Introduction
Psychological stress is the subjective perception of a current or potential adverse environmental change (i.e., stressor), which entails a response from the individual to adapt to new conditions. Stress-generating situations are an important part of life (Golbidi, Frisbee, & Laher, 2015).
The nature of stressors is diverse. They can be physical or psychological, recognized by specific brain regions, and produce adaptative responses through activation of the autonomic nervous system and the hypothalamic-pituitary-adrenal axis mainly (de Kloet, Joëls, & Holsboer, 2005). Physical stressors—e.g., musculoskeletal trauma—activate brain areas such as the stem and the hypothalamus, while psychological stressors—e.g., normative and non-normative life events—activate the amygdala, the prefrontal cortex, and the hippocampus. When facing stressing situations, there is a quick release of norepinephrine, serotonin, dopamine, and corticotropin-releasing hormone (CRH), which promote vigilance, alertness, evaluation of the situation, and startup of coping strategies, as well as learning (Joëls & Baram, 2009).
The length of the stressor affects the response. Acute stressors trigger neural activation and release of neurotransmitters and hormones (Jöels & Baram, 2009). When the stressor lasts more (i.e., long-term), there might be maladaptive responses with consequences for the cardiovascular, the endocrine/metabolic, and the nervous systems (Golbidi et al., 2015). Long-term stress is caused by events lasting days or longer (Joëls & Baram, 2009; Epel et al., 2018). This kind of stress generates structural and functional neural changes (McEwen, 2007), which, added to an intrinsic vulnerability, favor the development or progression of mental disorders, among which those with depressive and anxiety symptoms stand out (depression and other affective disorders, post-traumatic stress disorder, generalized anxiety disorder) (Goh & Agius, 2010).
Even in normal conditions, the post-partum period implies challenges for women, who must undergo changes to adapt to the maternal role. These changes include mother-child attachment behaviors influenced by the stress level perceived during the perinatal period (Lau, 2001), which in turn depend on the mental health (personality traits, mental disorders) and on the level of support received, which when insufficient, causes a sense of loneliness (Lau, 2001; Tahirkheli, Cherry, Tackett, McCaffree, & Gillaspy, 2014; Cherry et al., 2016). The effect of stress on the mother-child attachment justifies its study during the perinatal period.
The birth of an ill child needing admission to a neonatal intensive care unit (NICU) adds more long-term maternal stress sources: mothers feel that their capacity to provide well-being and to soothe their children’s pain is negatively affected, suffer for their children’s condition, and must follow medical recommendations. Compared with fathers, in these circumstances mothers are more exposed to stress and its negative consequences (Carter, Mulder, & Darlow, 2007; Sikorova & Kucova, 2012; Doering, Moser, & Dracup, 2000). Some of the consequences include sleep disturbances, fatigue (Obregon, Litt, Patel, Ziyeh, & McCormick, 2019), and structural changes in the brain, amygdala, or prefrontal cortex, which disrupt their response to the newborn needs, thus hindering attachment (Kim, 2021).
Given the deleterious consequences of stress on the mother and on the attachment with her child (Prouhet, Gregory, Russell, & Yaeger, 2018; Muller-Nix et al., 2004), it is essential for perinatal psychiatry—focused on the clinical and research aspects related to mental health in the prenatal period and the year after delivery—to study what factors and coping skill profiles are related to the stress perceived by mothers of neonates admitted to the NICU. Prior research has shown that bad baseline mental health increases maternal stress, which in turn raises the risk of subsequent disorders such as post-traumatic stress disorder or depressive disorder, even up to one year after the child’s admission to the NICU (Hynan et al., 2015). There is no relationship between parity, multiple pregnancy, or unplanned pregnancy with the stress degree of these mothers (Palma, Von Wussow, Morales, Cifuentes, & Ambiado, 2017).
As for the influence of the clinical characteristics of neonates admitted to a NICU on maternal stress, although most studies agree that stress is not linked to the newborn’s condition (Shaw et al., 2006; Lasiuk, Comeau, & Newburn-Cook, 2013; Woodward et al., 2014; Wormald et al., 2015), a relationship of stress with gestational age, newborn cardiovascular diseases, and NICU hospitalization duration has been reported (Dudek-Shriber, 2004).
