Introduction
Quality of life is a broad and polysemic construct that aims to assess the degree of well-being of individuals through the reflection of health effects in the physical, psychological, emotional, and social fields (Skevington, 2002). It is considered a resource for the use of care and health treatment outcomes, and is defined by the World Health Organization (WHO) as “an individual’s perception of their position in life in the context of the culture and value systems in which they live and in relation to their goals, expectations, standards and concerns” (Olsson & Nilsson-Wikmar, 2004; World Health Organization [WHO], 1994).
During pregnancy, women go through changes that can affect their quality of life. Their bodies undergo modifications to provide the conditions for embryo implantation and fetus development. However, the changes are not just physiological, as they affect other spheres, such as the psychological and social (Abreu, Brandão, & Torres, 2019).
From a psychological point of view, the process of constitution of the maternal identity, defined through an idealized image of the self as a mother and also of the child as a child, occurs before birth (Cunha, Santos, & Gonçalves, 2012). Based on this construction, the development of a sense of responsibility results in changes in family and social relationships (Giordani, Piccoli, Bezerra, & Almeida, 2018).
In the obstetric context, unplanned pregnancy is a factor associated with gestational depression, financial difficulties, and consequences for personal and professional life (Lima, Tsunechiro, Bonadio, & Murata, 2017). Furthermore, while the pregnancy trimester progresses, there is a worsening in sleep quality due to, for example, muscle pain, shortness of breath, and heartburn (Silva, 2017).
The experience of pregnancy is also influenced by personal life circumstances, such as marital status and socioeconomic conditions, as well as cultural beliefs and values. Sociodemographic factors, such as older age, lower educational level, common symptoms during pregnancy and the quality of prenatal care are determinants of the impact of pregnancy on quality of life (Menezes, Floriano, & Lopes, 2021; Netto, 2007).
Quality of life studies have become more frequent in recent decades. However, most of those involving pregnant women had small samples; restriction of the pregnancy trimester; gestational risk stratification, or the presence of specific diseases (Abreu et al., 2019; de Castro, Ferreira, Camargos, Leite, & Mattos, 2019; Gariepy et al., 2017; Iwanowicz-Palus, Zarajczyk, Pięta, & Bień, 2019; Pantzartzis et al., 2019; Taşdemir, Balci, & Günay, 2010; Trombetta, Traebert, & Nunes, 2018).
Research with women undergoing prenatal care in the Unified Health System (SUS) is important to analyze the context of life and factors that influence the quality of life during pregnancy, as they help to identify the most vulnerable groups in need of more attention. Thus, the aim of this study was to analyze the quality of life and its association with demographic, socioeconomic, obstetric, and health conditions of pregnant women undergoing prenatal care at the SUS in Colombo, Paraná (PR).
method
Design of the study
A cross-sectional study forming part of the longitudinal research “Study of Life and Health Conditions in Pregnancy and Puerperium,” with women in prenatal care at SUS in the municipality of Colombo (PR). Thus, pregnant women who underwent prenatal care at SUS and were residents of Colombo, Paraná, were considered eligible to participate in this study. The interviews took place between March 2018 and September 2019.
Procedure
Information was collected through interviews with a questionnaire applied to pregnant women. To measure quality of life, the WHOQOL-BREF module was used, validated for its use in Brazil by Fleck in 2000. It is composed by four domains: physical, psychological, social relations, and environment, which were treated as variables of outcome. The WHOQOL-BREF consists of 26 questions and each answer follows a performance on the Likert scale - which varies between 1 and 5, with higher scores indicating better quality of life. The scores of the quality of life domains were transformed into a scale from 0 to 1 for the use of the inflated beta regression, and treated as a continuous variable.
As exposure variables, 1. Demographics were selected: age (up to 19 years old, 20-29 years old, 30 years old or more) and self-declared color/ethnicity (white/yellow, brown/black); 2. Socioeconomic: education (0-7 years, 8-10 years; 11 years or more), per capita family income (R$ 0-475, R$ 476-750, R$ 751-3,000) and paid work (no, yes); 3. Obstetrics: number of pregnancies (1st pregnancy, 2nd pregnancy, 3rd pregnancy, or more), planned pregnancy (no, yes) and pregnancy trimester (0-13 weeks, 14 - 26 weeks, 27 or more weeks); and 4. Health conditions: common symptoms during pregnancy (sickness, vomiting, constipation, reflux, and heartburn) and self-reported morbidity (urinary infection, diabetes, hypertension, anemia, pre-eclampsia, eclampsia, and others) were categorized. The minimum wage in Brazil in the year of collection was R$ 998.00 and the dollar was equivalent to R$ 4.01 reais.
