants were informed about the research and those who met the inclusion criteria were invited to participate, Informed consent was obtained for all participants. The MINI was applied individually by a trained researcher and the questionnaire was subsequently given to each of the participants for simultaneous response. The questionnaire did not record any participant’s name; it was assigned a folio that allowed identifying it in case of required specialized assessment (generalized anxiety disorder, depressive disorder).
Data analysis
Statistical analyses were performed using the Statistical Package for the Social Sciences (SPSS), version 19 and EPIDAT 3.1.
Univariate Analysis: For qualitative variables, simple frequencies and proportions were calculated. For quantitative variables, central trend measures (mean, median) and dispersion measures (standard deviation) were calculated. Normality tests were performed (Kolmogorov-Smirnov or Shapiro-Wilk).
Bivariate Analysis: Odds Ratio was estimated for prevalence with 95% confidence intervals and p value < .05. The hypothesis contrast was made using Mann-Whitney’s U-use or Kruskal Wallis. Pearson Square Chi or Fisher’s Exact Test was used as an association measure.
Multivariate analysis: A logistic regression model was performed including only statistically significant or clinically important variables that could explain depression and anxiety.
Ethical considerations
The study was approved by the health research and ethics committee of the UMAE, La Raza. Prior to inclusion, the informed consent of all participants was obtained.
Results
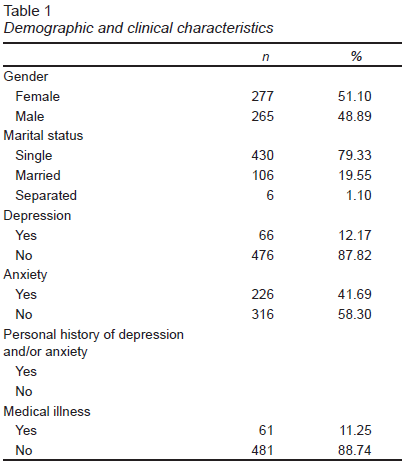
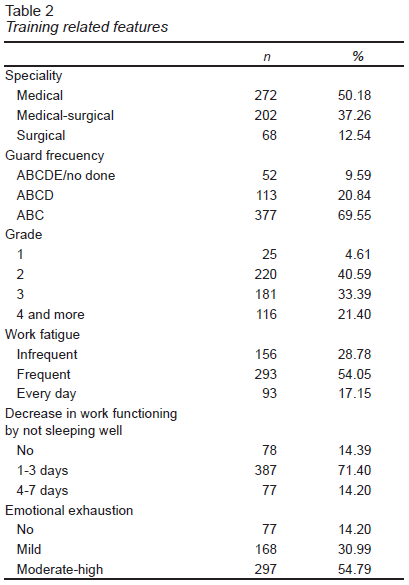
Demographic and clinical data are displayed in Table 1. Subjects were predominantly single (79.33%) and presented anxiety (41.69%). Regarding substance consumption: 70 (12.91%) reported risky alcohol consumption, 3 (.55%) harmful consumption, 404 (74.72%) risk-free consumption, and 65 (11.99%) did not consume; 66 (12.17%) used tobacco without dependence, 45 (9.95%) with low dependency, 2 (.36%) with moderate dependence, and 429 (79.15%) reported not smoking; 75 (13.83%) reported drug use more than a year ago, and an equal number in the last year, 392 (72.32%) did not consume; the rest of the training-related features are listed in Table 2
When analyzing by grade of residence and kind of specialty, working hours without guard and sleeping hours without guard, it was observed that the surgical specialties were those with longer working hours and less sleep hours. The prevalence of major depression and generalized anxiety disorder was 12.2% (95% CI [9.33, 15.02]) and 41.7% (95% CI [37.45, 45.94]), respectively. Regarding the consumption of substances, 80% consumed alcohol, 20.9% consumed tobacco, and 27.6% had used drugs.