Since maternal stress has diverse negative long-term influences on the mother and her attachment to the newborn (Gorritza Pérez, Bárcenas Bellót, Gorritza Pérez, & Brito Herrera, 2013), the aim of this cross-sectional study was to assess the association of both mothers’ sociodemographic, clinical, psychological, and psychiatric factors and neonates’ clinical aspects with the severity of stress perceived by the mothers of newborns while admitted to a university hospital NICU.
Method
Design study
Cross-sectional analytical study of mothers of neonates admitted to the NICU of the Clínica Universitaria Bolivariana, Medellín, Colombia (CUB), conducted until reaching a preestablished sample size.
Description of the sample
Women aged 18 years or older with at least one child admitted to the NICU were included consecutively. The women were not under any psychological or psychiatric intervention as part of the attention during the stay of their children in the NICU. They were assessed after the first 72 hours to one week from the admission. The limit of 72 hours was determined to warrant cases with clinical relevance. Mothers who did not agree on participating or who, according to the researchers’ judgment, had cognitive or verbal communication difficulties hindering their participation were excluded.
The sample was calculated for a multivariate linear model with a maximum of six predictors for an R2 > .25. According to the curve of prediction for sample size, the minimum n should be 43 (Field, 2013). To exclude outliers, and in anticipation of contingencies, such as the withdrawal of consent, an n = 47 (10% extra sample) was defined.
Variables and instruments
A form was designed to record the mothers’ sociodemographic and clinical variables of interest.
Clinical characteristics of the neonates were also recorded. The neonates’ variables included birth weight, number of days in the NICU, preterm birth and other main diagnoses, presence of more than one admission diagnosis and death during NICU admission. We also included the Score for Neonatal Acute Physiology (SNAP II), which assesses clinical severity from least to most at a range of 0 to 165, according to physiological parameters during the first 12 admission hours (Richardson, Corcoran, Escobar, & Lee, 2001).
The mothers’ psychological characteristics were assessed with these instruments:
Perceived Stress Questionnaire (PSQ): The PSQ quantifies stress by assessing its cognitive and emotional aspects. It includes 30 items scored from 1 (almost never) to 4 (usually), in a 20-80 range, where a higher score means more stress. The PSQ allows for the classification of both baseline and current perceived stress (the latter is the dependent variable in this study) with very good concurrent validity and reliability. Baseline stress refers to the last year and current stress refers to the last days to weeks. The PSQ is to be fulfilled by the person being assessed. The free Spanish version was used (Levenstein et al., 1993).
Coping Strategies Questionnaire (CSQ)©: The CSQ has 42 items scored between 0 (never) and 4 (most of the time). It assesses seven basic styles grouped into two coping styles: problem-focused (problem solving, positive reappraisal, social support seeking) or emotion-focused (overt emotional expression, religion, avoidance, negative self-focus). The CSQ has excellent construct validity and reliability. The author granted us written consent to use the Spanish self-administered scale (Sandín & Chorot, 2003).
UCLA Loneliness Scale©: This scale has 20 items scored between 1 (never) and 4 (always) that add-up to grade the perception of loneliness from 20 to 80 (20-39 mild, 40-59 moderate, ≥ 60 severe), with very good concurrent and discriminant validity. The author of this self-administered instrument granted written authorization to use its Spanish version (Russell, 1996).
Short version of the Eysenck Personality Questionnaire-Revised-Spanish (EPQ-RS)©: The EPQ-RS validly and reliably assesses the basic dimensions of personality (extraversion, emotionality/neuroticism, and tough-mindedness/psychoticism) and includes a scale of social desirability. It contains 48 dichotomous self-administered questions allowing to assign a typical 1-99 score to each dimension. The original test is used in this study with permission (Ortega, Ibáñez, & Moro, 1997).