All interviewers involved in fieldwork received standardized theoretical training lasting approximately 90 minutes, including all stages and instruments used in the research. After theoretical training, the interviewers received four-hour supervised field training.
In the descriptive analysis, the following descriptive measures were used: position measures (mean and median), dispersion measures (standard deviation, amplitude), quartiles, and percentages. Collinearity was tested between variables using the variance inflation factor (VIF).
To inspect the association the domains of quality of life (outcomes) and exposure variables, inflated beta regression models belonging to the generalized additive models for location, scale, and shape (GAMLSS) were built. The GAMLSS family represents models with greater flexibility to estimate the asymmetry and kurtosis parameters, thus they do not need the exponential family distributions. For the model, initially, demographic variables were introduced, then socioeconomic, obstetrical, and finally, health conditions. Explanatory variables were included, with a p-value ≤ .20 in the model. Variables with p-value <.05 remained in the final model, which was evaluated using quantile residual graphs, QQ (quantile-quantile) plots, and Akaike Information Criteria (AIC) values. For the analysis and data processing, the free software R for statistical computing was used with the aid of packages: gamlss, tidyr, dplyr, ggplot2.
Ethical considerations
The study was approved by the Human Research Ethics Committee of the Health Sciences Sector of the Federal University of Paraná (UFPR), according to opinion number 2405347 on 11/29/2017.
Results
At the end of the collection, there were 130 refusals to participate in the study (mean age = 26.6; 95% CI = [25.7, 27.5]), for a total of 604 pregnant women interviewed (mean age = 26.0; 95% CI = [25.5, 26.4]). The proportion of responses to the questionnaires was 82.3%.
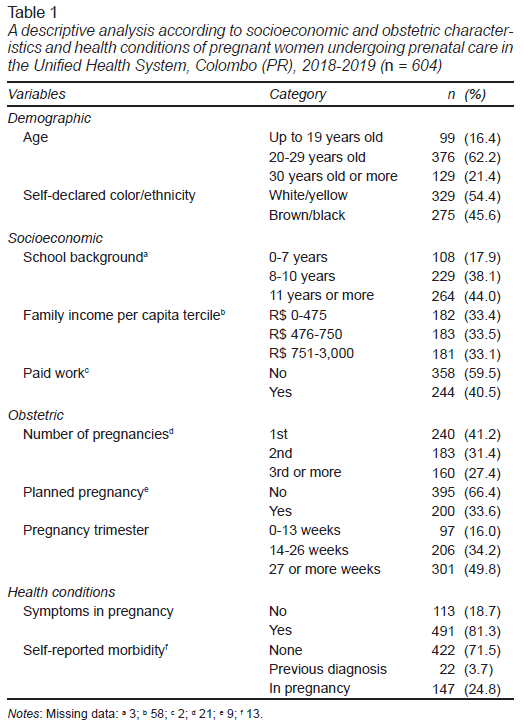
It was found that 62.2% of the pregnant women were aged between 20 and 29 years and had a 33.4% per capita family income between R$ 0 and R$ 475. These women were in their first pregnancy (41.2%), did not plan the pregnancy (66.4%), and did not report any morbidity (71.5%; Table 1).
