Salud mental 2022;
ISSN: 0185-3325
DOI: 10.17711/SM.0185-3325.2022.040
Received: 2 June 2021
Accepted: 12 November 2021
Fear of cancer recurrence in informal caregivers of childhood cancer survivors
Fatima Sagrario Espinoza-Salgado1 , Edgar Landa-Ramírez2 ,1 , Rebeca Robles3
1 Facultad de Psicología, Universidad Nacional Autónoma de México, Ciudad de México, México.
2 Programa de Psicología Urgencias, Hospital General doctor Manuel Gea González, Ciudad de México, México.
3 Centro de Investigación en Salud Mental Global, Dirección de Investigaciones Epidemiológicas y Psicosociales, Instituto Nacional de Psiquiatría Ramón de la Fuente Muñiz, Ciudad de México, México.
Correspondence: Fatima Sagrario Espinoza Salgado Facultad de Psicología, Universidad Nacional Autónoma de México. Avenida Chapultepec 45 Col. Centro CP 06040 Alcaldía Cuauhtémoc, Ciudad de México México. Phone: +52 55 5709-8112 Email: fatima.espinoza.14@gmail.com
Abstract:
Background. Fear of cancer recurrence is one of the most distressing psychological consequences in cancer survivors and their informal primary caregivers (IPC). IPC of childhood cancer survivors (CCS) are often their mothers, which could intensify fear of cancer recurrence (FCR) and its impact on both IPC and CCS. However, the phenomenon has not been widely described in this specific population.
Objective. To summarize and analyze current evidence on the evaluation and management of FCR among IPC of CCS.
Method. A narrative review of studies included in four databases (PsycInfo, Medline, CINALH, and Web of Science) with no language or year of publication restrictions.
Results. Measures specifically developed to assess FCR among IPC of CCS comprising an interview and a questionnaire with initial psychometric evaluations and two short, online intervention programs based on cognitive-behavioral-contextual therapy were identified (ENGAGE and CASCAdE). Both have demonstrated acceptability in parents of CCS in high-income countries; preliminary evidence also exists of the effectivity of CASCAdE in reducing FCR.
Discussion and conclusion. Given the limitations of this area of psychological evaluation, the Fear of Cancer Recurrence Inventory, originally developed for adult cancer survivors, constitutes the most suitable tool for evaluating FCR among IPC of CCS. The CASCAdE program seems a promising intervention for IPC of CSS, although cultural adaptations, evaluations of its acceptability in low- and middle-income countries, and controlled studies in large samples are still required.
Keywords: Fear of cancer recurrence, caregivers, childhood cancer, survivors..
Resumen:
Antecedentes. El miedo a la recurrencia del cáncer es una de las consecuencias psicológicas más angustiantes en los supervivientes y sus cuidadores primarios informales (CPI). Los CPI de supervivientes de cáncer infantil (SCI) a menudo son sus madres, lo que podría intensificar el miedo a la recurrencia (MR) y su impacto tanto a los CPI como a los SCI. Sin embargo, el fenómeno no se ha descrito ampliamente en esta población específica.
Objetivo. Resumir y analizar la evidencia actual sobre la evaluación y manejo del MR entre CPI de SCI.
Método. Se realizó una revisión narrativa de los estudios incluidos en cuatro bases de datos (PsycInfo, Medline, CINALH y Web of Science) sin restricciones de idioma o año de publicación.
Resultados. Se identificaron instrumentos desarrollados específicamente para evaluar MR entre CPI de SCI que comprenden una entrevista y un cuestionario, además de dos programas de intervención en línea basados en terapia cognitivo-conductual-contextual (ENAGE y CASCAdE). Ambos demostraron aceptabilidad en los padres de SCI en países de ingresos altos. También existe evidencia preliminar de la efectividad de CASCAdE en la disminución del MR.
Discusión y conclusión. Dadas las limitaciones de esta área de evaluación psicológica, el Inventario del Miedo a la Recurrencia del Cáncer, desarrollado originalmente para supervivientes adultos, constituye la herramienta más adecuada para evaluar MR en los CPI de SCI. El programa CASCAdE parece una intervención prometedora para CPI de SCI, aunque aún requiere adaptaciones culturales, evaluaciones de aceptabilidad en países de ingresos medio-bajos y estudios controlados con nuestras más grandes.
Palabras clave: Miedo a la recurrencia del cáncer, cuidadores, cáncer infantil, supervivientes.
Background
Worldwide, between 50 and 200 million children population suffer some form of cancer (neoplasms before the age of 20; Piñeros, Mery, Soerjomataram, Bray, & Steliarova-Foucher, 2021; Steliarova-Foucher et al., 2017). In this age group, leukemias are the most common type of cancer, with 50% of the cases. Though it has been estimated that, with adequate treatment and depending on the type of cancer, stage, and geographic region, between 62-80% of the children with cancer will reach survival (Ferlay et al., 2019; Rebholz et al., 2011; Ward, DeSantis, Robbins, Kohler, & Jemal, 2014), in the case of Mexico these percentages are lower, around 55% (Rivera-Luna et al., 2017; Rodríguez-Romo et al., 2018).
According to some authors, survival is the process that occurs from the point of diagnosis to the remainder of the patient’s life (Marzorati, Riva, & Pravettoni, 2017). For others, a cancer survivor is a person who has completed oncological treatment and become disease-free (Marcus, 2004). In any case, medical follow-up is considered important do to the survivors’ higher risk of developing chronic diseases or dying at younger ages in comparison with the general population (Bhatia, Landier, Casillas, & Zeltzer, 2006; Kurt et al., 2012; Oeffinger et al., 2006; Suh et al., 2020). This survival phenomenon is not exclusive to the patient who has been disease free, but also to those who have accompanied him/her throughout the process, since caregivers ‒generally family members‒ are also considered part of the survival and are impacted by the effects of the disease (National Cancer Institute [NCI], 2020).
