Introduction
Non-suicidal self-injury (NSSI) is the direct and intentional destruction of one’s body tissue, implemented without conscious intent to die and, often, as a dysfunctional mechanism of emotion regulation (Nock, 2010). Currently, it is considered an important public health problem, given the high prevalence estimates in the population of adolescents and young adults, which range between 12 and 23% (Ammerman, Jacobucci, & McCloskey, 2018; Mortier et al., 2017; Muehlenkamp, Claes, Havertape, & Plener, 2012). In Mexican population, Castro-Silva et al. (2017) found that 30.9% of their college student sample reported episodes of an experimental nature, while 26.9% had a pattern of greater frequency and severity. Regarding school adolescents, Albores-Gallo et al. (2014) found a prevalence of 17.1%, however, only 5.6% met the diagnostic criteria of the American Psychiatric Association (2013).
The prevalence of NSSI is consistently higher in clinical population, with estimates that vary from 41% (Claes, Vandereycken, & Vertommen, 2007), 60% and up to 82.4% in adolescents and young adults (Kaess et al., 2013; Nock & Prinstein, 2004). Even more, there is evidence that comparing inpatient versus outpatient NSSI thoughts and behaviors frequency, the prevalence is higher for adolescents receiving in-hospital treatment (Glenn et al., 2017). In Mexico we still do not have precise estimates of prevalence for this population profile. The only work found on this topic was that of Ulloa-Flores, Contreras Hernández, Paniagua Navarrete, & Victoria Figueroa, (2013) who studied retrospectively from the clinical record, a sample of 556 adolescents (average age of 14.46 years), who were treated in a children’s psychiatric hospital during the period between 2005 and 2011. It was found that this proportion of patients corresponded to 9.8% of the total population attended during the aforementioned period.
Related to NSSI, a poorly studied sector on clinical population are adolescents who suffer from psychosocial vulnerability conditions, a group that Raymond, Iasiello, Jarden, and Kelly (2018) call disadvantaged young people. The concept refers to the group of individuals that present one or more risk factors, such as suffering from a mental disorder, dropping out of school, problems with justice, coming from contexts of marginalization and poverty, among others. Each of them contributes to severely limit the young person’s ability to reach his or her potential. These factors are emphasized since there is strong evidence about their power of negative impact on teenagers’ lives.
The conditions of extreme poverty seriously compromise the optimal development of children who suffer from it, in addition to promoting additional risk factors and their transmission to the next generation. Adoption of street life is among the main ones (Hossain & Alam, 2016), which is closely related to family dysfunction and early experiences of interpersonal trauma and revictimization, commonly generated by the attachment figures themselves (Martin et al., 2016; Kagan, Henry, Richardson, Trinkle, & LaFrenier, 2014). So, the group of vulnerable adolescents tend to be affected in their psycho-emotional state, mainly, trauma spectrum disorders, difficulties in emotion regulation (Linehan, 1993), compromised neurobiological development (Perry, Pollard, Blakley, Baker, & Vigilante, 1995), depressive and anxious disorders (Shein-Szydlo et al., 2016), disorders related to insecure attachment (Kagan, 2006), as well as behavioral disorders in the form of impulsivity, oppositionalism, and self-destructiveness (Font & Berger, 2015), all of them have been associated with the presence of NSSI (Liu, Scopelliti, Pittman, & Zamora, 2018; Marín-Tejeda, 2013).
According to the previous description, the group of vulnerable adolescents frequently suffer from a configuration of symptoms that meets the formal diagnostic criteria for different psychiatric disorders and therefore, they can be considered a high-risk population for presenting NSSI (Cipriano, Cella, & Cotrufo, 2017; Kaess et al., 2013). In addition, the close relationship between NSSI and interpersonal trauma as a more severe trauma modality (Charuvastra & Cloitre, 2008), such as physical abuse and neglect, sexual abuse, and emotional neglect is well documented (Baiden, Stewart, & Fallon, 2017; Smith, Kouros, & Meuret, 2013). Ford and Gómez (2015) conducted a systematic review of research results about the association between history of traumatic experiences, abuse, and family violence with NSSI. Their most important findings are that traumatic experiences precede the emergence of symptoms of post-traumatic stress disorder (PTSD), as well as symptoms of dissociative disorders (DD), these in turn, contribute to the emergence of both NSSI and suicidal ideation and attempt, where emotional dysregulation, as part of the symptomatic complex, is the key factor that explains the emergence and maintenance of these self-destructive behaviors. NSSI is a predictor of suicidal intent, so vulnerable adolescents who self-injure and, who additionally suffer symptoms of depression, should be considered as a greater risk population presenting suicidal ideation and attempt (Taliaferro & Muehlenkamp, 2014).
