INTRODUCTION
The pandemic caused by SARS-CoV2, the etiologic agent of COVID-19, represents an unprecedented social on April 2022, there have been 5, 950, 424 accumulated cases and 337, 435 deaths related to COVID-19 since the pandemic began. Lockdown started on March 23rd, 2020, and it extended over a year, with a peak (average number of infections per day) on January 20th, 2021 (Secretaría de Salud, 2020).
Since older adults (OA) were particularly susceptible to develop severe manifestations of the disease and complications that increase disability and decrease quality of life (Sepulveda-Loyola et al., 2020), it was a priority that this population sector remains isolated as an effective prevention strategy; however, this represented a new challenge for older adults’ mental health. At this point, two different terms must be introduced: a) Social isolation, which is defined as having low quality of contact with others; it is objective and can be measured using observations of an individual’s social network (Freedman & Nicolle, 2020) , b) Loneliness, which refers to the adverse emotional state experienced subjectively related to the perception of unsatisfied intimate and social needs (Luanaigh & Lawlor, 2008).
Prevalence suggests that nearly one-third of older adults experience loneliness and/or social isolation, and a subset (5%) reports often or always feeling lonely (Kotwal et al., 2021). Although loneliness does not have the status of a clinical disease by itself, it is associated with several negative health outcomes like stress, sleep disturbances, depressive symptoms, cognitive impairment, coronary heart disease, stroke, and mortality (Akhter-Khan et al., 2021).
On the other hand, partial or total restriction of social interaction could generate negative consequences for the health of OA, especially in those with chronic diseases, disabilities, and geriatric syndromes (Sepulveda-Loyola et al., 2020).
Social isolation may cause impairment in social recognition memory, thereby potentially increasing risk of long-term perceptions of loneliness (i.e., animals exposed to social isolation later have difficulties with social recognition; Mumtaz, Khan, Zubair, & Dehpour, 2018). However, it does not affect other types of memory. This may be related to the specific neural network which processes social information in the mammalian brain which includes: olfactory bulbs, medial nucleus of the amygdala, lateral septum, and the pyramidal layer of neurons of the hippocampus which makes a trajectory in the shape of an inverted C, specially in the region called CA2 (Leser & Wagner, 2015).
We aim to examine the influence of loneliness and social isolation in daily cognitive function in a sample of Mexican older adults living in the community during the first wave of COVID-19 pandemic lockdown and assess characteristics associated with loneliness.
METHOD
Design of the study
Cross-sectional study derived from the cohort “The impact of COVID 19 on well-being, cognition, and discrimination among older adults in the United States and Latin America.” carried out in a population of non-institutionalized people aged 55 or older. A non-probabilistic sampling was performed, selecting, for convenience, those in the United States, as well as several in Spanish and Portuguese-speaking countries of Latin America. A detail description of the methodology is summarized in the study by Babulal (2021).
Participants
For this study, we included participants who resided in Mexico (n = 308), during the first six months of lockdown (March–August, 2020). Those who completed the previously described surveys in the first stage or baseline of the SARS-CoV2 pandemic were chosen. All participants completed a one hour-long survey (online with a computer or smartphone or through a phone call with a trained researcher, for help) which was conducted in Spanish. Collected data were managed using the REDCap (Research Electronic Data Capture) tool, a software designed for the research data capture which is located at the Massachusetts General Hospital (Harris et al., 2009). All measurements were translated to Spanish following the World Health Organization guidelines to ensure accuracy.
Dependent variable
Systematic assessment of daily cognitive function offers the potential to improve our understanding of the determinants of functional decline, specific cognitive impairments (Tomaszewski Farias et al., 2011), mild changes in daily function and daily cognition frequently occur in the early stages of neurodegenerative diseases, including during the stage of mild cognitive impairment (MCI; Hsu et al., 2017). Thus we assessed them with the Everyday Cognition Scale (E-Cog). This validated instrument in spanish, has been designed to subjectively assess cognitive and functional abilities, an improvement if compared to its performance 10 years ago. It exhibits excellent psychometric properties including good test–retest reliability (r = .82, p = < .001). It also provides evidence of various aspects of validity such as content and construction as well as convergent, divergent, and external validity. E-Cog comprises 39 items through which six cognitive domains are evaluated, and they are: memory, language, visuospatial, and perceptual abilities and executive functioning (subdivided into planning, organization, and divided attention). Each item is rated using a four-point Likert scale that ranges from 1: better or no change, to 4: consistently much worse (Table 1 in the supplement; Farias et al., 2008). Each functional domain was defined by the underlying cognitive abilities thought to be the most critical to those daily living activities, higher score indicates greater deterioration (Russo et al., 2018).
