INTRODUCTION
The World Health Organization (WHO, 2021) describes depression as a mood disorder characterized by a predominantly low and/or irritable mood, with a variety of symptoms, which can include ‒but is not limited to‒ significantly diminished interest or pleasure in all, or almost all, activities, excessive or inappropriate guilt, feelings of worthlessness, hopelessness, lack of motivation, weight loss or weight gain, increased or decreased appetite, psychomotor retardation, insomnia or hypersomnia. Thus, it does not only affect the person who suffers from it, but their entire environment, including his/her partner, family, friends, etc. Literature indicates that 9.2% of the general population has suffered at least one depressive episode, and that one out of five persons will present one before the age of 75 (Wagner et al., 2012). The WHO (WHO, 2021) established depression as the leading global cause of disability.
Depression, in the context of pregnancy, can have important repercussions on self-care and on the developing baby, and can even culminate in maternal death due to suicide or complications from the mother’s comorbidities (Jadresic, 2014). Another possibility is the death of the mother-baby binomial. Deaths by suicide are a leading cause of maternal mortality in the United States. Yet, the prevalence and trends in suicidality (suicidal ideation and/or intentional self-harm) among pregnant women remain poorly described. Suicidal ideation and intentional self-harm, one year before and after giving birth, increased significantly between 2006 and 2017. Those with depression, had larger escalations (Admon et al., 2021). Other possible consequences are emphasized by Mitchell et al. (2023), including preterm birth, substance use, continued depression and anxiety; once again, mentioning suicide. Whatever the outcome, it would indisputably have a severe impact on the woman’s environment. Vázquez-Rojas (2020), in a study carried out in the city of Hermosillo, Sonora, in patients who had attempted suicide, observed that the diagnoses of major depressive disorder and persistent depressive disorder were presented in 30% and 14%, respectively. Although this study was not conducted in pregnant women, but rather men and women, it highlights the great influence of depressive disorders on a possible fatal outcome and contributes to local statistics.
Furthermore, depressed pregnant women are at greater risk of neglecting their pregnancy, abandoning prenatal care or not carrying it out properly, or not following medical instructions or following them erroneously, compared to non-depressed pregnant women. Additionally, they are more exposed to possible substance abuse such as tobacco, alcohol, and drugs in general, which can affect the obstetric outcome, with significant repercussions on the binomial. In turn, some depressive symptoms such as anorexia or hyporexia, can alter some aspects of the pregnancy and contribute to adverse results; for example, the expected weight gain. There exists an underdiagnosis of depression from early stages of pregnancy (Jadresic, 2014). The American Psychiatric Association (APA) did not mention perinatal depression prior to its fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). In said edition, it is included as a specifier “major depressive disorder with peripartum onset” (APA, 2013). However, it does not differ from a depressive disorder in other contexts. That is a rather relevant matter, since, as Lartigue et al. (2008) describe, the consequences of perinatal depression can have a much bigger impact than other subtypes of depressive disorders. The National Institute of Mental Health (NIMH) states that perinatal depression does not have a single cause. Instead, research suggests that it is a result of a combination of genetic and environmental factors. Life stress, the physical and emotional demands of childbearing and caring for a new baby, and changes in hormones that occur during and after pregnancy can contribute to the development of perinatal depression. (NIMH, 2020). Postpartum depression is a topic generally better explored than depression during pregnancy. However, it should be noted that the APA states that about 50% of postpartum major depressive episodes, begin prior to delivery. The APA also states, in its most recent edition of the Diagnostic and Statistical Manual of Mental Disorders ‒Fifth Edition, Text Revision‒ (DSM-5-TR), that approximately 9% of women will experience a major depressive episode between conception and birth (APA, 2022). Morales and collaborators describe in their study conducted on pregnant women treated at the Instituto Nacional de Perinatología (INPer), in Mexico City, that the prevalence of probable depression was 17.8% (Morales et al., 2004).
Unfortunately, there are not enough records on this matter; although there are some figures in certain regions of the country, there is nothing similar at the regional or local level in the state of Sonora. Unfortunately, there are not enough records on this matter; although there are some figures in certain regions of the country, there is nothing similar at a regional or local level in the state of Sonora.