Additional early adversity circumstances have been identified as risk factors for presenting NSSI, however, according to the American Psychiatric Association (2013), they are not considered strictly traumatic in nature. For example, some research results with adolescents have shown an association between NSSI and parental absence (Trujillo & Servaty-Seib, 2017), poor quality relationships with parental figures (Tschan, Schmid, & In-Albon, 2015; Di Pierro, Sarno, Perego, Gallucci, & Madeddu, 2012), and lack of social support (Christoffersen, Møhl, DePanfilis, & Vammen, 2015). Attachment is a key concept here, it is understood as a deep and enduring emotional bond that connects one person to another across time and space (Ainsworth, 1979). A child’s attachment to its caregiver is a source of security when he/she experiences discomfort or threat. The caregiver’s responsive pattern can help to regulate the child’s emotional states, so he/she can develop a secure attachment pattern. On the other hand, an inconsistent response pattern or a lack of response from the caregiver can lead to an insecure attachment pattern (Bowlby, 1970) and consequently to difficulties in emotion regulation ([DER]; Linehan, 1993).
Associations between an insecure attachment pattern and NSSI have been described by some empirical evidence. For example, Molaie et al. (2019) found in a sample of adult psychiatric inpatients that preoccupied attachment was associated with lifetime NSSI, but emotional pain partially mediated the relationship between that dysfunctional attachment pattern and NSSI. In the same way, with a longitudinal research design, Gandhi et al. (2019) found that dysfunctional attachment between the adolescents and his/her mother was associated with greater NSSI frequency, which was mediated by increased rates of identity confusion. Meanwhile Jiang, You, Zheng, and Lin (2017) found that self-report of quality of attachment (QOA) with parents mediated by self-compassion allowed to distinguish teenagers with history of NSSI episodes. All those results show that an insecure attachment pattern with significant others increase the likelihood of engaging in NSSI or could maintain it. Despite the importance of these findings, currently studies in this regard are scarce, particularly with adolescent population.
Objectives and hypothesis
This research sought to describe the risk profile for NSSI on a sample of adolescents who received services for vulnerable population in NGO’s. Our specific objectives were as follows: 1. to describe their demographic and clinical characteristics as well as NSSI frequency, we compared such characteristics by beneficiary type: internal beneficiary (IB) versus external beneficiary (EB); 2. to explore the predictive relationship of NSSI with depression, DER, and suicidal ideation; 3. to compare the average scores on administered measures based on a) QOA and b) NSSI presence/absence.
Evidence shows that NSSI prevalence is higher on inpatient versus outpatient samples, so coupled with greater instability in the relationship with their attachment figures, compared to EB, we consider to IB as a more vulnerable population and we hypothesized that they will report higher scores in all administered measures. Meanwhile, given that there have been found clear and strong associations between NSSI and the concurrent measures, we expected to replicate that results to find the best predictors of NSSI for this population. Given the associations between an insecure attachment and NSSI, we hypothesized that adolescents with positive QOA will get lower scores. Finally, we expected that adolescents without significant and recent NSSI pattern, will get lower scores in administered measures.
Method
Design of the study
This was a cross-sectional, correlational, and prospective study (Hernández Sampieri, Fernández-Collado, & Baptista Lucio, 2014).
Subjects
A convenience, non-probabilistic sample of 255 adolescents aged between 11 and 15 (average age 13.24; ± 1.81) of both sexes (45.5% women) participated. They were beneficiaries for at least three months of one of six NGO’s, institutions of civil society that provide assistance services to children suffering from psychosocial vulnerability and risk factors that included exposure to family and community violence, parental neglect, trauma, marginalization and poverty. 181 (71%) participants were categorized as IB, since they resided on their institution facilities, where they received basic services such as feeding, shelter, and education, in addition to medical, psychological, pedagogical, and legal assistance. IB maintained little or no contact with their family. The remaining group (n = 74, 29%) was categorized as EB, since they received assistance services in one of these institutions, but they resided in family home, whose members were in charge of basic needs and formed the primary reference group for these teenagers. The average schooling years for the sample was 7.24 (+ 1.78), corresponding to the first grade of junior high school.