This scale can be applied directly to the patient (E-Cog) or to their informant (iE-Cog); There are two ways to report the result: a) continuous score: sum between 1 and 4, the total score is divided by the total number of questions answered, thus creating an average score, taking into account the missing data; b) dichotomized score: the suggested cut-off point based on a cross-sectional comparison of the ADNI to discriminate between normal cognition and cognitive impairment is 1.31 for the participant and 1.36 when applied to the informant, which is obtained from the average (continuous score) divided among six total domains evaluated, obtaining a mean of the total average of the scale (van Harten et al., 2018).
Independent variable
Loneliness: The De Jong Gierveld Loneliness Scale (De Jong Gierveld & Tilburg, 2006), measures emotional (items 1, 5 and 6) and social loneliness (items 2, 3 and 4) by three items each, with a total of six items for general loneliness. Participants select an answer from four options which are: “yes”, “more or less”, “no” or “no answer”. Negatively worded items were inverted; afterward these item scores were added to obtain a total for each participant. Higher scores indicate greater loneliness.
Social isolation: The Epidemic-Pandemic Impacts Inventory (EPII; Grasso, Briggs-Gowan, Ford, & Carter, 2020), is a questionnaire developed and designed to assess the personal impact of the coronavirus pandemic in various domains of personal and family life. The EPII consists of 92 items in 10 categories that assess employment (11 items), education (2 items), home life (13 items), social activities (10 items), economy (5 items), emotional health and well-being (8 items), physical health (8 items), physical distancing and quarantine (8 items), history of infection (8 items), and positive change (19 items). For the present study, the subscale of physical distancing and quarantine was used. The responses were summed (yes versus no), and the mean of this subscale was calculated. A higher number in the score suggests a higher load/difficulty.
Subjective Memory Complain: The 7-Memory questionnaire has been validated to assess cognitive changes in older people (Filshtein et al., 2020; Go et al., 1997), and the answers consist of “yes” or “no” according to the subjective memory complaint. The responses were summed to obtain a maximum score of 7. Higher scores represent a greater subjective memory complaint.
Sociodemographic and clinical variables
Information on age, gender, marital status, educational level by years of education, occupation, self-perception of health status, self-reported comorbidities, and the use of medications were included.
Statistical analysis
Descriptive statistics using arithmetic means, standard deviations, frequencies, and proportions examined in sociodemographic and health variables was performed, categorical variables were compared using χ2 and T test in the case of continuous variables. The presence of loneliness, social isolation, and subjective memory complaint (SMC) were binomial variables. Rho Spearman correlations were examined to establish the relationship between the E-Cog total score as well as the outcome measures. In order to determine the association between loneliness, social isolation, and SMC with E-Cog, participants were categorized with using the cut-off point suggested by van Harten et al. (2018) those with a score < 1.31 indicating normal cognition, final average score was obtained from the sum of the means of each domain divided by six. Univariate linear regression models were later adjusted for potentially confounding variables (age, sex, and education) on multivariate linear regression. A value of p < .05 was considered statistically significant. All statistical analyses were conducted using SPSS version 25.0 for MAC (Chicago, IL, USA), figures were made with RStudio (R version 4.1.0, RStudio, Inc., Boston, MA).
Ethical considerations
All participants gave their consent online to be included. This study was approved by the Institutional Ethics Research Committee of the National Institute of Medical Sciences and Nutrition Salvador Zubirán (Instituto Nacional de Ciencias Médicas y Nutrición Salvador Zubirán, INCMNSZ) with the registration ID: GER-3410-20-21-1.