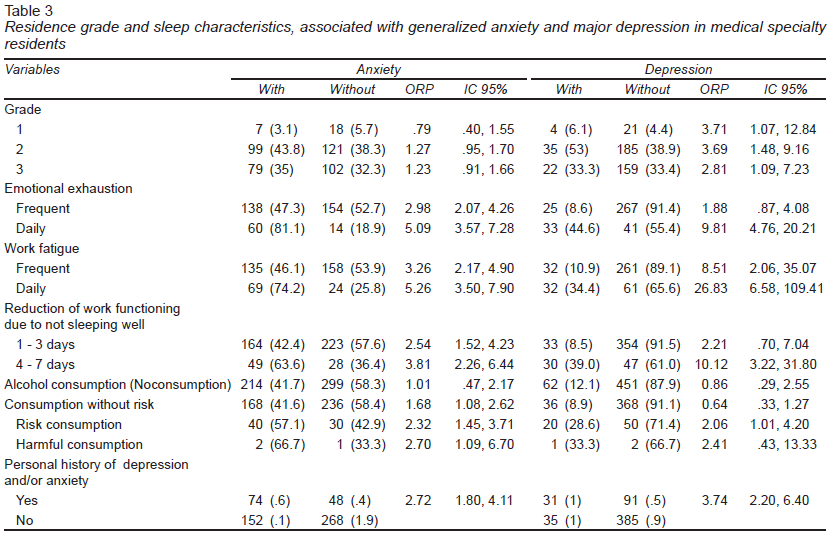
When performing the bivariate analysis for depression, the characteristics with the greatest risk were: present daily work fatigue, ORP 26.83 (95% CI [6.58, 109.41], p < .001), daily emotional exhaustion, ORP 9.81 (95% CI [4.76, 20.21], p < .001), decrease in work functioning by not sleeping well, ORP 10.12 (95% CI [3.22, 31.80], p < .001), personal history of depression and/or anxiety, ORP 3.74 (95% CI [2.20, 6.40], p < .001), and being in the 1st grade of residence, ORP 3.71 (95% CI [1.07, 12.84], p = .02). For anxiety, the characteristics of the highest risks are: daily emotional exhaustion, ORP 5.09 (95% CI [3.57, 7.28], p < .001), work fatigue every day, ORP 5.26 (95% CI [3.50, 7.90], p < .001), decrease in work functioning by not sleeping well, ORP 3.81 (95% CI [2.26, 6.44], p < .001), personal history of depression and/or anxiety, ORP 2.72 (95% CI [1.80, 4.11], p < .001), and harmful alcohol consumption, ORP 2.70 (95% CI [1.09, 6.70], p < .001) (Table 3).
In the analysis of the association of residence characteristics and disorders studied, depression and anxiety were found to have a higher association with ABC guard, ORP 1.13 (95% CI [.50, 2.50]) and ORP 1.42 (95% CI [.93, 2.17]), respectively. For tobacco use, a greater association was found with depression and anxiety when consumption was low dependence with ORP 2.70 (95% CI [1.58, 4.60]) and ORP 1.45 (95% CI [1.08, 1.92]), respectively.
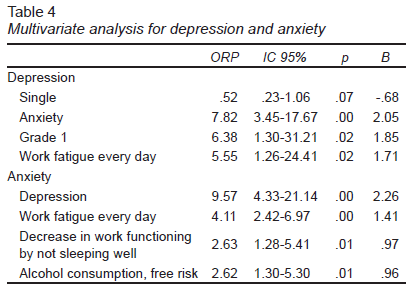
Finally, multivariate analysis shows that work fatigue increases the risk of depression or anxiety more than five times, and that the presence of one of the disorders increases the risk of the other more than seven times (Table 4).
Discussion and conclusion
Although reports of emotional distress related to medical work date back to approximately 50 years ago, research in training doctors is relatively recent. The manifestations studied range from stress and burnout to mental disorders and suicide as the most important complication (Mata et al., 2015).
The reasons of the high frequency of mental disorders in medical residents are a matter of debate. In some reports, they are attributed to the characteristics of medical residence; in others to the predisposition for mental disorder (Center et al., 2003). Our results confirm that some characteristics inherent to residence (work fatigue, emotional exhaustion, decrease in work functioning by not sleeping well, personal history of mental disorder, and harmful alcohol and tobacco use) increase the risk of suffering from depression and anxiety. The association with chronic disease is also confirmed.
Finally, it is important to mention that a weakness of the study is that the sample is limited to residents of a High Specialty Medical Unit. However, it is likely that the characteristics inherent to medical residency are very similar at all levels of care. Since our study is cross-sectional, there is temporary ambiguity, so the results must be interpreted with caution. Another important factor is the possibility of having an information bias, since the responses of medical residents may not reflect the situation nowadays. One of the causes is that the questionnaire was not carried out privately and was self-applied, and when incurring in this kind of bias it is not possible to determine the affectation of the risk, since it can be overestimated or underestimated.
However, all in all the strengths of our study were that we used an instrument to diagnose mental disorders rather than to measure symptoms, in addition to adding scales in the case of substance use-abuse (alcohol and tobacco). Medical residents of 32 specialties were included (medical, medical-surgical, and surgical) which allows the characteristics of the sample to be heterogeneous compared to other studies. The sample inquired about other characteristics of the residence (type of guard, hours of workday, labor fatigue, emotional exhaustion) that have not been described in similar studies. Also, the sample size was higher than other studies conducted in our country in this type of population.
Because depression and anxiety associated with training-related characteristics in resident physicians are prevalent, scrutiny of such problems is recommended in order to implement interventions that mitigate discomfort and prevent poor patient care.