An informal primary caregiver (IPC) is a person who shares an affective bond with the patient. In the case of childhood cancer survivors (CCS), between 90% and 95% of IPC are mothers (Holosbach & Solares, 2010). During the illness, the IPC meets patient needs not covered by the formal sector, such as providing emotional support, health care and direct care, despite not having received, any professional training to perform these tasks (Romito, Goldzweig, Cormio, Hagedoorn, & Andersen, 2013) and having limited financial resources (Koyanagi et al., 2018). It is estimated that this care lasts for between one- and three-years during the treatment of the disease and if patient survival is achieved, care may be maintained due to late effects and/or treatment (Oeffinger, Hudson, & Landier, 2009; Rebholz et al., 2011), which add up to the tasks of parenting (Sharkey et al., 2019).
Care provision has an impact at least three levels: 1. financial: treatment is expensive for the average family, meaning that the IPC must obtain resources, bringing about debts and stress (Fitch, Sharp, Hanly, & Longo, 2021; Hanratty, Holland, Jacoby, & Whitehead, 2007); 2. physical: self-care, physical activity, and good eating habits decrease, with health problems frequently being reported (such as sleep disorders, fatigue, headaches, physical exhaustion due to lack of rest; Klassen et al., 2008); and 3. mental: IPC tend to present distress, anxiety, depression, post-traumatic stress, and adverse effects on their quality of life (Kearney, Salley, & Muriel, 2015; Pierce et al., 2017).
Fear of recurrence
One common psychological consequence described in adult survivors and their IPC is fear of cancer recurrence (FCR), defined as “a fear or concern that the cancer will return or progress in the same or another part of the body” (Northouse, 1981, p.1). It is characterized by high levels of worry, rumination, or intrusive thoughts regarding the return of cancer, maladaptive coping, functional impairments, excessive emotional distress, difficulty planning, low adherence to healthy habits, increased medical visits, and the abandonment of medical surveillance (Lebel et al., 2014; Simonelli, Siegel, & Duffy, 2017).
According to the literature, factors related to a greater risk of FCR among IPC include: 1. being a woman (Holosbach & Solares, 2010; Romito et al., 2013), 2. having low educational attainment (Simard et al., 2013), 3. presenting symptoms of anxiety and depression (Abate et al., 2018; Carreño-Moreno, Chaparro-Díaz, & Blanco-Sánchez, 2017; Kalra, Kamath, Trivedi, & Janca, 2008; Montero, Jurado, & Méndez, 2014; Nam et al., 2016; Prussien et al., 2018; Wikman, Mattsson, von Essen, & Hovén, 2018); 4. a decline in the quality of life (Klassen et al., 2008; Mellon, Kershaw, Northouse, & Freeman-Gibb, 2007); 5. being the mother of the patient (Montero, Espinoza, Bravo, & Méndez, 2017); and 6. the duration and type of treatment received by the survivor (McGinty, Goldenberg, & Jacobsen, 2012; Simard et al., 2013). IPC also experience psychosocial sequelae during cancer survival, particularly fear of cancer recurrence, which, in addition to having direct negative consequences for themselves, may impact the quality of care provided to cancer survivors at vital stages of their growth and development (Ernst et al., 2020; Sharkey et al., 2019).
Clearly, FCR reduce ICC’s quality of life and should therefore be considered an important part of their routine clinical care (Butow et al., 2018; Simard et al., 2013). Existing guidelines for FCR in adult survivors mention that effective psychological interventions for this phenomenon include elements of cognitive-behavioral therapy and mindfulness (Butow et al., 2018). However, no specific clinical guidelines for the evaluation and treatment of FCR have been developed specifically for IPC of CCS.
The relevance of this phenomenon contrasts with the scant evidence on the evaluations and interventions reported so far, meaning that systematic efforts to increase studies in the field are warranted. This narrative review therefore seeks to summarize and analyze the studies undertaken to evaluate and manage FCR among IPC of CCS. To guide this review, two questions were designed from the acronym PICO: 1. A PO question to identify psychometric instruments that evaluate FCR in IPC (of both adults and CCS): Do Informal Primary Caregivers of cancer survivors present fear of recurrence? and 2. A PIO question (only for ICP for CCS): In Informal Primary Caregivers of childhood cancer survivors is Psychotherapy, Cognitive Behavioral Therapy significant for Fear of Recurrence?
Method
A systematic search was carried out in May 2020 using four databases: PsycInfo via Ovid, Medline via Ovid, CINALH via EBSCO, and Web of Science via Clarivate. A combination of MeSH and text word terms was used to identify the relevant studies (including caregiver, mothers, parents, cancer survivor, child* cancer, cognitive behav* therapy, psychotherapy, fear, anxiety, fear of cancer recurrence, and cancer recurrence) to identify the studies. The inclusion criteria for this search were: articles with title or abstract referring to caregivers, mothers, or fathers who cared for a childhood cancer survivor, where a cognitive-behavioral intervention program for FCR was evaluated or involved and quantitative results were included.
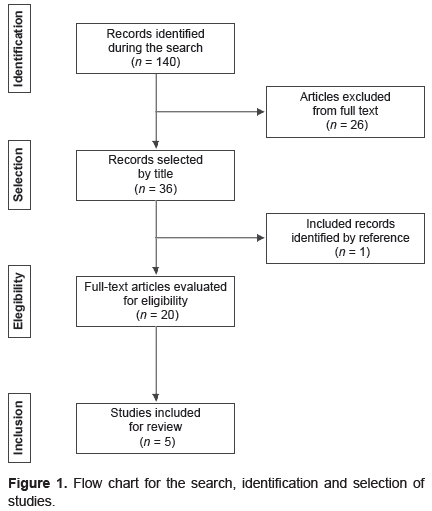
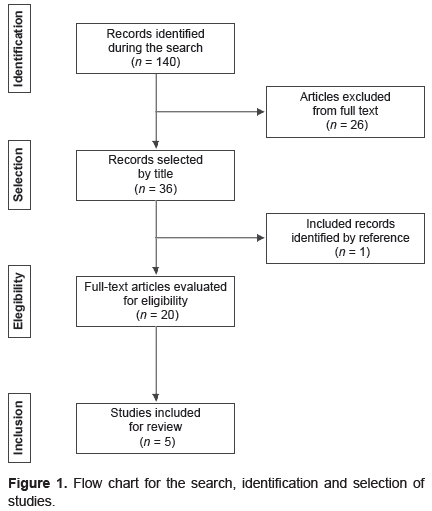
A total of 140 articles were identified, and after a selection process described in Figure 1. The studies that were excluded from this review were mostly studies with cancer survivors (children or adults) not ICP, and two that evaluated treatments for ICP (combinations of cognitive-behavioral treatments with systemic techniques) but in order to reduce symptoms of post-traumatic stress (Kazak et al., 1999; 2004) not FCR. Finally, six articles were selected for the present review. All were in English and met the criteria of having as main objectives of the study the description, evaluation and/or development of a psychometric instrument for FCR, or the description and evaluation of a cognitive-behavioral intervention program.
view
Results
What are the tools described to assess fear of recurrence?
