INTRODUCTION
The term stigma refers to a sign, mark, or signal that usually has negative connotations and could cause discrimination (Corrigan, Rüsch, & Scior, 2018; Rüsch & Kösters, 2021; Seeman, Tang, Brown, & Ing, 2016; Thornicroft et al., 2016; Wang, Link, Corrigan, Davidson, & Flanagan, 2018). Stigma in mental illness can be defined as a negative attitude caused by the manifestation of a mental disorder or the mention of some psychiatric treatment in a person’s life (Sartorius et al., 2010).
The stigmatization of mental illness affects the relationship with other people and the self-concept of the person who suffers it (Lasalvia et al., 2021; Sartorius et al., 2010; Thornicroft et al., 2016). Such a situation would also affect the quality of care received by those with mental health diagnoses when they develop a non-psychiatric medical condition and are cared for by other specialists (Corrigan et al., 2018; Sartorius et al., 2010; Thornicroft et al., 2016), which results in a deterioration in their quality of life (Sartorius et al., 2010; Wang et al., 2018). Possible causes of persistance of stigma to persist include lack of information and lack of contact or relationship with a person with a mental disorder (Korszun, Dinos, Ahmed, & Bhui, 2012; Pandian et al., 2020; Simon & Verdoux, 2018).
It is worrying that negative and stigmatizing beliefs towards people with a mental disorder affect the general population (WHO, 2018; Lasalvia et al., 2021; Roberts & Bandstra, 2012; Seeman et al., 2016), yet the fact that these ideas extend to doctors-in-training is even more alarming. Medical students may have similar or even more negative attitudes and beliefs (Kassam, Papish, Modgill, & Patten, 2012); cultural stigmatization should not permeate or amplify in medical school (Adams, Lee, Pritchard, & White, 2010).
Stigmatization can be directed towards oneself or someone else (Eksteen, Becker, & Lippi, 2017), and would affect how students learn to provide care since they could prejudge those who seek medical attention (Roberts & Bandstra, 2012). As an additional result, patients could fell unheard and thus avoid speaking about their symptoms and health problems, further affecting the medical care they receive (Leung, Awani, Chima, & Udo, 2015; Rüsch & Kösters, 2021).
The people in charge of education play a fundamental role in facilitating and supervising direct contact with patients, promoting coexistence, participating in their treatment, and fostering comprehensive learning (Kerebih, Salelew, & Hailesilassie, 2019; Lyons & Janca, 2015). Various guidelines have been established to achieve objectives within the medical student’s training (Sartorius et al., 2010).
An effective educational plan that favors contact with patients with mental disorders at different stages of the course of their illness could reduce stigma and continue to sensitize clinicians on the subject during other stages of their training (Eksteen et al., 2017; Oliveira et al., 2020). In addition, it could be extended to the rest of the medical specialties (Eksteen et al., 2017). Unfortunately, although there are studies carried out in the Mexican population that describe the attitudes towards mental illness in the general population (IESM-OMS, 2011), we did not find studies that describe the opinions of medical students in Mexico. The objective of our study was to measure and compare medical students’ attitudes toward mental illness at the beginning and the end of their Psychiatry course.
METHOD
Study design
This investigation was observational, cross-sectional, descriptive, and open.
Subjects
The participants were students in their fifth year of Medicine of the same university who took the Psychiatry subject; their participation was anonymous and voluntary, and they were told that they could end their participation at any time if they wanted to.
Place
The authors invited the students to answer the MICA-2 scale in their classroom during their Psychiatry course’s first and last classes.
Course characteristics
The Psychiatry course has 20 weeks and is developed over five months. The academic program is designed so that students attend theoretical and practical classes. The massive theoretical classes (300 or more students) have a frequency of one to two weekly sessions of 1-hour duration, and expository-type strategies are implemented. The practical part of the course includes case review workshops in small groups (30 students) once a week. The objective is to practice a theoretical and practical discussion of cases through live or video-recorded interviews with patients who present psychiatric pathology. In addition, students perform two shifts per semester in the emergency services and the hospitalization area of the hospital’s Psychiatry department attached to the Faculty of Medicine.
Measurements
The instrument used was the Scale of Clinicians’ Attitudes towards mental illness, version for medical students (MICA-2; Kassam et al., 2012). It is self-applicable and consists of 16 items, with responses on a 6-point scale; possible scores range from 16 to 96, and higher means more negative and stigmatizing attitudes. Moreover, it has good internal reliability in the original study, with a Cronbach’s alpha of .79.
Procedure
The students were asked to voluntarily participate; to avoid possible biases, their participation was anonymous. Sociodemographic information was collected, and the MICA-2 scale was applied initially and once again after the students finished their course, which lasted for five months.