The current psychiatric diagnoses of interest (depressive episode, dysthymia, generalized anxiety disorder, adjustment disorder, acute stress disorder, substance use disorder) were established following the Diagnostic and Statistical Manual 5 (DSM-5) criteria (American Psychiatric Association, 2013). To increase reliability, each individual criterion of each disorder’s criteria was dichotomized as present/absent.
Procedure
Pilot
With standardization purposes, before the sample collection, one of three consultation-liaison psychiatrists assessed 10 mothers in the presence of the other two. The three of them completed the sociodemographic and clinical instruments and the DSM-5 criteria. After each interview, they discussed and resolved discrepancies.
Sample collection
A social worker reviewed from Monday to Friday the list of admissions to the NICU, verified that the mothers were ≥ 18 years-old and had at least one child admitted for more than 72 hours, and scheduled a visit with one researcher.
Besides the three psychiatrists standardized in the pilot, other five clinicians assessed the participants. In order to standardize them, these five were distributed among the first three psychiatrists for a similar exercise to that of the pilot with the first 15 mothers in the study (five mothers by team). The information included in the study for these 15 participants was the one obtained by each of the three psychiatrists standardized in the pilot.
Having eight clinicians favored the availability of researchers for scheduling interviews at different times at the participants’ convenience, thus avoiding the risk of losing cases.
During each interview, the clinicians collected the mothers’ sociodemographic and clinical information and assessed them with DSM-5 criteria. The mothers fulfilled the self-administered instruments after an explanation. To fulfill the CSQ baseline score the participants were asked to consider the last year, which includes the months of pregnancy, and the time since birth for the current stress score. Neonates’ clinical data were obtained from the electronic charts.
When a psychiatric diagnosis or other mental health issue were identified, the participant mother was derived for the corresponding clinical attention, which was not part of the current study.
Statistical analysis
Sample description and bivariate analyses
Discrete variables are reported in absolute frequency and percentage. The diagnosis of normality of continuous variables was performed with Shapiro-Wilks’s test; normal variables are reported with mean ± standard deviation (SD); the non-normal, with median and interquartile range (IQR).
The difference in the amount of baseline stress according to the CSQ, with respect to current stress (i.e., the dependent variable in this research), was determined with the t-test for related samples. The correlation of the study variables with current stress was analyzed with Pearson correlation test (normal continuous variables), Spearman correlation test (non-normal continuous variables), and point-biserial correlation test (dichotomous variables). Significance for these and for multivariate analysis was set at .05.
Multivariate analysis
Those variables significantly correlated with current stress were used for a linear model. To avoid distorting redundancies and to obtain a parsimonious model, in the case of the various psychiatric disorders, the bivariate analyses were examined to define (if several were significantly correlated with the current stress) which diagnosis to use for the model. Before creating the model, outliers (cases with standardized residual > 3) were excluded.
Since it was the most conservative, the backward method was chosen to define the predictor variables retained by the model. The assumptions of linear regression were verified: independence of residuals by Durbin-Watson statistic (DW ≈ 2); absence of multicollinearity according to the average in the variance inflation factor (VIF ≈ 1); homoscedasticity according to the patterns of the scatterplot; and normality of residuals according to observation of the histogram and the Q-Q plot. A 1,000-sample bootstrap was planned for the coefficient statistics if either of the last two assumptions was not met. The model summary is reported (R2, F-statistic, and p-value), as well as the coefficients of its component variables with their statistics.
Ethical considerations
This research was approved by the Health Research Ethics Committee of Universidad Pontificia Bolivariana, Medellín, Colombia (UPB) and the participants signed a written informed consent after resolving doubts with one of the researchers.