FCR evaluation in IPC of CCS has been undertaken through open and semi-structured clinical interviews. For example, in the descriptive study by Iwai et al. (2017), 57 dyads (parents-survivors) were interviewed through a questionnaire on their demographic characteristics, mental and physical health status (in a four-point Likert scale), and concerns (using open-ended questions). However, this evaluation indiscriminately uses terms such as anxiety, worry, and fear, and lacks specificity and homogeneity in the assessment and explanation of the phenomenon.
Another attempt to evaluate FCR among IPC of CCS was the questionnaire created by Woodford et al. (2018) to determine the usefulness of an intervention program. This questionnaire comprises five questions with Likert-type response options (from five = very frequent, to one = not at all). Although it has the advantage of having been administered in a clinical setting, none of its psychometric properties were reported, which places major constraints on its use in other populations.
The instrument for evaluating FCR among parents of CCS with at least initial proven psychometric properties is the Parents’ Attitudes Toward Childhood Cancer (Duran, 2011). This measure includes 12 items with Likert-type response options (from 1 = strongly disagree, to five = totally agree). It was developed in five stages: content universe, expert judging, development of response options, piloting in the target population with 84 parents of CCS, and construct and content validity. Two factors with moderate inter-correlation (r = .53) emerged: 1. perseverance of parental concerns (α = .91) and 2. psychosocial losses (α = .76). However, no total internal consistency coefficient was reported, and since the sample size is small, its use in other populations is not warranted due to the lack of methodological characteristics suggested by experts in psychometrics (Furr, 2018; Nunally & Bernstein, 1994; Streiner, Norman, & Cairney, 2015).
Given the limitations in this area of psychological evaluation, some authors have decided to use questionnaires developed originally for IPC of adults’ cancer survivors to evaluate IPC of CCS (e.g. Wakefield et al., 2016). The first instrument was the Fear of Recurrence Questionnaire (Northouse, 1981), comprising 22 items with five response options (from five = strongly agree, to one = disagree), originally developed to evaluate the construct among IPC of adult breast cancer survivors. When used with IPC of CCS, only the first five items are administered to assess the presence, frequency, and intensity of FCR. Its development process included the determination of its content validity through expert opinions, its application to IPC of 30 CCS, and the calculation of correlations between the items (close to r = .6, suggesting adequate internal consistency). Additional psychometric evaluations are required for it to be considered a valid, reliable instrument (Furr, 2018; International Test Commission [ITC], 2013; Nunally & Bernstein, 1994; Streiner et al., 2015).
A more useful alternative for evaluating these constructs, also originally developed for IPC of adult cancer survivors: the Fear of Cancer Recurrence Inventory (Simard & Savard, 2009). This is a 42-item questionnaire with five Likert-type response options (from 0 = never/hardly ever, to 5 = all the time/a lot). Total and subtotal scores were obtained. Its creators observed the principles recommended for the construction of psychological measures (DeVellis, 2017; ITC, 2013; Nunally & Bernstein, 1994; Streiner et al., 2015), including focus groups with experts, piloting with cancer survivors, and its administration to 300 cancer survivors for exploratory factor analysis, reliability, and divergent and convergent construct validity. Seven factors and five subscales emerged, with a high internal consistency coefficient (α = .95) indicating that it is a valid, reliable instrument, suitable for survivors of all types of cancer. Its two adaptations to evaluate IPC also demonstrated high internal consistency indexes (α = .94; Lin, Chen, Chang, Fang, & Lai, 2016; Lin, Chen, Simard, Chang, & Lai, 2018).
The FCR began by being described as an emotional state, so instruments to evaluate the construct among ICP, such as the Fear Cancer Recurrence Questioner Family Member (Northouse, 1981), are aimed solely at evaluating the presence of FCR as an emotion. However, after the increase in studies on this phenomenon, its definition and characteristics have been expanded, including related behaviors, trigger situations, beliefs, thoughts, coping strategies, and difficulty in making plans for the future (Fardell et al., 2016; Lebel et al., 2014). All has been reflected in instrument-specific items such as those included in the Fear of Cancer Recurrence Inventory (Simard & Savard, 2009) and the Parents’ Attitudes Toward Childhood Cancer (Duran, 2011), which also include parameters such as frequency, duration, and / or latency of each related behavior.
What are the intervention programs for fear of recurrence in pediatric survivor caregivers?