Additionally, we asked the students to answer a question that explored their interest in learning more about mental illness. The question was exploratory, with answers on a Likert-type scale, with the following options: “agree,” “moderately agree,” “neutral,” “moderately disagree,” and “disagree.”
Statistical analysis
We compared baseline measurements of demographic and clinimetric variables between groups to control for possible biases. For the difference concerning the change between the final and baseline score on the MICA-2 scale, the t-test was used for paired data, given the equality of variances of the sampling distributions.
Furthermore, Pearson’s chi2 tests were performed for categorical variables such as gender, origin, occupation, academic condition, and residence condition in an exploratory and secondary way. All information was analyzed with the statistical software JMP 13.
Ethical considerations
The Institutional Ethics Committee reviewed and approved the study (PS15-001). There was no potential harm to participants, and the anonymity of participants was guaranteed.
RESULTS
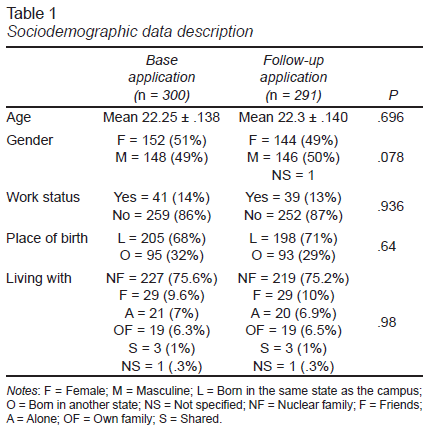
Three hundred thirty students were invited to participate in the research, of which 300 participated in the initial application and 291 in the follow-up, with a participation rate of 97%. There was a similar gender distribution in both applications: in the initial one, 152 (51%) were men, and 148 (49%) were women; in the follow-up, 146 (50%) were men, and 144 (50%) were women. One student did not answer the section corresponding to gender. The mean age was 22 ± 2 years, within a 20-30-years range (Table 1).
Most of the participants reported to be full-time students, and most were born in the city where the medical school is located; almost a third of them were from other cities. In addition, most of the students lived with their families of origin.
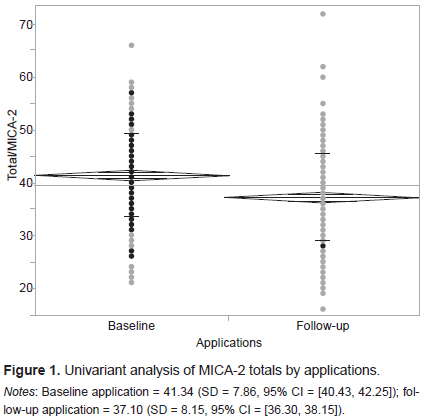
In the initial application, the MICA-2 average score was 41.34 (SD = 7.86, 95% CI = [40.43, 42.25]), with a maximum score of 66 and a minimum of 21. In the follow-up application, the mean was 37.10 (SD = 8.15, 95% CI = [36.30, 38.15]), with a maximum of 62 and a minimum of 19. We found a reduction in the mean scores between the initial and final application. In general, the stigmatic attitudes decreased (Figure 1). We found that this decrease was unaffected by gender, age, and the other demographic variables.
After finishing the course, the difference between the baseline and final applications mean scores was -4.11 (p = ≤ .0001). In our subjects, the MICA-2 scale had a Cronbach’s alpha coefficient of 69 (rounded), which is considered acceptable and similar to the previously reported (Kassam et al., 2012).
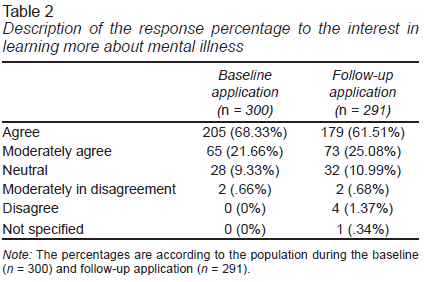
The response of the question on the interest in learning more about mental illness was as follows: 270 students (89.99%) mentioned agreeing or moderately agreeing with that statement, and 28 (9.33%) answered having a neutral position. It is important to note that only two students (.66%) mentioned that they moderately disagreed and that none of them said they disagreed.
However, on the follow-up application, there was a decrease in the number of students who agreed (252 students, 86.59%). There was an increase in the neutral responses (32 students, 10.99%) and students’ responses disagreeing or moderately disagreeing (6 students, 2.05%; Table 2).
