Introduction
The COVID-19 pandemic has impacted the world severely, with more than 9.8 million of people infected and close to 500,000 deceases registered. It has also caused an imminent psychosocial and economic crisis, along with social distancing, self-isolation and travel restrictions that reduced the workforce; it is needless to say that many jobs have been lost (Nicola et al., 2020; World Health Organization [WHO], 2020). A relevant psychosocial aspect to consider under these circumstances is the widespread fear where our moral judgments and social attitudes become harsher and more conservative (Robson, 2020). Widespread fear is a feeling of anxiety when faced with the possibility of being a victim; thus, it is possible to identify two elements of widespread fear to COVID-19: on the one hand, the emotion of fear, also defined as social anxiety, and on the other, a risk cognition of being a victim (Ruiz Pérez, 2007). Catastrophes, insecurity and several social phenomena have filled the void left by ineffective social welfare policies and are intended to be solved by institutional security that positions widespread fear as a crucial issue in the interpretation of reality (Fonseca Vindas & Sandoval García, 2006). Concerning widespread fear, among quarantine symptoms (social distancing and isolation) related to the CORONAVIRUS in a review of 3,166 papers from 24 selected, post-traumatic stress symptoms, confusion, and anger were commonly reported (Brooks et al., 2020). In a study analyzing post-traumatic stress disorder (PTSD), resilience, and social withdrawal as avoidance, it was found that avoidant coping strategies are usually used to escape direct confrontation with stressful circumstances. Wishful thinking or social withdrawal were positively associated with PTSD symptom development. A lack of social support may increase vulnerability to PTSD symptomatology (Thompson, Fiorillo, Rothbaum, Ressler, & Michopoulos, 2018). In addition, retrospective and prospective studies have found that avoidant coping increases vulnerability and PTSD symptoms (Gil, 2005; Hooberman, Rosenfeld, Rasmussen, & Keller, 2010; Najdowski & Ullman, 2009). The COVID-19 pandemic is without doubt one of the biggest challenges in modern history. This study is centered in the psychosocial perspective, which approaches studies about people and social context, the perceptions of widespread fear perceptions that communities build, considering their confidence and capability to provide community coping strategies to cope with the emerging SARS-CoV2 pandemic crisis.
These dimensions can be measured and understood as a construct called widespread fear to COVID-19, a synonym of social anxiety. This core construct has been related to several coping strategies, and to several PTSD symptoms based on PTSD DSM-5 criteria (American Psychiatric Association [APA], 2013). Widespread fear to COVID-19 is an emotional stress-related fear, usually associated to anxiety, stigmatization, and discrimination. (Person et al., 2004) described underlying anxiety about a disease with an unknown cause and possible fatal outcome, which directly precipitate psychological distress event rates through indirect outcomes, like: increased smoking rates, sedentary lifestyles, and direct acute coronary syndrome (Chávez-Valdez, Esparza-Del Villar, Ríos Velasco-Moreno & Relojo-Howell, 2019). Described widespread fear as a kind of collective fear that develops physio emotional coping strategies that enhance perception of uncertainty, unhealthier behaviors, post-traumatic stress traits, and anxiety disorders. (Person et al., 2004) warns us about empirical studies, which have shown that during serious disease outbreaks, when the public requires immediate information, there is usually a subgroup of the population that is at potentially greater risk of experiencing fear, stigmatization, and discrimination. (Chávez-Valdez et al., 2019). Suggest that there is a prevalence of post-traumatic stress traits in threatened collectives. Ruiz Pérez (2007) refers to certain coping strategies that reproduce fear in threatened communities.
Therefore, the purpose of this study is to determine the association between post-traumatic stress symptoms and widespread fear to COVID-19 Ruiz Pérez (2007) Social anxiety scale, in Spanish (Escala de Miedo Difuso) with respect to coping strategies during the contingency due to COVID-19 in the Mexican population. Hypotheses werenʼt established due to the insufficient amount of data to establish them.
The specific aims/objectives of this study were:
Explore the association between post-traumatic stress symptoms and widespread fear to COVID-19.
Determine the interaction between post-traumatic stress symptoms and coping strategies.
Explain the relationship between coping strategies and widespread fear to COVID-19.
Method
Design of the study
This was a cross-sectional, empirical, descriptive study of populations through survey research in a web-based survey platform (Montero & León, 2007) In order to make the sample as representative as possible, a non-probabilistic nationality quota sampling was carried out.