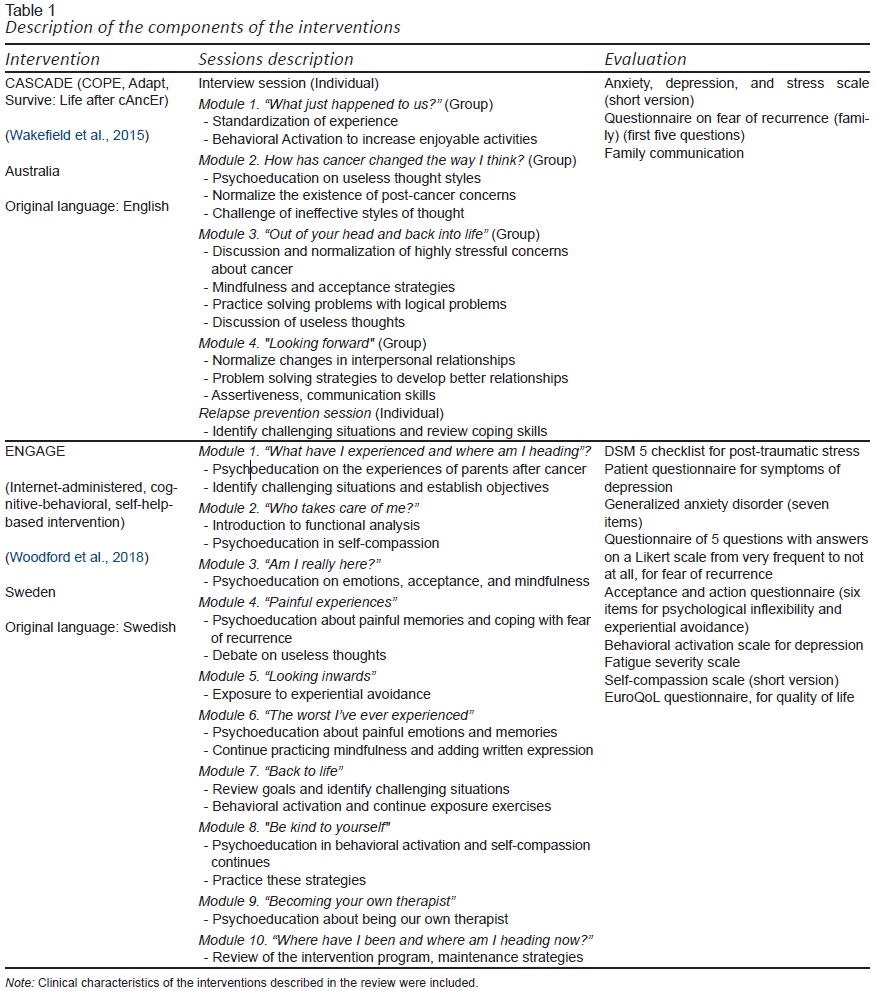
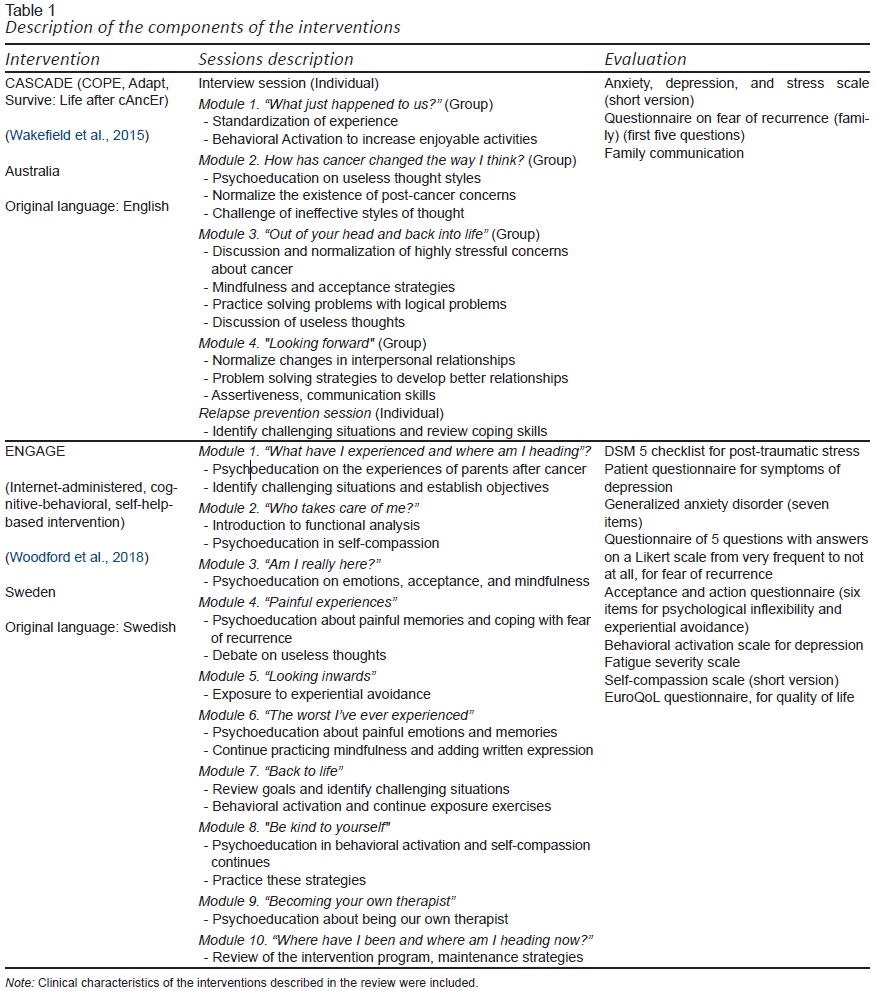
Regarding the interventions for managing FCR in IPC of CCS, two programs were found, both from the cognitive-behavioral-contextual model (Table1), which is in line with the recommendations of the clinical guidelines for FCR in IPC in adult cancer survivors available to date (Butow et al., 2018): CASCAdE (Wakefield et al., 2015), and ENGAGE (Woodford et al., 2018).
view
CASCAdE is an online intervention consisting of six individual and group sessions (Table 1). It was evaluated in a study conducted in Australia by Wakefield et al. (2016) to determine its acceptability and viability, and to generate initial information on its effects on quality of life, depression, anxiety, and FCR. With a control group on the waiting list, 47 parents (intervention group [n = 25], control group [n = 22]) completed self-report instruments based on a randomized, controlled design, including the Fear of Cancer Recurrence Questionnaire (Northouse, 1981), at the beginning, end and at three-month follow-up. Most parents completed the intervention (96%) and evaluations (80%), and a significant effect on fear of recurrence was achieved.
In turns, ENGAGE is an asynchronous (pre-recorded) online intervention comprising 11 individual sessions based on elements of contextual therapies (Table 1). Parents of CSS are encouraged to take one session per week but have 12 weeks to complete the program, which has also been evaluated through an acceptability and viability study in Sweden (Woodford et al., 2018). An uncontrolled intergroup design was used and fifty parents completed self-report instruments on FCR, post-traumatic stress, depression, anxiety, fatigue, and process variables of the acceptance and commitment therapy model (encompassing psychological inflexibility, experiential avoidance, and self-compassion). In this case, FCR was evaluated using a short questionnaire with Likert-type response options (from one = very frequent, to five = hardly at all). Evaluations were carried out prior to the intervention (baseline), weekly, at the end and at a six-week follow-up. Over 70% of parents answered all the evaluations, 50% watched the videos and answered the telephone follow-up, 70% reported having benefited from the intervention, and 95% of the parents completed the whole intervention. Clinical effects on the variables evaluated were not described.