Places
Through a non-probability sampling, six NGO’s based in Mexico City were chosen: Casa de las Mercedes I.A.P. (N = 15, 5.8%), Hogares Providencia I.A.P. (N = 22, 8.6%), Ednica I.A.P. (N = 48, 18.8%), Internado Infantil Guadalupano I.A.P. (N = 81, 31.7%), Casa Alianza I.A.P. (N = 49, 19.2%), and Yolia A.C. (N = 32, 12.5%), the latter with alternate headquarters in Chignahuapan, Puebla (N = 8, 3.1%). Participants were recruited between October, 2018; and August, 2019.
Measurements
Inventory of Statements About Self-Injury (ISAS-I. Klonsky & Olino, 2008). The ISAS is a questionnaire of public domain; the first part evaluates the lifetime frequency of 12 modalities of NSSI. Participants are asked to estimate the number of times they have performed each behavior. With seven additional items, contextual elements of a qualitative nature are evaluated, such as age at onset, the experience of pain during episodes, the presence of witnesses, etc., Klonsky and Glenn (2009), and Klonsky and Olino (2008) reported data of excellent internal consistency for ISAS-I (α = .84) and adequate test- test reliability (.85). Marín-Tejeda (2017) carried out the adaptation of ISAS-I to Mexican Spanish, with a report of adequate psychometric properties: discrimination capacity through contrasted groups (t from -6.31 to -1.96), factor analysis with presence of four components (59.41% of explained variance), and analysis of internal consistency with Cronbach alphas from .836 to .4. We reported the total ISAS-I score (lifetime frequency), the score of each factor, and two mutually excluding scores: a) the non-significant NSSI pattern (sum of scores of factors 1, 3 and 4, and/or score of four or less in factor 2 and/or more than a year of the last episode); and b) the significant and recent NSSI pattern (minimum score of five in factor 2 in the last year).
Beck Depression Inventory II (BDI-II. Beck, Steer, & Carbin, 1988). It consists of 21 items that assess the severity of depression symptoms, which have the phrase listing format so that the interviewee is asked to choose the sentence that best describes their emotional state during the last two weeks (Likert-type scale from 0 to 3 points). González, Reséndiz Rodríguez, and Reyes-Lagunes (2015) adapted it to Mexican population with university students; they reported data of high internal consistency (α = .92), and positive correlations with concurrent measures of depression (r = .65) and anxiety (r = .71). The latent structure was explored with principal components analysis (PCA); additionally, authors compared different structures using confirmatory factor analysis (CFA) techniques. They found a three-factor structure: negative attitude, performance difficulties, and somatic elements. Authorization was obtained from one of the authors of this adapted version for use in this research.
Difficulties in Emotion Regulation Scale-Spanish Version (DERS-E. Gratz & Roemer, 2004). The original scale consists of 36 items, which measures difficulties in emotion regulation. It is made up by six factors: non-acceptance, goals, impulses, awareness, strategies, and emotional clarity. Preliminary studies indicate an internal consistency of .93 and reliability with Cronbachʼs alpha greater than .8 for each subscale. For this research, Spanish adaptation for adolescents (authorized by the original author) was used (Marín-Tejeda, Robles García, González-Forteza, & Andrade-Palos, 2012); a first CFA showed that the data did not replicate the original six-factor structure, thus an exploratory factor analysis (PCA) was carried out. Results showed that the data adjusted with a 24 items and four factor model, which was corroborated with a second CFA (χ2 = 259.729, df = 230, p > .05). Cronbach’s alphas for each factor ranged between .85 and .68. Significant estimates of validity through contrasted groups and correlation with concurrent measures were obtained.
Roberts Suicidal Ideation Scale (CES. Roberts & Chen, 1995). It consists of four items (of public domain), with which the frequency of thoughts and affects related to the intention of committing suicide is explored. The interviewee is asked to indicate on a Likert-type scale of four response options, the number of days of the last week in which he has experienced such internal states. It is a widely used instrument with Mexican students (Córdova-Osnaya & Rosales-Pérez, 2016). However, in our country, at least two different versions are used. For this research, the four items of the original instrument were integrated, given the recent report of its adequate psychometric properties: internal consistency of .76, a single factor that explained 63.4% of variance, and data of adequate predictive and convergent validity (Rosales-Pérez, Córdova-Osnaya, & Cortés-Granados, 2016).