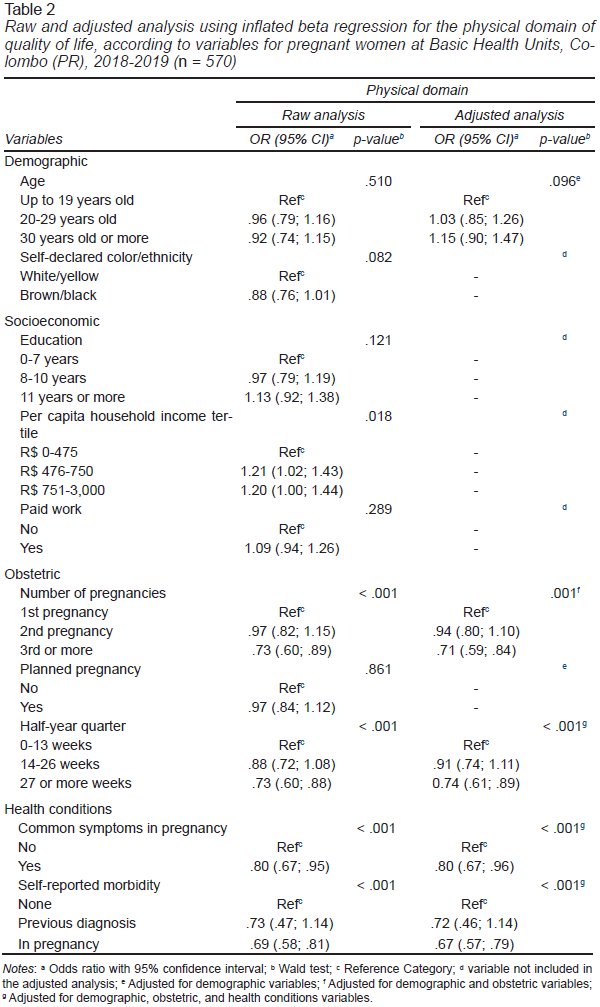
For the adjusted analyses, the sample consisted of 570 responses with complete data. Lower scores for the physical domain of quality of life were associated with higher parity (OR = .71; 95% CI = [.59, .84]), third pregnancy trimester (OR = .74; 95% CI = [.61, .89]), reference to common symptoms (OR = .80; 95% CI = [.67, .95]) and morbidity during pregnancy (OR = .67; 95% CI = [.57, .79]; Table 2).
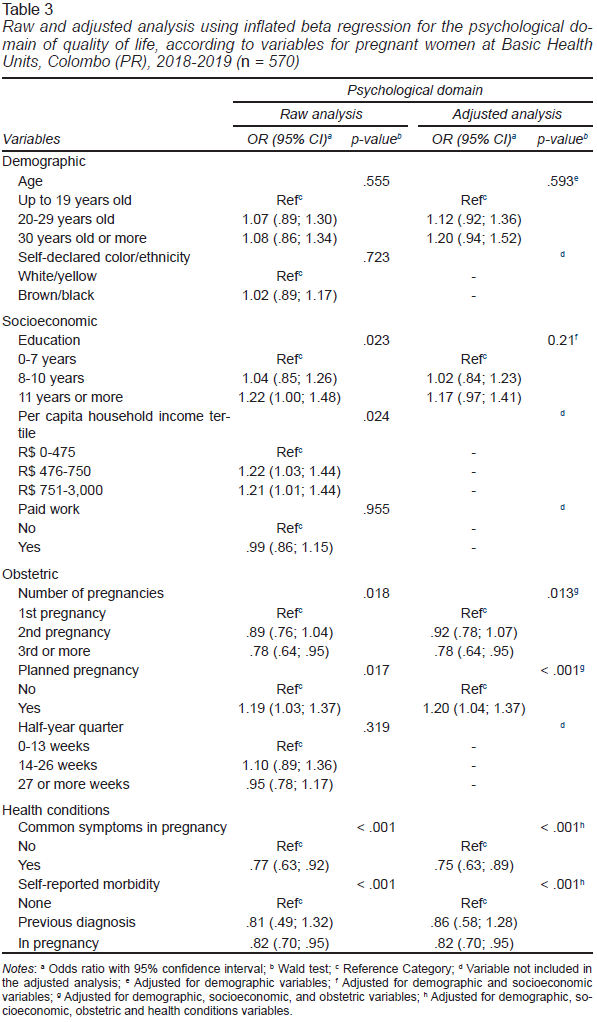
Planned pregnancy (OR = 1.20; 95% CI = [1.04, 1.37]) was associated with higher scores in the psychological domain, while a higher number of common symptoms during pregnancy (OR = .75; 95% CI = [.63, .89]) and having morbidity were associated with lower scores (OR = .82; 95% CI = [.70, .95]). Women with higher education had higher scores (OR = 1.17; 95% CI = [.97, 1.41]), while those with more pregnancies had lower scores (OR = 1.02; 95% CI = [.84, 1.23]; Table 3).