Discussion and conclusion
Although FCR among IPC of CCS is a major importance issue due to its impact on the mental and physical health of both survivors and their caregivers (Cupit-Link, Syrjala, & Hashmi, 2018; Duran, 2011), the number and quality of studies on the evaluation and intervention of this indicate that research efforts in this area are still limited. Key research areas include the development and rigorous psychometric evaluation (DeVellis, 2017; Furr, 2018; ITC, 2013; Nunally & Bernstein, 1994) of the measures specifically designed to assess FCR in IPC of CCS. Nowadays, this construct could be evaluated through proxy instruments, structured interviews, checklists, and distress thermometers (Mitchell, 2007). Therefore, efforts to develop or adapt and evaluate instruments measuring FRC in IPC of CCS in a comprehensive, including its particular affective, behavioral, and cognitive components; (Fardell et al., 2016; Lebel et al., 2014) and culturally relevant way (Reyes-Lagunes & García-Barragán, 2008) are warranted.
Another major research agenda is required for the development and evaluation of intervention programs specifically designed for IPC of CCS. Although valuable recommendations for FCR management exist (Chen et al., 2018; Butow et al., 2018), they have only been evaluated among IPC of adult cancer survivors. The effect of interventions specifically designed for IPC of CCS on FCR has not been directly evaluated but it is assumed to be significant given their impact on related variables (such as anxiety, depression, post-traumatic stress, and quality of life; Simard et al., 2013; Simonelli et al., 2017). FCR has specific characteristics that should be addressed (such as hypervigilance of symptoms, constant rumination about the possibility of cancer recurrence, the fact that there is a real possibility that the cancer will return and that it can produce significant health consequences and avoidant behaviors such as dropping out of medical surveillance; Simard et al., 2013).
The two interventions specifically designed for IPC of CCS are CASCAdE (Wakefield et al., 2015) and ENGAGE (Woodford et al., 2018). Both include intervention strategies based on third-generation cognitive behavioral models, particularly Acceptance and Commitment Therapy (ACT) and mindfulness, for which evidence exists on patients with chronic diseases (Kuba & Weißflog, 2017), and adult cancer survivors (Sharpe et al., 2019). ACT could be used as a transdiagnostic intervention model to promote adaptation to various life challenges through psychological flexibility (rather than engaging in counterproductive attempts to eliminate or repress undesirable experiences; Hayes, Strosahl, & Wilson, 2015). In theory, FCR could be managed from this perspective (Simonelli et al., 2017), as well as among IPC of CCS. However, the current level of evidence is based on feasibility and acceptability studies, and further research of the field is required to corroborate these hypotheses.
Interestingly, both CASCAdE and ENGAGE are online interventions that have demonstrated acceptability (Seitz, Knaevelsrud, Duran, Waadt, & Goldbeck, 2014) and could democratize access to psychological interventions among populations that have reduced their visits to healthcare centers because of their status (as IPC of cancer survivors). This could be particularly important in contexts characterized by scarce mental health human resources and large territories, such as Mexico and other Latin American countries where a significant increase in CCS is anticipated (Shalkow, 2017) and populations are particularly vulnerable to develop psychological problems (Montero, 2013; Koyanagi et al., 2018), including FCR (Simard et al., 2013; Simonelli et al., 2017).
However, online implementation, as suggested by the results of this review, may be a limitation due to the socio-economic characteristics of the region, where not all IPC have access to a device with internet. In the particular case of Mexico, according to the National Institute of Statistics and Geography (Instituto Nacional de Estadística y Geografía [INEGI], 2020), only around half of the households have an internet connection (56.4%). Telephone or face-to-face interventions could be considered so that IPC living in areas distant or close to mental health centers have access to this type of program. Hopefully, initial regional efforts to implement and evaluate psychological treatments for breast cancer survivors (Altuve, 2020) could promote interest, investment, and advances in IPC of CCS psychological treatment, as has been reported in international scientific literature.
As a narrative review, the limitations of this study include the biases imposed by the methodological and clinical training of the authors, which lead to preformed opinions that influence the evaluations and judgments of the studies described (Manterola, Astudillo, Arias, Claros, & Grupo MINCIR, 2013). However, the use of a systematic search in an objective, rigorous, and meticulous way has allowed us to conclude that there is a clear need for further scientific efforts in the field, particularly to ensure the proper identification and management of FCR among IPC of CCS as routine clinical practice.
Funding
None.
Conflict of interest
The authors declare they have no conflicts of interest.
Funding
This study is part of the doctoral research of the first author, with the support of the National Council of Science and Technology (CONACYT) CVU 697167, and under the supervision of the latter.
REFERENCES
Abate, C., Lippé, S., Bertout, L., Drouin, S., Krajinovic, M., Rondeau, É., … Sultan, S. (2018). Could we use parent report as a valid proxy of child report on anxiety, depression, and distress? A systematic investigation of father-mother-child triads in children successfully treated for leukemia. Pediatric Blood & Cancer, 65(2). doi: 10.1002/pbc.26840
Altuve, J. J. (2020). Distrés psicológico, miedo a la recurrencia del cáncer y calidad de vida relacionada con la salud en sobrevivientes de cáncer de mama venezolanas. Psicooncología, 17, 239-253. doi: 10.5209/psic.72019
Bhatia, S., Landier, W., Casillas, J., & Zeltzer, L. (2006). Medical and Psychosocial Issues in Childhood Cancer Survivors. In A. E. Chang, D. F. Hayes, H. I. Pass, R. M. Stone, P. A. Ganz, T. J. Kinsella, J. H. Schiller, & V. J. Strecher (Eds.), Oncology an evidence-based approach (pp. 1801-1813). Nueva York, NY: Springer. doi: 10.1007/0-387-31056-8_102
Butow, P., Sharpe, L., Thewes, B., Turner, J., Gilchrist, J., & Beith, J. (2018). Fear of Cancer Recurrence: A Practical Guide for Clinicians. Oncology (Williston Park, N.Y.), 32(1), 32-38.