Additional Data Questionnaire. Instrument created for this research. Designed as an Excel file to be individually administered to the mental health staff of each NGO, who answered the seven items that compose it based on: a semi-structured interview, the institutional record and structured response options. The purpose was to obtain objective information (to avoid social desirability) about the background of each participant, particularly: type and number of traumatic experiences, legal background, history of mental health treatment, psychiatric diagnoses, affiliation time to the institution, and quality of the relationship with the attachment figure (with identification of such person, family, or not); the question about the latter topic was: “Indicate the quality of relationship that the minor maintains with his main reference figure”. Consider the people who visit him at the institution facility or whom the child visits or with whom he lives. There were four categorized answers: 1. Good, it helps the child, with emotionally positive impact, 2. Bad, it damages the child or negatively impacts their emotional state, 3. Indifferent, irrelevant emotionally for the child, it doesn’t change the child’s emotional state; and 4. Without any attachment figure, when the child has no relationship with his family nor receives visits from other people (see supplemental material).
Procedure
Group administration of measurement tools on institutional space and schedules was held, plus a questionnaire of demographic data (age, sex, primary figure, schooling years of the adolescent and of his/her mother’). In the case of participants who did not answer all the questions, who were unable to read and write, or who didn’t understand the questions, the survey implementer individually read the items in the instrument and noted the respondent’s answers; if the interviewee were still unable to answer or to understand the questions, their questionnaire were invalidated. Subsequently, additional information was obtained from each participant through a semi-structured interview with each NGO’s mental health department staff, who answered the Additional Data Questionnaire.
Statistical analysis
A regression analysis was performed with a stepwise method, with Significant and Recent NSSI as the dependent variable and, according to the degree of association previously reported (Marín-Tejeda, 2013), predictors were entered with the following order: depression, DER, and suicidal ideation. Four groups were formed based on QOA and the average scores of the measurements were compared with an ANOVA. Three groups were formed based on NSSI presence/absence: 1. no NSSI episodes, 2. non-significant NSSI, and 3. significant and recent NSSI. The average score of concurrent measures were compared with an ANOVA. Differences between IB versus EB were determined in all the measures with a t of Student. Chi2 was used for categorical variables. Any result at the level of p < .05 was considered significant.
Ethical considerations
Study’s purposes were explained to NGO’s authorities and approval was obtained; subsequently, they signed the consent as tutors of the minors. Later, study’s purposes were explained to the adolescents and the corresponding signed informed consent was requested. Participation was voluntary and none of them refused to collaborate. In a subsequent session, feedback was provided to the mental health personnel of each NGO about institutional and individual outcomes, in addition to providing a list of children with high-risk profiles.
Results
Comparison of demographic and clinical characteristics by NGO beneficiary type
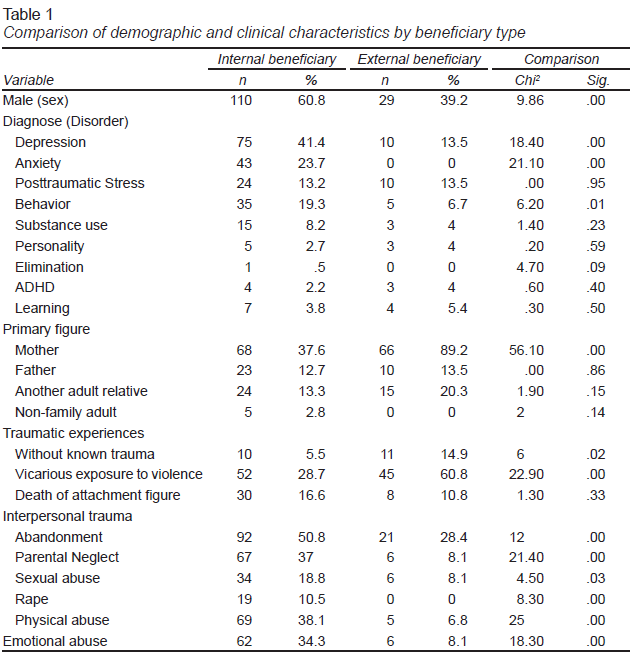
44.7% of participant’s mothers had secondary education as the maximum level of education (33% were unaware of this data); therefore, the socioeconomic extraction of the sample was considered low. A comparative summary of demographic and clinical characteristics of internal versus external beneficiaries is presented in Table 1. It shows that among IB’s, the presence of men predominates. About 90% of EB identified to their mothers as the main reference figure, contrary to IB, whose proportion in this sense was significantly lower. Although the proportion of trauma victims is relatively equivalent for both types of beneficiaries (94.5% and 85.1% respectively), IB suffered more traumatic experiences in all reported modalities, except for the death of the attachment figure, which was equivalent for both types of beneficiaries; and vicarious exposure to violence, the latter with higher reported prevalence for EB. Interpersonal trauma modalities, commonly inflicted by an attachment figure and with a more severe psychopathological consequences, were reported with higher prevalence for IB. Regarding the assigned psychiatric diagnoses, there was a higher prevalence of depressive disorders, followed by anxiety, behavior, and post-traumatic stress disorders. Compared to EB, the proportion of IB who were given these diagnoses were significantly higher, except for post-traumatic stress.