Description of the sample
The participants were enrolled through the platform Salud Mental COVID-19 (Mental Health COVID) https://www.saludmentalcovid.com/, an online positive psychology-based intervention platform designed to provide a self-applied psychological treatment to the Mexican population. The participants needed to create an account and answer the questionnaires inside the webpage before proceeding to the intervention. This study is registered on Clinical Trials (NCT04468893); and on the World Health Organization. Participants needed to answer self-informed psychometrics before having access to the intervention
https://apps.who.int/trialsearch/Trial2.aspx?TrialID=NCT04468893. The data collected for this study was taken over the months of April thru May of 2020.
Participants
At the time data was collected, a total of 370 participants answered the psychometric instruments: from them 312 were women, 58 men, one participant answered as another gender and one participant did not provide this data. The age inclusion criteria was between 18 to 70 years old, but the sample obtained was only between 25 to 40 years (M = 32.45, SD = 10.76). The educational level was middle school (n = 10), high school (n = 52), bachelorʼs degree (n = 221), masterʼs degree (n = 69), doctoral studies (n = 8), another (n = 8) and not answered (n = 2). Lastly, regarding the employment situation, 211 participants indicated that they worked, 157 were unemployed, and two did not answer.
The inclusion criteria was:
Participants with an age range between 18 years old to 70 years old (Adult, older adult).
Participants must complete and sign an online informed consent in order to be considered as a sample for current study.
To have access to a communication device with access to the internet (computer, tablet, or mobile phone).
To have a valid email address.
To have basic digital skills in the use of an operational system and internet browsing.
To understand Spanish since all the contents are in this language.
Exclusion or elimination criteria:
Participants that did not sign the informed consent.
Participants that voluntarily decided to withdraw the current study.
To have a diagnosis of psychotic disorder.
To be receiving psychological and / or pharmacological treatment during the study.
Sample size
The sample size was estimated using Cohen’s (1992) statistical power analysis method to detect significant effects of magnitude, based on the preliminary results and the average range of correlations (r), ranging from .20 to .53. In this sense, it was seen that a larger sample was not required in order to reduce the confidence interval of the estimate to a range acceptable. Cohen (1992) states that the coefficient (r) of correlation is by itself an indicator of statistical power magnitude.
Measurements
The psychometric instruments allowed a reliable measure of coping strategies, widespread fear to COVID-19, and PTSD symptoms. All instruments were validated in Mexican population by C.V.S.M.
The scales comply with adaptations that allowed the psychometric qualities of the items to be retained; additionally, a pilot study was carried out. The instruments were the following:
CIU Urban Strategies Coping Strategies Scale (Vuanello, 2006). Adapted by Chávez-Valdez and Ríos Velasco-Moreno (2018). The aforementioned scale was developed by Vuanello (2006). This tool design was based on the Inventory of Situations and Anxiety Answers (ISRA) (Miguel-Tobal, & Cano-Vindel, 2002). Situations and responses consider four factors: affective components, physiological activation, cognitive confrontation & behavioral promotion. In the reliability analysis, the scale reached a Cronbach’s alpha of .92 (Vuanello, 2006); in this study the alpha coefficient reached .91.
Widespread fear scale, in Spanish, Escala de Miedo Difuso (Ruiz Pérez, 2007). Chávez-Valdez and Ríos Velasco-Moreno (2018) adapted a new version of the Ruiz Pérez (2007) scale which measures an emotional widespread fear related to contextual violence into an adapted widespread fear to COVID-19 version. It is composed of seven items, with options of 0 = nothing, 3 = a lot. It measures widespread fear to COVID-19 in previous studies, an internal consistency of .95 was reached (Chávez-Valdez et al., 2019). In the present study, an internal consistency of .96 was obtained.
Scale of Post-Traumatic Stress Traits in the Mexican Youth Exposed to Social Violence (Pineda, Guerrero, Pinilla, & Estupiñán, 2002), validated by Chávez-Valdez, Esparza-Del Villar, & Ríos Velasco-Moreno (2020). It measures PTSD symptomatology based in the Diagnostic and Statistical Manual for Mental Disorders fourth edition (DSM-IV-TR). A 24-item self-report measure considering five PTSD criterions and a total PTSD symptomatology score. Factors were labeled as communitarian PTSD traits by the authors considering DSM-IV.TR criterions (Chávez-Valdez et al., 2020). The first factor belongs to PTSD criterion D “negative alterations in cognitions and mood.” The second factor refer to PTSD criterion B “intrusion symptoms”, third factor is related with PTSD criterion G “functional significance”, referring the fourth factor, comprises PTSD criterion C “avoidance symptoms”, and a fifth factor concerning PTSD criterion E “alterations in arousal and reactivity symptoms” (Chávez-Valdez et al., 2020). It is important to mention that the scale identifies PTSD symptoms according to PTSD criterions found in threatened collectives; it does not pretend to perform levels of severity or individual clinical diagnosis. Since it could only be done with clinical interview, the scaleʼs focus is to identify and categorize PTSD symptoms.