Carreño-Moreno, S., Chaparro-Díaz, L., & Blanco-Sánchez, P. (2017) Cuidador familiar del niño con cáncer: Un rol en transición. Revista Latinoaméricana de Bioética, 17(2), 18-30. doi: 10.18359/rlbio.2781
Chen, D., Sun, W., Liu, N., Wang, J., Zhao, J., Zhang, Y., … Zhang, W., (2018). Fear of Cancer Recurrence: A Systematic Review of Randomized, Controlled Trials. Oncology Nursing Forum, 45(6), 703-712. doi: 10.1188/18.ONF.703-712
Cupit-Link, M., Syrjala, K. L., & Hashmi, S. K. (2018). Damocles’ syndrome revisited: Update on the fear of cancer recurrence in the complex world of today’s treatments and survivorship. Hematology/Oncology and Stem Cell Therapy, 11(3), 129-134. doi: 10.1016/j.hemonc.2018.01.005
DeVellis, R. F. (2017). Scale development: Theory and application. California: Sage Publications.
Duran, B. (2011). Developing a Scale to Measure Parental Worry and Their Attitudes Toward Childhood Cancer After Successful Completion of Treatment: A pilot study. Journal of Pediatric Oncology Nursing, 28(3), 154-168. doi: 10.1177/1043454210397755
Ernst, M., Brähler, E., Klein, E. M., Jünger, C., Wild, P. S., Faber, J., … Beutel, M. E. (2020). What’s past is prologue: Recalled parenting styles are associated with childhood cancer survivors’ mental health outcomes more than 25 years after diagnosis. Social Science & Medicine, 252, 112916. doi: 10.1016/j.socscimed.2020.112916
Fardell, J. E., Thewes, B., Turner, J., Gilchrist, J., Sharpe, L., Smith, A., … Butow, P. (2016). Fear of cancer recurrence: a theoretical review and novel cognitive processing formulation. Journal of Cancer Survivorship, 10(4), 663-673. doi: 10.1007/s11764-015-0512-5
Ferlay, J., Colombet, M., Soerjomataram, I., Mathers, C., Parkin, D. M., Piñeros, M., … Bray, F. (2019). Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. International Journal of Cancer, 144(8), 1941-1953. doi: 10.1002/ijc.31937
Fitch, M. I., Sharp, L., Hanly, P., & Longo, C. J. (2021). Experiencing financial toxicity associated with cancer in publicly funded healthcare systems: a systematic review of qualitative studies. Journal of Cancer Survivorship: Research and Practice, 16, 314-328. doi: 10.1007/s11764-021-01025-7
Furr, M. (2018). Psychometrics: An Introduction (3rd Ed.). Los Angeles: Sage.
Hanratty, B., Holland, P., Jacoby, A., & Whitehead, M. (2007). Financial stress and strain associated with terminal cancer--a review of the evidence. Palliative Medicine, 21(7), 595-607. doi: 10.1177/0269216307082476
Hayes, S. C., Strosahl, K., & Wilson, K. G. (2015) Terapia de aceptación y compromiso: proceso práctica del cambio consiente (mindfulness). Bilbao, España: Descleé de Brouwer.
Holosbach, G., & Solares, T. (2010). Experiences of caregiver of children and teenagers with cancer. Serie: Ciencias da Saúde, 11(1), 89-108.
Instituto Nacional de Estadística y Geografía [INEGI]. (2020). INEGI Estadísticas a propósitos del día mundial del internet, datos nacionales. Retrieved from https://www.inegi.org.mx/contenidos/saladeprensa/aproposito/2020/eap_internet20.pdf
International Test Commission [ITC]. (2013). ITC Guidelines on Test Use (ITC-G-TU-20131008). Retrieved from https://www.intestcom.org/files/guideline_test_use.pdf
Iwai, N., Shimada, A., Iwai, A., Yamaguchi, S., Tsukahara, H., & Oda, M. (2017). Childhood cancer survivors: Anxieties felt after treatment and the need for continued support. Pediatrics International: Official Journal of the Japan Pediatric Society, 59(11), 1140-1150. doi: 10.1111/ped.13390
Kalra, H., Kamath, P., Trivedi, J. K., & Janca, A. (2008). Caregiver burden in anxiety disorders. Current Opinion in Psychiatry, 21(1), 70-73. doi: 10.1097/yco.0b013e3282f2dfca
Kazak, A., Alderfer, A., Streisand, R., Simms, S., Rourke, M., Barakat, L., … Cnaan, A. (2004). Treatment of Posttraumatic Stress Symptoms in Adolescent Survivors of Childhood Cancer and Their Families: A Randomized Clinical Trial. Journal of Family Psychology, 18(3), 493-504. doi: 10.1037/0893-3200.18.3.493
Kazak, A., Simms, S., Barakat, L., Hobbie, W., Foley, B., Golomb, V., … Best, M. (1999). Surviving Cancer Competently Intervention Program (SCCIP): A Cognitive-Behavioral and Family Therapy Intervention for Adolescent Survivors of Childhood Cancer and Their Families. Family Process, 38(2), 176-191. doi: 10.1111/j.1545-5300.1999.00176.x
Kearney, J. A., Salley, C. G., & Muriel, A. C. (2015). Standards of Psychosocial Care for Parents of Children with Cancer. Pediatric Blood & Cancer, 62(Suppl 5), S632-683. doi: 10.1002/pbc.25761
Klassen, A. F., Klaassen, R., Dix, D., Pritchard, S., Yanofsky, R., O’Donnell, M., … Sung, L. (2008). Impact of caring for a child with cancer on parents’ health-related quality of life. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology, 26(36), 5884-588. doi: 10.1200/JCO.2007.15.2835
Koyanagi, A., DeVylder, J. E., Stubbs, B., Carvalho, A. F., Veronese, N., Haro, J. M., & Santini, Z. I. (2018). Depression, sleep problems, and perceived stress among informal caregivers in 58 low-, middle-, and high-income countries: A cross-sectional analysis of community-based surveys. Journal of Psychiatric Research, 96, 115-123. doi: 10.1016/j.jpsychires.2017.10.001
Kuba, K., & Weißflog, G. (2017). Acceptanceand Commitment Therapy in the Treatmentof ChronicDisease. Psychotherapie, Psychosomatik,Medizinische Psychologie, 67(12), 525-536. doi: 10.1055/s-0043-118742