RESULTS
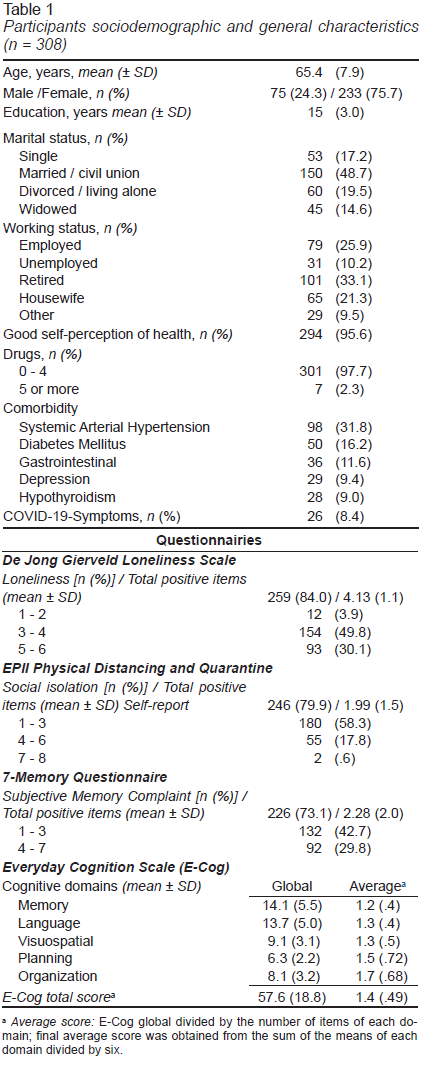
From a total of 308 participants, three participants were excluded for incomplete surveys. Finally, 305 participants were included for statistical analysis from which 75.7% were women (n = 233) with a mean age of 65.4 years (SD = ± 7.9), only 8.4% reported COVID-19 symptoms. Most subjects were married/civil union (48.7%). Those who lived alone were distributed within the following groups: single (17.2%), widowed (14.6%), and divorced/living alone (19% / 48%). The average years of education was 15 (SD = ± 3.0). In terms of occupation, most participants were retired (33.1%), followed by economically active people (25.9%) and housewives (21.3%) (Table 1).
Up to 84.0% (n = 259) had loneliness with a mean affirmative item in the De Jong Gierveld Loneliness scale of 4.13 (SD = ± 1.1) while 79.9% (n = 246) of the participants identified themselves with social isolation using the EPII scale (Table 1). On the other hand, the E-Cog total score was 57.6 (SD = ± 18.8) and average score 1.4 (SD = ± 0.49) with the following highest scores for these cognitive domains: memory (14.1, SD = ± 5.5), language (13.7, SD = ± 5.0), and visuospatial (9.1, SD = ± 3.1).
While 73.1% of the participants reported memory complaint, evidenced with affirmative items in the 7-Memory Questionnaire, the mean affirmative items were 2.2 (SD = ± 2.0), and the major complaints were: in difficulty of remembering things from one second to the next (48.9%) and remembering a short list of items (43.3%).
Loneliness scale (rho .219, p = < .005), EPII Physical Distancing and Quarantine (rho .178, p = < .05) and SMC (rho .68 p = < .001) showed positive Spearman correlation.
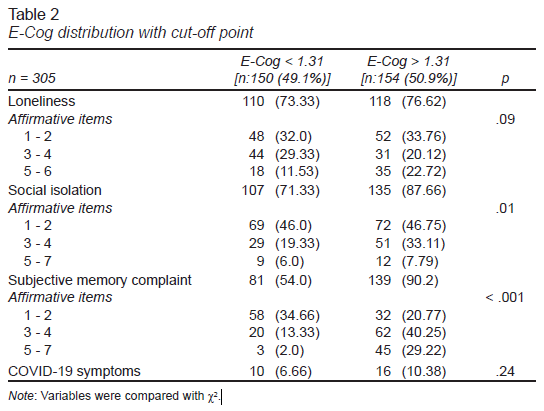
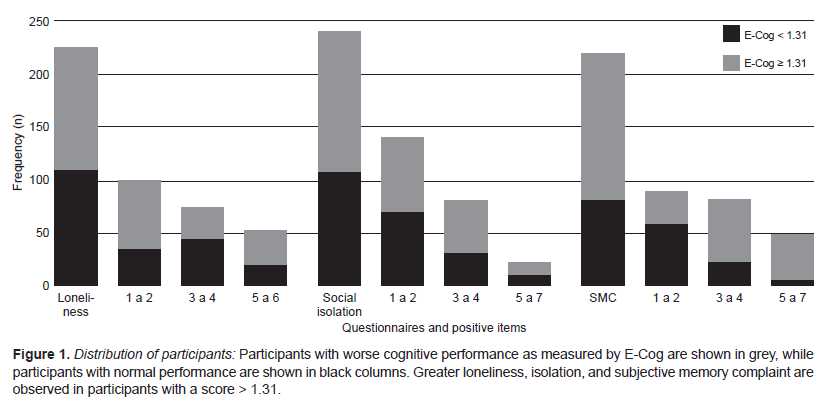
Using the cut-off point suggested by van Hartel et al. (2018), 49.1% (n = 150) had a score < 1.31 indicating normal cognition, while 50.9% (n = 154) had a higher score, corresponding to cognitive impairment (van Harten et al., 2018). The perception of loneliness was higher in the second group (76.62% vs. 73.3%), as well as social isolation (87.66% vs. 71.33%) and SMC (54% vs. 90.2%) demographic characteristics were similar in both groups (Table 2, Figure 1).