Procedure
The evaluation procedures include: 1. All participants who accepted the informed consent answered the scales. 2. Recollected data was exported to Excel spreadsheets in a codification format into numbers considering assumed value criteria for each scale; this process was double-checked to avoid errors. Meanwhile, SPSS files were codified to reach an adequate importation of the data into SPSS files. 3. Correlations and multiple regressions were performed. Coping strategies allowed quantifying multiple behavioral associations with PTSD symptoms. Thus, we performed multiple regressions to characterize the behavioral system among coping strategies.
Statistical analysis
The data was analyzed using the Statistical Package for the Social Sciences (SPSS), 22nd version. Univariate analysis was performed. Normality was assessed using normality tests. Partial correlations between variable dimensions were done, all tests used a level of significance of .05 and < .01.
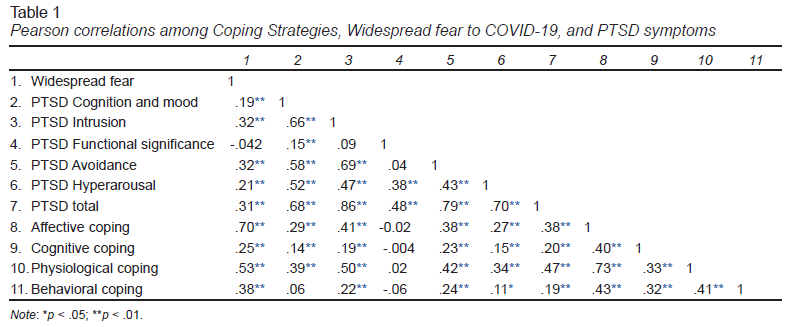
The first analysis performed was the Pearson Product-Moment Correlation including the main targeted variables (coping strategies, widespread fear and post-traumatic stress traits or criteria). Pearson correlations were calculated in order to evaluate possible extreme collinearity among variables (Kline, 2015). According to Kline, correlations of .90 are indicative of extreme collinearity and may result in non-positive definite data matrices. After wards, in a second phase, multiple regression analysis were performed. Data was included in two steps. In the first step, we entered the dependent variable coping strategies and added widespread fear. The second step was a multiple regression of PTSD symptoms predicted by the coping factors. Multiple linear correlations were calculated to evaluate multivariate collinearity (Kline, 2015) and to find what coping variables had statistically significant standardized beta values. Kline indicates that an R2 value greater than .90 reflects extreme multivariate collinearity. Tolerance and variance inflation factor indexes were calculated since tolerance values (1-R2), and all the variables showed less than .10, and variance inflation factor values (1/[1-R2]) lower than 10.0, so no multivariate collinearity was found.
Ethical considerations
This study was approved by ELPAC University of Behavioral Sciences, in Chihuahua, Mexico (Act number 2008). Psychosocial intervention divulgation was performed through participant universities websites, newspapers, and scientific media. Participants’ informed consent should be accepted before proceeding. Since the participants answered online, their data was protected in questionnaires embedded in the platform without third parties to access the data besides the researchers of this study. The participants were asked for the minimum information so identification would not be possible, no name was requested. Participants just needed an email to log in. Privacy policy can be verified at link: https://www.saludmentalcovid.com/privacy.aspx.
The platform was designed by two software engineers in collaboration with D.R.A.
Results
Associations among coping strategies, widespread fear to COVID-19 and, post-traumatic stress symptoms
Pearson correlations were analyzed among coping strategies, widespread fear, and PTSD symptoms (Table 1). None of the correlations had values of .90 of higher, indicating there is no extreme collinearity that results in a non-positive definite data matrix. Out of the 55 correlations, 47 were statistically significant, and most of them were either moderate or large (Cohen, 1992). Widespread fear to COVID-19 had the strongest correlations with affective and physiological coping. PTSD symptoms were correlated with coping strategies, stronger associations were among physiological, followed by affective strategies with intrusion and avoidance symptoms.