The average affiliation time to the corresponding NGO was 39.8 months (± 31.1), with a statistically significant difference (t = -5.7; p < .5) between IB (M = 32.1, ± 24.9) and those from EB (M = 58.16, ± 36.5). 58.6% of IB received psychological treatment, while 24.3% of them were beneficiaries of both psychological and psychiatric care. In contrast, 74.3% of EB did not receive any mental health care, a difference that was statistically significant (Chi2 = 58.6). On the other hand, in 32.5% of IB’ cases, there was an ongoing legal process due to the referred experiences of victimization and trauma, while this was the case in only 1.3% of EB (Chi2 = 24.4, p < .001).
Comparison of NSSI frequency by NGO beneficiary type
Regarding the measurement of self-injury, the average ISAS-I lifetime score for the complete sample was 33.1 (± 146. 4). Almost half of participants reported no NSSI episodes (42%, n = 107), while 16.9% reported a non-significant NSSI pattern (four or less episodes), therefore, 41.1% indicated that they had repeatedly practiced self-injury with at least five episodes. 57.6% of adolescents reported episodes in the last year, while 35.6% indicated a significant pattern according to the DSM-V criteria (American Psychiatric Association, 2013), with at least five episodes in the last year. The average score for men in ISAS-I was 42.7 (± 191), and for women it was 21.6 (± 57.7). Among adolescents who reported episodes of NSSI, the most common modalities in order of frequency were: banging/hitting self (69.5%), cutting (57.4%), interfering with wound healing (44.5%), carving (43.9%), biting (39.1%), and sticking self with needles (34.4%), while the least frequent was rubbing skin against rough surfaces (12.1%).
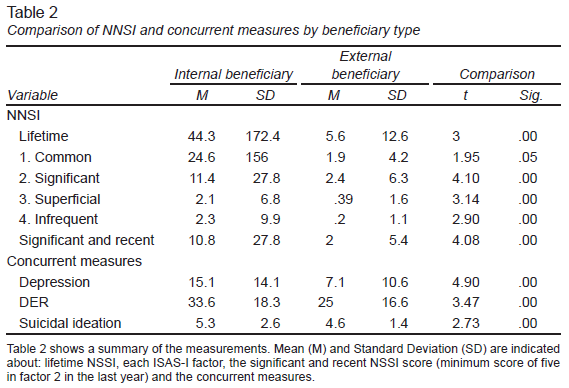
Regarding administered measures, IB presented significantly higher scores compared to EB, with at least one standard deviation of difference in depression, DER and suicidal ideation. Regarding Self-Injury, IB also obtained significantly higher scores on three factors of ISAS-I: factor 2, significant self-injury (for the latter, including the recent pattern with episodes in the last year and a minimum score of five); factor 3, superficial and factor 4, infrequent, except in factor 1, common self-injury. Table 2 presents a summary of these results.
Predictive relationship of NSSI with depression, DER and suicidal ideation
A regression analysis was performed with stepwise method, with significant and recent self-injury as target variable, predictors were entered as follows: depression, DER, and suicidal ideation. The model showed that depression was the unique predictor (R = .34, R2 = .12, adjusted R2 = .117).