Results
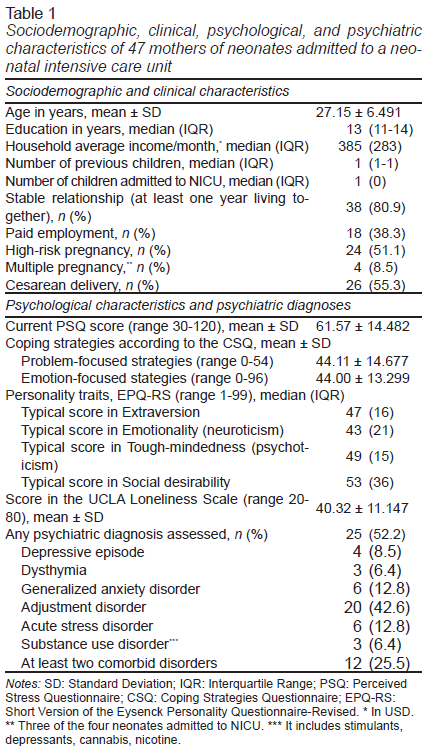
Three candidates were not included in the study because they did not consent. Table 1 shows sociodemographic, clinical, and psychological characteristics of the 47 study participants, as well as their mental disorders prevalence. The mothers’ average income in USD was relatively low; most of them had a stable relationship (for at least one year); and more than half had a high-risk pregnancy and cesarean delivery.
The average current CSQ score (stress after delivery), 61.57 ± 14.482, was higher than the baseline score, 51.11 ± 14.383, implying an increase of 10.47 points (t 5.861, df 46; p<.001). Almost one-half of the participants (23% or 49%) had a moderate or severe perception of loneliness. Although the score in the problem-focused and emotion-focused coping strategies was similar in absolute numbers, the score in the former was actually higher, as its scoring range was narrower (Table 1). There was no predominance of any particular personality trait.
More than one-half of the sample had a psychiatric disorder and one-quarter had at least two. The most common was the adjustment disorder, in 20 participants (42.6%), which was mixed with anxiety and depressed mood 9/20 (45.0%), with depressed mood 8/20 (40.0%), with mixed disturbance of emotions and conduct 2/20 (10.0%), and with anxiety 1/20 (5.0%). In 19/20 (95.0%) cases, the adjustment disorder was related to the health of the hospitalized children. Seven mothers (14.9%) had a depressive disorder (depressive episode or dysthymia).
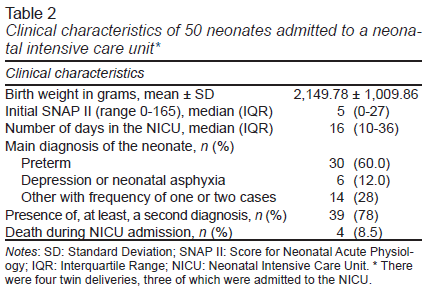
Table 2 shows the neonates’ characteristics evidencing their clinical status severity. Most of them were born prematurely and had more than one active diagnosis justifying their admission.
Bivariate analyses
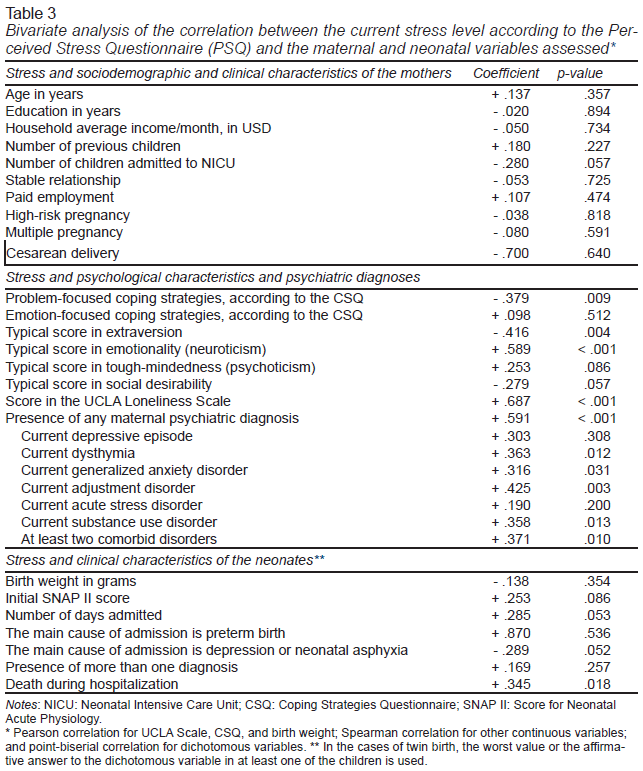
Several psychological characteristics and psychiatric diagnoses correlated with the current stress level, while the mothers’ sociodemographic aspects or the mothers’ or neonates’ clinical characteristics did not (Table 3). The perception of loneliness displayed the highest direct correlation (the greater the loneliness, the greater the stress). Four out of six mental disorders correlated in a direct way with stress. In fact, the “presence of any maternal psychiatric diagnosis,” which summarizes psychiatric morbidity, reached the second highest correlation among all significant variables and the highest correlation among psychiatric disorders. Conversely, the use of more problem-focused coping strategies and less extraversion was associated with lower stress (inverse correlation).