Associations among widespread fear, post-traumatic stress criterions and coping strategies
Cohen (1992) suggested that coefficient (r) is by itself a magnitude indicator of statistical power, states for a .10 a low effect, .30 a moderate effect, and .50 a large effect.
The strongest correlations reflected that coping strategies were affective and physiological. The relationship among affective coping strategies was direct and statistically significant to widespread fear to COVID-19, a large effect (r = .70, [p < .01]), and physiological coping strategies were direct and statistically significative with a large effect (r = .53, [p < .01]). Both behavioral (r = .38, [p < .01]) and cognitive coping strategies showed a positive or direct statistically significant moderate effect (r = .25, [p < .01]), suggesting that the principal coping strategies that the sample performed are associated to affective physiological reactions.
Widespread fear had a statistically significant correlation total PTSD score (r = .31, [p < .01]), Avoidance (r = .32, [p < .01]), Intrusion (r = .32, [p < .01]), Hyperarousal (r = .21, [p < .01], and Cognition and mood (r =.19, [p < .01]), with moderate effects in almost all the PTSD symptoms, only PTSD functional significance was non-significant.
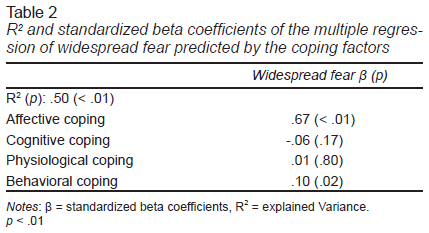
A multiple regression was analyzed with widespread fear predicted by the coping factors (Table 2). The R2 value was .50 (p < .01), meaning that 50% of the variability of widespread fear was explained by the coping factors. Only affective and behavioral coping had statistically significant standardized betas.
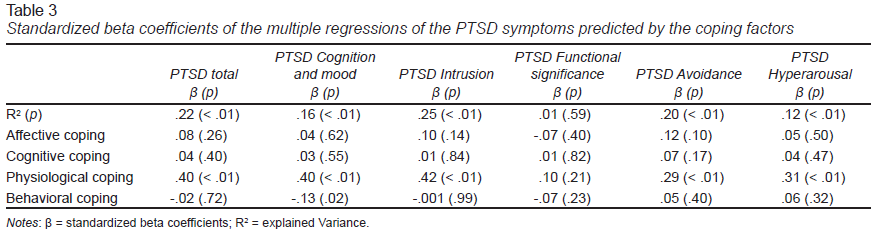
Multiple regressions of PTSD symptoms predicted by the coping factors were analyzed (Table 3). The only multiple regression that was not statistically significant was with PTSD functional significance symptom. The significant R2 values ranged from .12 (PTSD hyper arousal) to .25 (PTSD intrusion). All statistically significant regressions related to the physiological coping variable were significant. Since none of the R2 values was greater than .90, there is no extreme multivariate collinearity in the data (Kline, 2015). Tolerance values ranged from .75 to .99, and variance inflation factor values ranged from 1.01 to 1.28, indicating no collinearity in the data (Kline, 2015).
Discussion and conclusion
Our study aim was to determine the associations between post-traumatic stress symptoms and widespread fear to COVID-19 with respect to coping strategies during the contingency due to COVID-19 in the Mexican population.
During the months of April and May 2020, 1,454 participants were registered and signed an informed consent, of which 711 filled out sociodemographic data (country, city, gender, age, email, among others). Of these, 711 participants, only 654 had a Mexican birth certificate. Subsequently, several filters were applied using the provided email as a reference. When reviewing the post-traumatic stress traits scale, 555 participants completed this scale, and when comparing the aforementioned with the widespread fear scale 540 participants completed the scale also; a complete sample comprising both scales reached 394 participants. A final filter was performed adding a coping strategies scale, which defined the final sample into 370 participants.
Considering the results of the multiple regression analyzing widespread fear predicted by the coping factors a value of R2 = .50 (p < .01) was obtained. In addition, there were no statistically significant associations with the criterion G PTSD functional significance (APA, 2013) at the time data collection for this study was completed. This is crucial because, at this point, no dysfunctional performance on physical health, work, or relationships associated to the pandemic can be demonstrated. It is important to note that most people that experience difficult situations or stressors tend to cope well and do not develop PTSD symptoms since there is no perception of a traumatic event.