Kurt, B. A., Nolan, V. G., Ness, K. K., Neglia, J. P., Tersak, J. M., Hudson, M. M., … Arora, M. (2012). Hospitalization rates among survivors of childhood cancer in the Childhood Cancer Survivor Study cohort. Pediatric Blood & Cancer, 59(1), 126-132. doi: 10.1002/pbc.24017
Lebel, S., Maheu, C., Lefebvre, M., Secord, S., Courbasson, C., Singh, M., … Catton, P. (2014). Addressing fear of cancer recurrence among women with cancer: a feasibility and preliminary outcome study. Journal of Cancer Survivorship: Research and Practice, 8(3), 485-496. doi: 10.1007/s11764-014-0357-3
Lin, C. R., Chen, S. C., Chang, J. T., Fang, Y. Y., & Lai, Y. H. (2016). Fear of cancer recurrence and its impacts on quality of life in family caregivers of patients with head and neck cancers. Journal of Nursing Research, 24(3), 240-248. doi: 10.1097/jnr.0000000000000169
Lin, C. R., Chen, S. C., Simard, S., Chang, J. T., & Lai, Y. H. (2018). Psychometric testing of the Fear of Cancer Recurrence Inventory-caregiver Chinese version in cancer family caregivers in Taiwan. Psycho-Oncology, 27(6), 1580-1588. doi: 10.1002/pon.4697
Manterola, C., Astudillo, P., Arias, E., Claros, N., & Grupo MINCIR. (2013) Revisiones sistemáticas de la literatura. Qué se debe saber acerca de ellas. Cirugía Española, 91(3), 149-155. doi: 10.1016/j.ciresp.2011.07.009
Marcus, A. (March 24, 2004). Debate heats up on defining a cancer survivor. The Wall Street Journal. Retrieved from https://www.wsj.com/articles/SB108008897185563641
Marzorati, C., Riva, S., & Pravettoni, G. (2017). Who Is a Cancer Survivor? A Systematic Review of Published Definitions. Journal of Cancer Education, 32(2), 228-237. doi: 10.1007/s13187-016-0997-2
McGinty, H. L., Goldenberg, J. L., & Jacobsen, P. B. (2012) Relationship of threat appraisal with coping appraisal to fear of cancer recurrence in breast cancer survivors. Psycho-Oncology, 21(2), 203-210. doi: 10.1002/pon.1883
Mellon, S., Kershaw, T. S., Northouse, L. L., & Freeman-Gibb, L. (2007). A family-based model to predict fear of recurrence for cancer survivors and their caregivers. Psycho-Oncology, 16(3), 214-223. doi: 10.1002/pon.1074
Mitchell, A. J. (2007). Pooled results from 38 analyses of the accuracy of distress thermometer and other ultra-short methods of detecting cancer-related mood disorders. Journal of Clinical Oncology, 25(29), 4670-4681. doi: 10.1200/JCO.2006.10.0438
Montero, X. (2013). Valoración integral y factores de cambio en la carga de cuidadores primarios informales de niños con cáncer (Doctoral dissertation). Retrieved from http://www.ciencianueva.unam.mx/xmlui/handle/123456789/83
Montero, X., Espinoza, F., Bravo, M., & Méndez, J. (2017) Ansiedad en Cuidadores primarios informales de niños y adultos con cáncer. In: C. Roja & Y. Gutiérrez (Eds.). Psicooncología 2: Enfoques, Avances e Investigación (pp. 297-318). Chile: Nueva Mirada Ediciones. Retrieved from https://dialnet.unirioja.es/servlet/libro?codigo=851170
Montero, X., Jurado, S., & Méndez, J. (2014). Carga, ansiedad y depresión en cuidadores primarios informales de niños con cáncer. Psicología y Salud, 24(1), 45-53
Nam, G. E., Warner, E. L., Morreall, D. K., Kirchhoff, A. C., Kinney, A. Y., & Fluchel, M. (2016). Understanding psychological distress among pediatric cancer caregivers. Supportive Care in Cancer, 24(7), 3147-3155. doi: 10.1007/s00520-016-3136-z
National Cancer Institute [NCI]. (2020). Cancer Diccionary. Retrieved from https://www.cancer.gov/espanol/publicaciones/diccionario/ampliar/S
Northouse, L. L. (1981). Mastectomy patients and the fear of cancer recurrence. Cancer Nursing, 4(3), 213-220. doi: 10.1097/00002820-198106000-00004
Nunally, J., & Bernstein, I. (1994). Psychometric Theory (3rd Ed.). New York: McGraw-Hill.
Oeffinger, K. C., Hudson, M. M., & Landier, W. (2009). Survivorship: Childhood cancer survivors. Primary Care: Clinics in Office Practice, 36(4), 743-780. doi: 10.1016/j.pop.2009.07.007
Oeffinger, K. C., Mertens, A. C., Sklar, C. A., Kawashima, T., Hudson, M. M., Meadows, A. T., … Childhood CancerSurvivorStudy. (2006). Chronic health conditions in adult survivors of childhood cancer. New England Journal of Medicine, 355(15), 1572-1582. doi: 10.1056/NEJMsa060185
Pierce, L., Hocking, M. C., Schwartz, L. A., Alderfer, M. A., Kazak, A. E., & Barakat, L. P. (2017). Caregiver distress and patient health-related quality of life: Psychosocial screening during pediatric cancer treatment. Psycho-Oncology, 26(10), 1555-1561. doi: 10.1002/pon.4171
Piñeros, M., Mery, L., Soerjomataram, I., Bray, F., & Steliarova-Foucher, E. (2021). Scaling Up the Surveillance of Childhood Cancer: A Global Roadmap. Journal of the National Cancer Institute, 113(1), 9-15. doi: 10.1093/jnci/djaa069
Prussien, K. V., Murphy, L. K., Gerhardt, C. A., Vannatta, K., Bemis, H., Desjardins, L., … Compas, B. E. (2018). Longitudinal associations among maternal depressive symptoms, child emotional caretaking, and anxious/depressed symptoms in pediatric cancer. Journal of Family Psychology, 32(8), 1087-1096. doi: 10.1037/fam0000463
Rebholz, C. E., Reulen, R. C., Toogood, A. A., Frobisher, C., Lancashire, E. R., Winter, D. L., … Hawkins, M. M. (2011). Health care use of long-term survivors of childhood cancer: the British Childhood Cancer Survivor Study. Journal of Clinical Oncology, 29(31), 4181-4188. doi: 10.1200/JCO.2011.36.5619
Reyes-Lagunes, I., & García-Barragán, L. F. (2008). Procedimiento de validación psicométrica culturalmente relevante: Un ejemplo. La Psicología Social en México, 12(1), 625-630.