Multivariate model
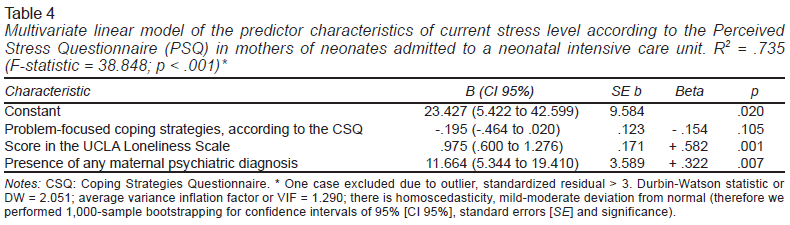
The five significant variables in the previous analysis were inputs to the multivariate model. The variable quantifying the presence of any psychiatric disorder was used because it synthesizes the disorders assessed in this sample, where comorbid psychiatric disorders were common, and because it had the highest bivariate correlation. The resulting model retained three of the initial variables and explains 73.5% of the stress variance (F 38.848; p<.001), with the level of loneliness perception as the most relevant aspect, followed by psychiatric morbidity. Problem-focused coping strategies might be relevant (i.e., are retained in the model) as protective against stress (Table 4).
Discussion and conclusion
We modeled the relationship of sociodemographic, clinical, psychological, and psychiatric characteristics with psychological stress in mothers of neonates admitted to the NICU of a high complexity university hospital in Colombia. Most of the participants were low income, high-risk pregnancies and deliveries were predominant, and psychiatric disorders were frequent.
Compared to the baseline, mothers of neonates admitted to the NICU experienced a significant increase in stress. Although various psychological and psychiatric characteristics were related to stress in the bivariate analyses, neither the sociodemographic and clinical aspects of the mothers nor the clinical characteristics of the neonates were related to stress in the multivariate model.
In the multivariate model, explaining more than 70% of the variance in stress, it is striking how stress worsened, firstly, by the perception of loneliness and, secondly, by any of the mental disorders assessed, while none of the personality traits was retained. Problem-focused coping strategies are important because are retained in the model.
A high prevalence of at least one psychiatric diagnosis was observed, being adjustment disorder the most frequent, even above depressive episodes, that are more common in the post-partum period under normal conditions (Shorey et al., 2018), and above other disorders with symptoms of anxiety. Likewise, a significant number of mothers had at least two comorbid disorders. As for personality traits, the median scores were close to the typical population score (Ortega et al., 1997). This pattern of psychiatric disorders and personality traits is consistent with the type of sample: mothers from general population with children admitted to a NICU.
It is worth mentioning the relationship between the presence of any maternal psychiatric diagnosis and stress severity. In fact, previous studies have reported that several psychiatric disorders, such as those related to stress/adjustment (Shaw et al., 2006; Vanderbilt, Bushley, Young, & Frank, 2009; Lefkowitz, Baxt, & Evans, 2010; Jubinville, Newburn-Cook, Hegadoren, & Lacaze-Masmonteil, 2012), mood (Lefkowitz et al., 2010; Roque, Lasiuk, Radünz, & Hegadoren, 2017; Gönülal, Yalaz, Altun-Köroǧlu, & Kültürsay, 2014; Segre, McCabe, Chuffo-Siewert, & O’Hara, 2014), and anxiety (Carter et al., 2007; Ionio, Mascheroni, Colombo, Castoldi, & Lista, 2019; Roque et al., 2017) are common among mothers with children admitted to a NICU, thus increasing stress and decreasing quality of life.