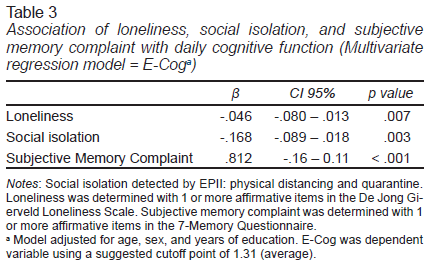
Table 3 describes the multivariate regression model adjusted by age, sex, and education. There’s a negative and statistically significant association with loneliness (β = -.046; 95% CI = [-.080, -.013]; p = .007) and isolation (β = -.168; 95% CI = [-.089, -.018]; p = .003), while SMC had a positive association with ECog (β = .812; 95% CI = [-.16, -.11]; p = < .001), this model explains the 15% of the variability of the E-Cog score.
DISCUSSION AND CONCLUSION
In this study, with data from a remote survey conducted in older adults living in the community, carried out during the first wave of the COVID-19 pandemic in Mexico, we found a negative and statistically significant association with self-perception of loneliness and social isolation and daily cognitive function, in contrast, SMC was higher in those with worse daily cognitive performance.
The frequency of loneliness in the participants is higher than that reported in the literature, being 84% compared to 30.9% and 43.1% reported by a cohort of older adults in California and Canada, respectively, during the COVID-19 pandemic (Savage et al., 2021). This feeling of loneliness appears to be even greater compared to the increase reported during confinement, for instance, in a cohort study of older adults in primary care in Hong Kong (n = 538, age = 70.6 + 6.1). Loneliness measured by the De Jong Gierveld scale during the COVID-19 pandemic increased from 1.6 to 2.9 positive items on average while the participants in our study had an average of 4.13 (1.1) positive items (Wong et al., 2020). Consistent with previous studies (Zovetti, Rossetti, Perlini, Brambilla, & Bellani, 2021), most of the participants with loneliness were women.
Older adults with the lowest report of loneliness were found in the lowest E-Cog scores, that is, those who referred loneliness during lockdown had a worse performance in the global E-Cog score. These findings coincide with those reported by Kim, Beam, Greenberg, and Burke (2020) who points out that loneliness predicts worse performance in several cognitive domains such as immediate memory, visuospatial skills, and processing speed (Kim et al., 2020).
In two previous studies, carried out as cohorts from China and Argentina using the E-Cog scale, the additional memory domains, such as language, divided attention, and planning (Marshall et al., 2014) were associated with a lesser impact on functionality compared to FAQ (Functional Assessment Questionary) without showing an association with hippocampal hypometabolism, and the ROI (Regions of Interest) of Alzheimer’s disease compared to the memory-related domain (Hsu et al., 2017) which could suggest greater usefulness for the detection of amnestic cognitive profiles compared to other scales.
The mechanism that explains how loneliness impacts on cognitive functions remarks a strong relationship with chronic stress underlying prolonged periods of loneliness, increased glucocorticoid activation and hypercortisolism. These physiological alterations occur differently depending on the loneliness’ period length. Thus, transient loneliness can activate the hypothalamic-pituitary-adrenal (HPA) axis to negatively regulate inflammatory responses while persistent loneliness is associated with increased production of pro-inflammatory cytokines such as: tumor necrosis factor-alpha (TNF-α), Interleukin 1-beta (IL-1β), Interleukin 6 (IL-6), among others (COX-2 and iNOS; Akhter-Khan et al., 2021; Bzdok & Dunbar, 2020). This state of chronic inflammation decreases dopamine signaling, circadian rhythm, and monoamine levels (serotonin, norepinephrine, and dopamine) which in turn synaptic plasticity and neuronal survival decrease. Consequently, neurodegeneration increases, perpetuating axis dysfunction HPA and physiological reward mechanisms (Wilkialis et al., 2021). In cohort studies, loneliness was associated with poorer performance in different types of memory, with a faster decline in semantic memory compared to episodic memory (Shankar, Hamer, McMunn, & Steptoe, 2013).