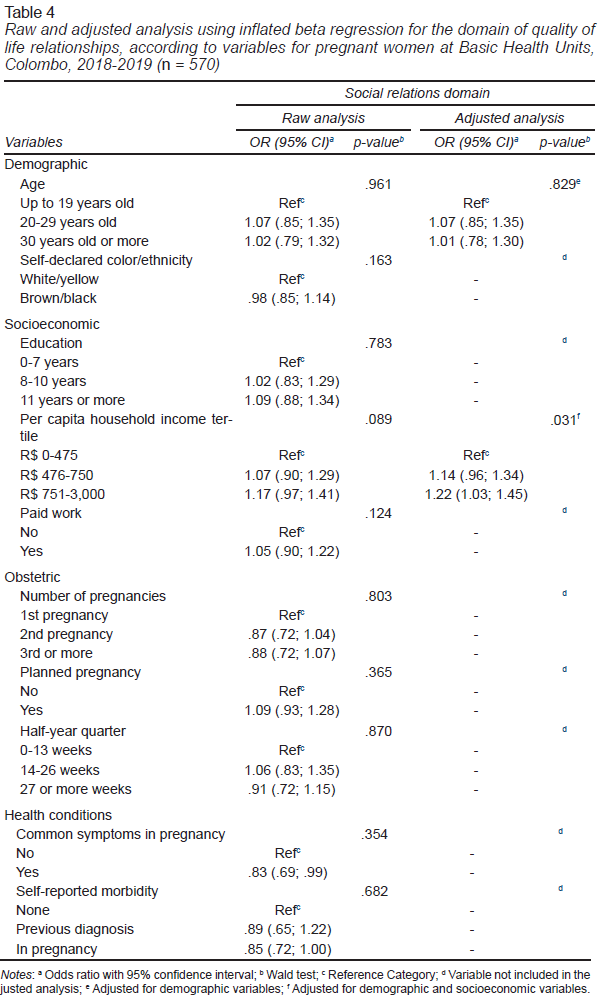
For the social relationship’s domain, higher scores were observed among pregnant women with higher per capita family income (R$751-3,000; OR = 1.22; 95% CI = [1.03, 1.45]; Table 4).
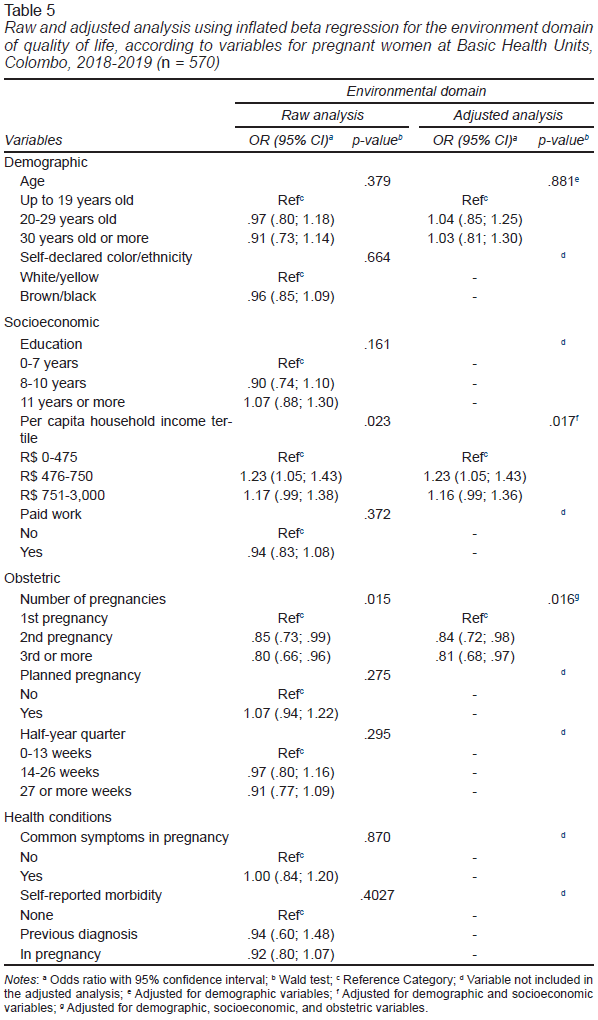
Pregnant women with higher parity (OR = .84; 95% CI = [.72, .98]) had lower scores for the environment domain, while women with income between R$476-750 had higher scores (OR = 1.23; 95% CI = [1.05, 1.43]; Table 5).
It was found that the model’s fit graphs showed random dispersion, independent residuals and normality (data not shown), and AIC values: -288.63; -418.88; 59.44 and -357.31, which had lower AIC values, contributing to a good fit of the model.
Discussion and conclusion
Quality of life was consistently associated with social determinants of health, such as education and income. Pregnant women with low education had lower scores in the psychological domain of quality of life. Similar results were found in studies that used the same instrument, and among pregnant women in basic units in Diamantina (MG), and pregnant women in gynecological clinics in Beirut (Lebanon). Low education can be associated with precarious social relationships, less access to information, lower income and other factors; while higher education is associated with better health perception, easier access to health services, and greater access to information, facilitating self-management of health care (Andrade, 2020; Liu et al., 2016; Mourady et al., 2017).