PTSD total symptomatology in SARS-CoV2-threatened communities was strongly predicted by physiological coping, so a strong reactive response in this communities, with a high prevalence of widespread fear to COVID-19, predicted by emotional focused coping, was a growing warning. PTSD symptomatology found in the sample and the widespread fear to COVID-19 is a relevant convergent finding. However, as a divergent finding, it also warns us about no other significant coping strategies preferred by our sample. In this case, cognitive confrontation and behavioral promotion coping strategies, which have a beneficial role to seek aid in case of a mental health pandemic outbreak, were not statistically significant by Mexican SARS-CoV2-threatened communities.
These results are in accordance with recent literature related to psychological symptoms due to the COVID-19 pandemic. In the study carried out by Germani, Buratta, Delvecchio, and Mazzeschi (2020) with a sample of 1,183 Italian adults, factors like: worrying and social fear, restlessness, and psychological maladaptation were observed. Talevi et al. (2020) suggest that during the pandemic, the general population suffered considerable psychological distress in terms of anxiety, depression, PTSD. These authors claim that these findings are also observed with severity worldwide. This aspect helps to the generalizability (external validity) of the study, an effort to engage in COVID-19’s trauma-related research.
There are other points of agreement, like associate traumatic events with coping strategies, mental health and well-being measures (Cherewick, Doocy, Tol, Burnham, & Glass, 2016). High levels of socio economic and cultural vulnerability, post-traumatic stress traits in young people, widespread fear and a variety of traumatic stressors usually impact psychosocial health and well-being (Chávez-Valdez et al., 2019).
Regarding the limitations of this study, it should be mentioned that, although 370 participants constitute a considerable sample, they do not represent still the whole circumstances of the Mexican population struggling with this pandemic. However, the authors know that this is the first study of such dimensions analyzing the pandemic effects in the Mexican population, a country where mental health services are lacking, and more epidemiological and psychology interventions should be applied (Martínez, Galván, Saavedra, & Berenzon, 2017).
Another limitation was that not enough detail of the sociodemographic characteristics of the participants was obtained. This was decided in order to maintain the anonymity of the participants, the gathered information pertained to gender, age, educational level, city, and employment status. In future studies, more detailed information of the participants will be gathered.
Additionally, our scale did not inquiere in terms of time span for the PTSD symptoms, and it is necessary for future studies to include this information to assess if the symptoms indicate PTSD or acute stress disorder. Finally, several studies indicate a comorbidity between PTSD and depression (e.g., Flory & Yehuda, 2015), and since depression was not evaluated in our study, there are limitations, for example, we cannot differentiate if the symptoms measured by the PTSD scale are better explained by depression. This limitation would also extend to other mental disorders that we did not measure in this study (e.g., anxiety, substance use).
Although participants are from Mexico, it is noteworthy that the symptoms are similar across countries, as mentioned in the studies of Germani et al. (2020) in Italian participants and Talevi et al. (2020) in Vietnam and China. More psychometric tests could have been applied to have a wider panorama of the symptomatology, such as: life quality and positive emotions, in order to observe how these areas could be affected during a contingency such as COVID-19.
Our results found that widespread fear to COVID-19 had direct effects on affective coping, while physiological coping had direct effect on PTSD symptomatology, like: cognition and mood, intrusion, avoidance, and hyperarousal.
Substance Abuse and Mental Health Services Administration (Center for Substance Abuse Treatment, 2014) indicate that delayed responses to trauma, among others, anxiety focused flashbacks, and emotional avoidance, can be indicators of more severe responses including intense intrusive recollections that continue during life span despite a return to safety. In this research, bad cognition and mood criterion showed a direct impact in physiological coping and a negative association on positive behavioral coping strategies (Center for Substance Abuse Treatment, 2014).
Also, intrusive memories or flashbacks, hypervigilance and avoidance responses in a recursive mode in a social anxious community can derive to avoidance disorders, like: substance abuse, compulsive eating disorders, and social avoidance (Kummer & Harsanyi, 2008).
Widespread fear to COVID-19 is related with emotional coping strategies and PTSD symptoms, such as: intrusion, generalized eluding or avoidance behaviors, hyperarousal and bad cognitions and mood. The current investigation warns about high physiological coping with traumatic intrusive-eluding symptomatology. We found intrusive and avoidant coping as moderator refugees to lead the pandemic crisis. These coping strategies must warn about severe reliable post-pandemic markers in several mental pathologies, including acute PTSD symptomatology evolution, as an individual diagnose or in comorbidity with mood disorders, persistent increased arousal symptoms, causing anger outbursts and hypervigilance. In the near future, if prevention is not performed, avoidance disorders, compulsive and addictive behaviors, and other dysfunctional behaviors can derive in multi pathological post-pandemic communities.