Similar with the English Longitudinal Study of Aging, were social isolation is associated with decreased episodic memory and verbal fluency after a 4-year follow-up period (Shankar et al., 2013) a Spanish study in older adults showed that greater social isolation is associated with lower scores in neuropsychological assessment batteries, reflected in both the global cognitive score and worse performance in verbal fluency and forward digits (Lara et al., 2019). In animal models, these findings have been related to alterations in the CA2 region of the hippocampus, (Leser & Wagner, 2015; Mumtaz et al., 2018) therefore, it is plausible to detect social isolation as an additional risk factor for cognitive impairment. In general, social interaction generates demands that protect and maintain cognition, leaving isolated people vulnerable to impaired cognition (Burns et al., 2020; Kim et al., 2020). Thus, we propose that social isolation in the participants of our study comes from an emergent situation as part of the preventive measures of contagion.
Previous studies with older adults during confinement as a result of COVID-19 in China report that being a woman and living alone carries a greater risk of perceived isolation since they depend more on family members and friends for social support. This was reduced due to social distancing during COVID-19 (Brailean, Steptoe, Batty, Zaninotto, & Llewellyn, 2019). However, this condition of physical distancing does not imply the deprivation of the feeling of accompaniment, protection or closeness to people in the form of an emotional connection as it occurs when experiencing loneliness. That is, the significant effects of loneliness, conceptualized as (self-perceived) social isolation, on general cognitive function can be found together but not always (Burns et al., 2020; Kim et al., 2020).
Regarding SMC, it is known that up to 25 to 50% of older adults living in the community refer it to first-contact doctors, which makes this a common problem. Memory complaint is associated with poorer performance in all the cognitive domains identified with validated instruments, mainly in relation to immediate recall, verbal fluency, and processing speed. These results have been described not only in older adults with increased memory complaints (cognitively intact), but also in those with cognitive impairment (Brailean et al., 2019). We found a higher frequency of SMC than that reported, interestingly, we observed that most of the participants with worse performance in daily cognition had higher SMC, despite having similar sociodemographic characteristics, it stands out that the greatest complaint is found in the items related in memory domain. E-Cog has been proposed as an instrument to assess subjective cognitive decline (SCD): Any occasion SCD = any item scored ≥ 2, but none ≥ 3; any consistent SCD = any item scored ≥ 3. (Rueda et al., 2015) That is, the prognostic value of SCD for incident MCI improves when both consistency of SCD and associated concern are evaluated.(van Harten et al., 2018) Thus, it is important to highlight the role of loneliness and isolation in SMC.
Limitations and strengths
Our study has some limitations, the design of the study, derived from an online survey. We do not have information prior to COVID-19 pandemic lockdown in these older adults, so we cannot know if they had isolation before the starting point of the study. We recognize that the E-Cog results were not compared with informant scores since there are previous studies where people with mild cognitive impairment reported performing better (lower scores) compared to the informants’ report (family members, caregivers; Marshall et al., 2014). On the other hand, although E-Cog has shown good test-retest reliability, even in the Spanish version, where both global and domain-specific scores have shown different trajectories in participants with cognitive impairment, dementia, and cognitive health (Farias et al., 2008; Filshtein et al., 2020; Marshall et al., 2014) so, based on suggested cut-off point derivated from cross-sectional studies (van Harten et al., 2018), this sample had similar characteristics in unimpaired cognition and probably cognitive impaired. Although the history of depression was questioned, we do not have screening tests to rule out the presence of loneliness as a confounding factor for affective disorders (Domènech-Abella et al., 2020; Tragantzopoulou & Giannouli, 2021).
Among the strengths of the study, we were able to describe the health characteristics of a sample of Mexican older adults from the community during the first wave of the SARS-CoV2 pandemic. As far as we know, this is the first study conducted on Mexican older adults with daily cognitive function. Although loneliness and social isolation are usually empirically associated, they should be approached as distinct and independent phenomena.
In our study, we found that OA with loneliness and social isolation have impairment in daily cognitive function which strongly suggests the need to increase vigilance of those identified with these conditions resulting from the deleterious effect on cognition.
The SARS-CoV2 pandemic brought multiple challenges but also valuable lessons for clinicians. Regarding cognition, it was possible to recognize latent but forgotten risk factors: loneliness and social isolation. A frequent condition in older adults prior to the contingency, and that provides greater vulnerability, especially in those who already had cognitive impairment even in preclinical phases like SMC. A better understanding of this phenomenon will allow the development and adaptation of evidence-based interventions to address and prevent its impact on cognitive decline.