DISCUSSION AND CONCLUSION
The results obtained on the MICA-2 scale are encouraging; compared with other published studies, a positive influence of academic courses on stigma in mental health was observed. The mean score at the baseline application was 41.25, (95% CI 40.43, 42.25), while at the end it became 37.10 (95% CI 36.30, 38.15). with non-overlapping confidence intervals, indicating that the stigma towards mental illness decreased after completing an academic period of 20 weeks. The academic course should be long enough to implement interventions and measure responses (Borg, Testa, Sammut, & Cassar, 2020; Hankir, Fletcher-Rogers, Ogunmuyiwa, Carrick, & Zaman, 2020) , even though some studies have reported changes after a 15-day rotation (Desai et al., 2019).
Additionally, when comparing these scores with those obtained in other studies, it seems that there is a lower presence of stigmatizing attitudes in our population. For example, in a study with students from central and eastern Europe, the authors obtained means of 38.1, 40.2, and 43.1 (Janoušková et al., 2021); conversely, in a study with a French population, the means obtained were 41.4 and 43.5 (Simon & Verdoux, 2018). The decrease in the follow-up scores can be considered an indicator of the decrease in the students stigmatizing ideas. These results are consistent with the literature (Babicki, Małecka, Kowalski, Bogudzińska, & Piotrowski, 2021; Desai et al., 2019; Masedo et al., 2021). Similarly, Simon and Verdoux (2018) report significant changes after an educational program with Psychiatry and Neurology students. Thus, it seems that stigmatizing attitudes can be reduced by an educational program, having a more marked positive impact when it is concomitant with supervised clinical practice (Simon & Verdoux, 2018) and proper guidance during their clerkships (Petkari, Masedo Gutiérrez, Xavier, & Moreno Küstner, 2018; Potts et al., 2022).
Among the various interventions to prevent stigma (Corrigan et al., 2018; Pandian et al., 2020; Rüsch & Kösters, 2021), direct contact with people with mental illness appears to be more effective than education with video exposure (Gervás et al., 2022) and group discussion (Pandian et al., 2020), which have shown high efficacy (Heim et al., 2019; Rezvanifar, Shariat, Shalbafan, Salehian, & Rasoulian, 2022). Our results suggest that it may be necessary to enrich educational interventions with more significant interaction with patients (Lien et al., 2021; Sandhu, Arora, Brasch, & Streiner, 2019), considering that the most appropriate strategies allow such coexistence in an educational context that prioritizes the clarification of beliefs and the detection of preconceived stigmatizing attitudes (Balon et al., 2017; Heim et al., 2019).
It has been suggested that to consider that interventions to prevent stigma are a success, they should be continuously evaluated for the persistence of the knowledge acquired (Pandian et al., 2020) with the use of more sophisticated instruments and even more intense interventions (Sandhu et al., 2019; Waqas et al., 2020). Interestingly, the proportion of reported interest in learning more about mental illness decreased. It is baffling that some students even disagreed with learning more; this could imply that other seminar or academic staff variables needed to be considered, such as satisfaction with the learned content or their interest in learning more about other medical specialties (Meng, Huang, Wang, Wang, & Wang, 2022). We could even hypothesize that the students who are not interested in specializing in Psychiatry may not wish to continue learning more about the subject (Meng et al., 2022; Potts et al., 2022).
Thus, it is possible to implement a simple intervention to improve the quality of the educational experience by bringing students closer to psychiatric clinical practice with more meaningful guidance and accompaniment from the professionals working in the institution. Also, collaboration with different disciplines with intervention design and application is of utmost importance, such as psychology, sociology, social work, etcetera. The most successful intervention should result from interdisciplinary work (Babicki et al., 2021; Corrigan et al., 2018; Potts et al., 2022).
Limitations
Among the limitations of this study, some are that it was developed in only one generation of students after one seminar and only in one medical school (Gervás et al., 2022; Lien et al., 2021; Waqas et al., 2020). Furthermore, no questions were asked about the students’ previous exposure to people with any disease or their representation by the media. It has been reported that having previous experience with medical or mental illnesses and how the media portrays psychiatrists could influence the choice of specialty (Babicki et al., 2021; Meng et al., 2022; Potts et al., 2022; Rezvanifar et al., 2022).
Although it had an internal consistency of .6859, and we used the recommended Spanish-translated version of the scale, it has not been validated yet in the Mexican population.
Other factors that were not included in the present study and that would be worth reviewing in subsequent studies are the history of contact with patients with psychiatric illnesses, having a relative who receives mental health care. Also, factors more closely related to the educational process include the teacher’s role, group size, program content, type of material reviewed, and teaching strategies.
It is possible to modify medical students’ attitudes towards mental disorders after taking a Psychiatry course if the people in charge of their learning show disposition and closer supervision during the clinical rotations.
However, there was a decrease in the response percentage of the interest to learn more about mental illness, suggesting that more variables were not considered.