Comparison of administered measures based on QOA
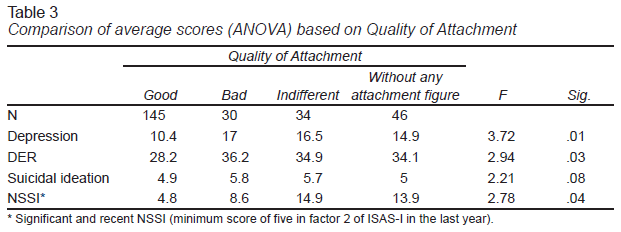
The mental health staff of each NGO identified the main person or persons who maintained a relationship with the adolescent. Results are: 134 adolescents maintained contact with their mother (52.5%), 66 with a brother (25.8%), 44 with a non-familiar adult (17.2%), 33 with his/her father (12.8%), 26 with one or both grandparents (10.1%) and 25 with an uncle (9.7%), while 46 (18%) of them did not maintain contact with any family member nor receive a visit from any other adult. The NGO’s mental health staff typified the QOA in four possible variants: good, bad, indifferent, and without any attachment figure, four groups were formed based on that classification and the average scores of administered measures were compared with an ANOVA; results are shown in Table 3. We can see that general comparison was significant, which could mean that compared to the other QOA modalities, adolescents with positive QOA obtained significantly lower scores, except for suicidal ideation. However, Tukey post-hoc test was non-significant and found no consistent differences between groups.
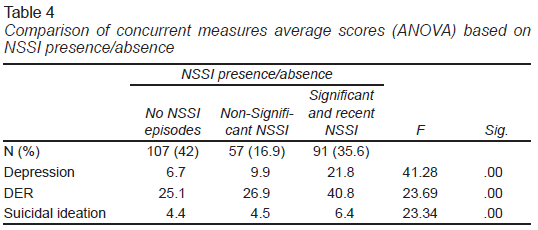
Comparison of concurrent measures based on NSSI presence/absence
Three groups were formed based on NSSI presence/absence: No NSSI episodes (ISAS-I lifetime score of zero), Non-Significant NSSI (sum of scores of factors 1, 3 and 4 and/or score of four or less in factor 2 and/or more than a year of the last episode); and Significant and Recent NSSI (minimum score of five in factor 2 in the last year). The average score of concurrent measures were compared with an ANOVA; results are shown in Table 4. We can see that the comparison between groups was significant, and with a Tukey post-hoc test we found that the only significant difference was between the group with significant and recent NSSI pattern and the other two groups. Differences between the other subgroups: without NSSI episodes versus non-significant NSSI were no significant for all the concurrent measures.
Comparing the three groups formed by NSSI presence/absence, a final Chi2 test was performed to study the frequency of assigned psychiatric diagnostics by the mental health staff of NOG’s. Results showed that participants with Significant and Recent NSSI pattern were diagnosed more commonly with a depressive (Chi2 = 37.55, p = .00) and/or anxiety disorder (Chi2 = 7.35, p = .02).
Discussion and conclusion
Demographic and clinical characteristics
Participants suffered from a set of adverse life circumstances, mainly poverty, trauma experiences, extraction from violent social contexts, as well as suffering from psychiatric disorders, particularly depression, anxiety, trauma, and behavior disorders, all of them associated with the presence of NSSI. The same risk factors have been reported with both multicultural (Bruffaerts et al., 2010), international (Kaess et al., 2013), and Mexican samples (Ulloa-Flores et al., 2013). Those authors included: low socioeconomic extraction, sociocultural context permeated by marginalization, violence and crime, young mothers at the time of birth, dysfunctional family dynamics, absent, disabled and/or harmful attachment figure, delinquent behavior and/or drug use in one or both parents, and numerous presence of brothers, many of them were in fact the reason for participants affiliation to his/her NGO.
The provided care profile by NGO’s is characterized by relatively long processes (mean attention time little more than three years), being more long-lasting for the subgroup of community, apparently contradictory data but that it may be due to the greater psychosocial instability of IB, who, on the other hand, received a greater proportion of legal and mental health care. However, given the high prevalence of psychopathology and trauma, it is clear that existed under attended issues. Commonly, NGO’s have a large population of beneficiaries, but limited financial and human resources, thus, to respond to demand volume, the mental health staff often chooses conducting psychoeducational group interventions, which can be very efficient to work with EB, but may be insufficient for IB.