Dutch and low-income Colombian pregnant women showed lower quality of life scores using the Short Form-36 questionnaire (Bai, Raat, Jaddoe, Mautner, & Korfage, 2018). In general, low-income women have greater difficulties in developing paid activities. Occupational activities in this group are characterized by greater physical strain, with more precarious ties, plus double working hours, with activities related to childcare and home care, which can lead to more restricted personal and social relationships, and consequently less quality of life in the domain of social relationships (de Castro et al., 2019). Higher income was associated with better quality of life scores in the domain of social relationships among pregnant women.
Pregnancy planning was associated with higher quality of life scores in the psychological domain. A possible justification is that planning the pregnancy can reduce the effect of negative aspects arising from the concern with planning changes, spending on children, and pregnancy care (Gariepy et al., 2017). In the other hand, negative effects of unwanted pregnancies can last later life, including poorer mental health outcomes, like depression and, anxiety (Lima et al., 2017).
Indian women with low risk of pregnancy and without pre-existing diseases, and healthy Jordanian women attending government institutions, with higher parity, had lower quality of life scores on the SF-36 instrument and, in this study, the parity was significant for the physical and environment domains (Alzboon & Vural, 2019; Singh, Kaur, & Singh, 2015). Multiparity impacts work and family income and is associated with a greater burden of domestic and personal care, and worse levels of mental health (Chang et al., 2014). In 2019, Brazilian women not employed in the labor market dedicated 18.8 hours to domestic activities, 37% of which were related to caring for other people, and the time spent on these activities increased with the number of children (Brasil, 2018). These factors may be associated with the environment domain, as it is the aspect related with financial resources and leisure activities (WHO, 1998).
The association between the last trimesters of pregnancy and worse quality of life scores in the physical domain is a frequent finding in other studies, such as those among Chinese and Canadian pregnant women with the advancement of pregnancy. Thus, symptoms such as lack of sleep, body aches and malaise are intensified, and are associated with a worse quality of life in the physical domain related to pain, discomfort, malaise, sleep, and rest (Bai et al., 2016; Lau & Yin, 2011).
Among the pregnant women evaluated, health conditions were consistently associated with the physical and psychological domains of quality of life, with worse scores for those who reported common symptoms and morbidities during pregnancy. Symptoms such as nausea and vomiting affect physical and emotional health, and negatively affect family, social, and occupational relationships (Bai et al., 2016). Similar results were found in studies with Czech pregnant women measured using the SF-36, and among Iranian pregnant women from government health centers using semi-structured interviews (Balíková & Bužgová, 2014; Kazemi, Nahidi, & Kariman, 2017).
In turn, morbidities, in addition to affecting the physical dimension of health, can cause concern with the development of the fetus, as they are considered risk factors for complications, and modify the classification of the gestational risk stratification, which demands a greater frequency of exams, consultations, and treatments, impacting the quality of life of pregnant women (Bacelar et al., 2020).
Among the limitations of this study, it is noteworthy that women who did not undergo prenatal care were not included, and few reported undergoing prenatal care in private services concomitantly with SUS care, which may have reduced the socioeconomic heterogeneity of the study. In addition, a specific quality of life instrument for pregnant women was not applied. However, this allows comparing non-pregnant and pregnant women, or the same women before and after pregnancy. Furthermore, the inclusion of pregnancy-related variables, such as trimester, symptoms, and parity, allowed the results to be contextualized based on some of the changes that occur in the pregnancy cycle. The sample may be biased considering refusals. Although we obtained a good response rate, and when comparing age, for example, there were no differences between those who responded and those who refused. Another limitation is that aspects of mental health prior to pregnancy were not asked to women, which may have interfered on the findings of the study.
For the next study, the inclusion of women from private services and the use of a specific quality of life instrument for pregnant women is suggested.
In the present study, part of the longitudinal, it is concluded that quality of life was associated with variables socioeconomics, obstetrics, and health conditions variables. For future studies, it is suggested to evaluate the impact of quality of life on maternal and child outcomes with longitudinal designs and qualitative studies in order to have an in-depth discussion on socioeconomic issues such as income, education, domestic burden, among others.
The results of this study show the need for macro-structural actions that expand the network of support and care for women, such as women’s health care programs, especially for those who have more children, lower economic status, and less education in order to provide conditions for improving their quality of life.