Rivera-Luna, R., Zapata-Tarres, M., Shalkow-Klincovstein, J., Velasco-Hidalgo, L., Olaya-Vargas, A., Finkelstein-Mizrahi, N., … Aguilar-Ortiz, M. R. (2017). The burden of childhood cancer in Mexico: Implications for low- and middle-income countries. Pediatric Blood & Cancer, 64(6), e26366. doi: 10.1002/pbc.26366
Rodríguez-Romo, L., Olaya Vargas, A., Gupta, S., Shalkow-Klincovstein, J., Vega-Vega, L., Reyes-Lopez., … Booth, C. M., (2018). Delivery of Pediatric Cancer Care in Mexico: A National Survey. Journal of Global Oncology, 4, 1-12. doi: 10.1200/JGO.17.00238
Romito, F., Goldzweig, G., Cormio, C., Hagedoorn, M., & Andersen B. (2013). Informal Caregiving for cancer patients. Cancer, 119(Suppl 11), 2160-2169. doi: 10.1002/cncr.28057
Seitz, D. C., Knaevelsrud, C., Duran, G., Waadt, S., & Goldbeck, L. (2014). Internet-based psychotherapy in young adult survivors of pediatric cancer: feasibility and participants’ satisfaction. Cyberpsychology, Behavior and Social Networking, 17(9), 624-629. doi: 10.1089/cyber.2014.0066
Shalkow, J. (2017). Cáncer en México, Situación Actual y Retos, (58). Retrieved from: https://www.paho.org/sites/default/files/Cancer-infantil-en-MEXICO.pdf
Sharkey, C. M., Clawson, A. H., Mullins, L. L., Brinkman, T. M., Pui, C. H., Hudson, M. M., & Krull, K. R. (2019). The relationship of child executive functions to parenting capacities in childhood acute lymphoblastic leukemia survivors. Pediatric Blood & Cancer, 66(8), e27761. doi: 10.1002/pbc.27761
Sharpe, L., Turner, J., Fardell, J. E., Thewes, B., Smith, A. B., Gilchrist, J., … Butow, P. (2019). Psychological intervention (ConquerFear) for treating fear of cancer recurrence: mediators and moderators of treatment efficacy. Journal of Cancer Survivorship, 13(5), 695-702. doi: 10.1007/s11764-019-00788-4
Simard, S., & Savard, J. (2009) Fear of Cancer Recurrence Inventory: development and initial validation of a multidimensional measure of fear of cancer recurrence. Supportive Care Cancer, 17(3), 241‐251. doi: 10.1007/s00520-008-0444-y
Simard, S., Thewes, B., Humphris, G., Dixon, M., Hayden, C., Mireskandari, S., & Ozakinci, G. (2013). Fear of cancer recurrence in adult cancer survivors: A systematic review of quantitative studies. Journal of Cancer Survivorship, 7(3), 300-322. doi: 10.1007/s11764-013-0272-z
Simonelli, L. E., Siegel, S. D., & Duffy, N. M. (2017). Fear of cancer recurrence: a theoretical review and its relevance for clinical presentation and management. Psycho-Oncology, 26(10), 1444-1454. doi: 10.1002/pon.4168
Steliarova-Foucher, E., Colombet, M., Ries, L., Moreno, F., Dolya, A., Bray, F., … IICC-3 Contributors. (2017). International incidence of childhood cancer, 2001-10: a population-based registry study. The Lancet Oncology, 18(6), 719-731. doi: 10.1016/S1470-2045(17)30186-9
Streiner, D. L., Norman, G. R., & Cairney, J. (2015). Health measurement scales: A practical guide to their development and use (5th Ed). New York, NY: Oxford University Press.
Suh, E., Stratton, K. L., Leisenring, W. M., Nathan, P. C., Ford, J. S., Freyer, D. R., …Henderson, T. O. (2020). Late mortality and chronic health conditions in long-term survivors of early-adolescent and young adult cancers: A retrospective cohort analysis from the Childhood Cancer Survivor Study. The Lancet Oncology, 21(3), 421-435. doi: 10.1016/S1470-2045(19)30800-9
Wakefield, C. E., Sansom-Daly, U. M., McGill, B. C., McCarthy, M., Girgis, A., Grootenhuis, M., … Cohn, R. J. (2015). Online parent-targeted cognitive-behavioural therapy intervention to improve quality of life in families of young cancer survivors: study protocol for a randomized controlled trial. Trials, 16, 153. doi: 10.1186/s13063-015-0681-6
Wakefield, C., Sansom-Daly, U., McGill, B., Ellis, S., Doolan, E., Roberson, E., … Cohn, R. (2016). Acceptability and feasibility of an e-mental health intervention for parents of childhood cancer survivors: Cascade. Supportive Care Cancer, 24(6), 2685-2694. doi: 10.1007/s00520-016-3077-6
Ward, E., DeSantis, C., Robbins, A., Kohler, B., & Jemal, A. (2014). Childhood and adolescent cancer statistics, 2014. CA: A Cancer Journal for Clinicians, 64(2), 83-103. doi: 10.3322/caac.21219
Wikman, A., Mattsson, E., von Essen, L., & Hovén, E. (2018). Prevalence and predictors of symptoms of anxiety and depression, and comorbid symptoms of distress in parents of childhood cancer survivors and bereaved parents five years after end of treatment or a child’s death. Acta Oncologica (Stockholm, Sweden), 57(7), 950-957. doi: 10.1080/0284186X.2018.1445286
Woodford, J., Wikman, A., Cernvall, M., Ljungman, G., Romppala, A., Grönqvist, H., & von Essen, L. (2018). Study protocol for a feasibility study of an internet-administered, guided, CBT-based, self-help intervention (ENGAGE) for parents of children previously treated for cancer. BMJ Open, 8(6), e023708. doi: 10.1136/bmjopen-2018-023708