The psychopathological profile found in this study is very similar to that described by Ulloa-Flores et al. (2013), with higher prevalence of mood, anxiety, and behavior disorders. However, compared to their work, we found a significantly lower proportion of substance use disorders, where the latter may be due to two factors: our participants had a lower age range, additionally to being beneficiaries of preventive and intervention programs for addictions in NGO’s facilities. Another substantial difference consists in the identification of post-traumatic stress as a prevalent diagnostic entity, which, unlike the referred disorders, it was found in an equivalent proportion among both beneficiary types, which is explained by the high exposure to trauma in all participants (higher than 80%).
Regarding comparisons between IB versus EB, we found support for our first hypothesis: IB’s are a more vulnerable population. The profile of IB included: adolescents were mostly male, had higher prevalence of psychiatric disorders, higher scores in all administered measures, and a higher proportion of severe traumatic experiences, mainly of interpersonal nature: abandonment of attachment figure, parental neglect, physical and emotional abuse, which according to Kagan et al. (2014), such experiences can be attributed as complex trauma, of an interpersonal nature and with a greater and more lasting negative impact (Charuvastra & Cloitre, 2008). On the contrary, for EB, the most common traumatic experience was vicarious exposure to violence, not as a primary victim nor perpetrated by the attachment figure, a fact that may explain the lower degree of impact in terms of associated psychopathology and less severe NSSI profile (Spinazzola et al., 2014; Kagan, 2006).
Based on those antecedents, we consider that the main differences that can explain the higher risk profile of IB compared to EB may consist on two related factors: the mostly interpersonal nature of traumatic experiences, and, therefore, the higher negative impact on QOA between the minor and his/her attachment figure. In fact, some authors such as Kaess et al. (2013) had already concluded that it is feasible to identify subgroups of NNSI perpetrators based on the nature of adverse life experiences, which influence both the frequency and severity of episodes.
Predictive relationship of NSSI with concurrent measures
According to Ford and Gómez (2015), and Auerbach et al. (2014), the adverse vital experiences contribute to the genesis of comorbid psychopathology and this, in turn, to NSSI. In line with this, our sample of vulnerable adolescents suffered a high prevalence of psychiatric conditions in the form of diagnoses assigned by mental health staff of NGO’s. However, we did not find support for our second hypothesis, because in terms of administered measures, we found that depression was the only predictor of NSSI, although with a smaller proportion of explained variance. Similar results have been previously reported, for example, with his sample of Mexican school adolescents, Marín-Tejeda (2013) found that depression was the main predictor with minimum predictive contribution of the DERS-E Non-Acceptance factor. Regarding suicidal ideation, Hom et al. (2018) found a discrete relationship between NSSI and this latter variable.
Our results can be attributed to two elements: 1. the lower age range of our sample; it is possible that an association between NSSI and concurrent variables are lower with younger population, but as research results shows, can be higher with the most common employed age range for studying NSSI: older adolescents and young adults samples. 2. Our cross-sectional study design; for example, with a longitudinal design, Glenn et al. (2017) showed a clearer association of NSSI with suicidal ideation. In sum, our results show that, when working with younger adolescents, it is important to directly administer at least depression measures, as well as parallelly obtain additional information to confirm a possible child’s comorbid disorder.
Comparison of administered measures based on QOA
A general comparison on average scores of administered measures, except for suicidal ideation, showed that adolescents with positive QOA obtained lower scores even on significant and recent NSSI, a fact that supports our hypothesis and, in the first instance, seems to confirm the typology of attachment patterns in two large groups: secure and insecure (Bowlby, 1970), at least for our sample of vulnerable adolescents. Even more, given the variability of identity of the attachment figure of the participants, our results adhere to Bowlby’s (1970) and Ainsworth’s (1979) postulates: the QOA established with the attachment figure is more important than the identity of the person performing this function. Therefore, we consider that a key factor in the genesis of vulnerability may involve absence, illness, instability, and/or damage by a primary attachment figure, with negative impact towards the development of psychopathology and NSSI (Kagan et al., 2014).
In the second instance, it should be noted that, with post hoc comparisons with Tukey’s test, we did not find consistent any differences among the subgroups. A possible explanation is the unequal number of participants between groups, with a larger number just for the participants with positive QOA. An example of the importance of work with a larger sample size is the study of García-Jauregui (2020), who recruited 937 Mexican schooled adolescents. She compared average scores on parental styles between subgroups classified by NSSI presence/absence, and similar to our results, the author found that minors with significant and recent pattern of NSSI obtained higher scores on negative parental styles, a difference that was not found between the other subgroups: without NSSI and non-significant NSSI.