The above-mentioned highlights the importance of timely diagnosing and treating mental disorders during pregnancy and postpartum, in order to reduce the negative consequences on the mother-child binomial. In this sense, the positive effects of involving mental health professionals in perinatal care teams should be emphasized (Austin, 2003; Olhaberry et al., 2013).
Since the perception of loneliness is the most important factor for stress, providing psychosocial support to the mothers is key (see, beta value in Table 4). The efforts of the health and social services staff should be directed not only to the physical newborn recovery, but also to provide the mother with formal psychosocial assistance, guidance and appropriate information, and to identify partners, relatives, or friends who can support her. Offering opportune information and encouraging family participation in childcare reduces stress (Heuer, 1993).
In an indirect way, previous studies have identified loneliness as a risk factor for stress in mothers of neonates admitted to a NICU, since it is common in samples with a predominance of single, separated, or widowed women with no social support network (Carter et al., 2007). In fact, an inverse relationship has been suggested between the perception of support and maternal stress, with positive perceptions being associated with lower stress levels (Montirosso, Provenzi, Calciolari, & Borgatti, 2012; Tandberg, Sandtrø, Vårdal, & Rønnestad, 2013).
In contrast to these two risk variables, problem-focused coping strategies could be protective in this stressful situation. The healthcare staff should promote easy-to-adopt measures, such as the analysis of possible solutions to specific difficulties, decision-making, and implementation of action plans by the mothers, as well as structured problem-solving programs (Lasheras, Farré-Sender, Porta, & Mestre-Bach, 2020). While this finding is not significant, it is relevant within the explanatory model, hence the importance of conducting studies on the specific role, and on interventions, over coping strategies in this population group.
Personality traits were not retained in the multivariate model. This can be explained by the fact that participants did not have particularly dysfunctional traits, since the sample belonged to the general, nonclinical population of mothers. It is important mentioning that, for example, a high degree of neuroticism is a determining factor for stress in samples with a significant trait of this personality factor (de Jong, van Sonderen, & Emmelkamp, 1999). Studies on other models of personality have shown that harm avoidance, novelty seeking, and self-transcendence are also related to stress (Carter et al., 2007).
Unlike the perception of loneliness and the presence of psychiatric disorders, the mother’s baseline demographic and clinical variables did not explain the stress, suggesting that current mental condition and psychosocial aspects specific to the situation (need for support and sense of loneliness) are the determinants of the current stress severity. Moreover, other studies report that family support and appropriate staff guidance can prevent maternal stress (Varma, Nimbalkar, Patel, & Phatak, 2019).
The clinical characteristics of the neonates were not associated with maternal stress either. Literature is inconclusive in this regard. While several studies report that these characteristics do not increase stress (Shaw et al., 2006; Lasiuk et al., 2013; Woodward et al., 2014; Wormald et al., 2015; Jee et al., 2012), it has been reported that gestational age or cardiovascular diseases yield to the perception that the newborn has an altered appearance and behavior and, therefore, increases stress (Dudek-Shriber, 2004), Future studies should delve into the relationship between specific clinical manifestations, the perception that they trigger and stress.
The main limitation of this study is its cross-sectional design. A study with a long-term follow-up could shed light on the effects of stress on the mother-child binomial. Clinical trials assessing the impact of psychosocial interventions focused on variables related to stress, over the stress perceived by mothers of newborns admitted to the NICU are also lacking. Besides supporting focused interventions, these trials would increase the clinical understanding of the causal model.
Considering that all the participants had their children admitted to the same NICU, it was not possible to assess whether different dynamics in other units influences the mothers’ stress. However, the various demographic, psychosocial, and health aspects of mothers and children that could potentially explain stress were considered, enabling a parsimonious explanation of more than 70% of its variance.
In conclusion, mothers of neonates admitted to a NICU have a high prevalence of mental disorders, revealing the need for active case finding; the presence of mental disorders and loneliness increase the severity of stress. Interventions should include timely treatment of mental disorders, adoption of strategies for effective social-family support, and implementation of coping measures specific to the difficulties encountered by the mothers.