In sum, despite the inconsistent Tukey test results obtained, and on condition of carrying additional studies, our data point that positive QOA is a protective factor against NSSI and other psychiatric conditions. Similar results had already been reported by Jiang et al. (2017), but they measured QOA between the adolescent and significant others by self-report, and unlike our results, they found that this variable was significant only regarding the parents and mediated by self-compassion. Conversely, our data seem to show that any other significant person can perform appropriately this function, although we did not explore the QOA with peers, we measured objectively the QOA by the mental health staff criteria and identified depression as another key variable. These findings are highlighted the importance of creating preventive and intervention programs for vulnerable adolescents, focusing on treating symptoms of depression, improving family functioning and the QOA with the attachment figure.
Comparison of administered measures based on NSSI presence/absence
Results confirmed our hypothesis: participants with a significant and recent NSSI pattern obtained higher average scores on concurrent measures. Data highlight: 1. when measuring NSSI, it is important to identify subgroups of perpetrators, based not only on the total ISAS-I score, but on clinical criteria that includes NSSI modality, frequency, and temporality (Marín-Tejeda, 2017); 2. on a more severe NSSI pattern underlies increased presence of comorbid psychopathology, therefore interventions must be designed just not to eliminate NSSI episodes, but to detect measure and modify the severity of comorbid psychiatric symptoms, specially related to depression and anxiety disorders, the most common diagnoses assigned by the mental health staff of NGO’s; and 3. adolescents without NSSI episodes and those with a non-significative NSSI pattern doesn’t differ on terms of comorbid psychiatric symptoms. However, the latter must be considered at risk for developing a more severe pattern.
Findings from the present study have important theorical and clinical implications. On regard to NSSI: there are subgroups of NSSI perpetrators, therefore, assessment must include not only the frequency of episodes, but additional clinical criteria such as NSSI modality, temporality, and functions; in addition to comorbid psychopathology, history of traumatic episodes, QOA, among others.
Adverse life experiences increase the risk of psychiatric conditions and NSSI. In this case, we found that depression, anxiety, behavior, and post-traumatic stress disorders were the most prevalent conditions. On the other hand, among vulnerable adolescents, it is possible to distinguish a higher risk profile from the nature of traumatic experiences they suffered; interpersonal trauma, commonly inflicted by the attachment figure was associated with significant and recent NSSI episodes and more severe psychiatric symptoms. IB, who reside permanently in a NGO were the minors with a higher risk profile: they suffered mostly interpersonal trauma, had depression symptoms and or maintained a negative/indifferent/absent QOA with an attachment figure. One of the main contributions of the present study is that, despite adversity, QOA is a protective factor against NSSI and other psychiatric condition.
Interventions designed to address NSSI with vulnerable adolescents must be based on a complete assessment, just not to eliminate NSSI episodes, but to detect measure and modify the severity of comorbid psychiatric symptoms, specially related to depression, PTSD, behavior, and anxiety disorders. Results highlighted the importance of creating preventive and intervention programs for vulnerable adolescents, especially those that focus on improving family functioning, parental practices, and the QOA between the minor and his/her attachment figure. Finally, it is crucial to support the work that NGO´s carry out to serve vulnerable populations, since, despite the extensive experience of these institutions in this type of activity, they often have limited human and economic resources.
Limitations
Several limitations should be addressed by future research. First, sample selection was not probabilistic, which makes it difficult to generalize the results. It is a cross-sectional design; therefore, an important area of opportunity is to study the predictive relationship between the variables with a longitudinal follow-up. Two of the four instruments used, specifically ISAS-I and CES in their Spanish versions, despite their good psychometric properties, have not yet enough evidence of validity because the absence of CFA. On regard to the BDI-II adapted version used for this research (authorized), authors did not indicate in their document that they have requested permission to adapt it. Since it is a scientific text, this authorization was taken for granted. One of the main variables: attachment, was not measured directly, on the contrary, the QOA was typified by mental health staff of each NGO, in this way, further confirmatory studies could cover this methodological limitation, determining more precisely the pattern of attachment and quality of it.