As evidenced in the literature, the presence of depressive symptomatology in this population is high and, on several occasions, enough attention is not given by patients and/or clinicians (Ortega et al., 2001). Previous undiagnosed depressive episodes have also been uncovered in the outpatient service of the Hospital Psiquiátrico “Cruz del Norte” (HPCN), in Hermosillo, Sonora, particularly in the perinatal and childhood history, which have sometimes led to complications in pregnancy and poor attachment after birth. In addition, a deterioration in self-care has been observed, which may be associated with greater use of tobacco, alcohol and illicit drugs, little physical activity and not adequately carrying out prenatal care (Gaviria et al., 2019). By performing an intentional search for depressive symptoms, it could be detected and addressed promptly.
The present work was conducted during the third quarter of 2021 at the Hospital Infantil del Estado de Sonora (HIES), particularly in the Hospital Integral de la Mujer del Estado de Sonora (HIMES) service. The detection of depressive symptomatology was sought by applying the Edinburgh Perinatal Depression Scale (EPDS) to pregnant women who were in the second or third trimester, with no prior diagnosis or treatment of affective disorders.
The aforementioned scale is self-applied and consists of 10 items, which evaluate the patient’s affective state in the two weeks prior to its application. It is focused on screening for depressive symptoms exclusively in women during pregnancy and postnatal period, being the only one of its field to have been validated in Mexican context (Lartigue et al., 2004).
Thereupon, avoiding the consequences of presenting depressive symptoms during pregnancy can be essential for the mother-child bond, as well as for the entire family, due to the type of effects they yield on them. By neglecting their pregnancy due to depressive symptoms, undoubtedly, the problem can be rather critical.
Hence, the objective of this research was to determine the prevalence of depressive symptoms in pregnant women treated at HIES/HIMES. The obtained information could work as a base for new protocols focused on the detection and treatment of depression during pregnancy and the arising of its consequences.
METHOD
Design of the study, subjects, and places
During the third quarter of 2021, an observational, descriptive, transversal, and prospective study was carried out in 168 pregnant women, treated at HIES/HIMES in Hermosillo, Sonora, selected by non-probabilistic sampling by consecutive cases. They all were in the 2nd/3rd trimester and had no previous history of affective disorders diagnosis and/or treatment. HIES is a hospital located in Hermosillo city, Sonora, providing secondary and tertiary health care and an estimate of 4000 deliveries per year take place there (Secretaría de Salud Pública del Estado de Sonora, 2019). All participants had the right to voluntarily participate in the study. The inclusion criteria were women in fertile age who were able to fully understand and respond the contents of the EPDS. Given the high prevalence of adolescent pregnancy receiving medical care at HIES, we decided not to exclude this age group. Apart from those who were unable to read and write, the exclusion criteria, in order to avoid possible biases caused by diagnoses such as bipolar depression or treatment-resistant depression, exclusion criteria were women with a previous diagnosed affective disorder and/or who had received treatment for depressive symptoms. The purpose of this study was not to assess the therapeutic efficacy of pharmacological and/or psychotherapy treatment, as it has already been proved effective for depression, but rather to detect those women with compatible symptoms who could have otherwise been left undetected and their current overall state. It is also important to state that, had they presented an affective disorder before, it could have led them to this point. Hence, the importance of making this a first episode exploration, to the extent possible.
Procedure
Sample size was determined based on a proportion of depressive symptomatology of 17.8% reported in a previous study in Mexico with similar characteristics, using the Edinburgh Perinatal Depression Scale (EPDS; Morales et al., 2004). However, since the findings were diverse –sometimes higher, sometimes lower– we opted for a proportion of 12.5% as a middle point for the sample, with an assumption of 95% confidence interval (CI), a 5% margin of error, and a final sample size of 168. The working hypothesis was based on the aforementioned study (Morales et al., 2004) looking for a 17.8% prevalence or lower. The EPDS was used to assess the potential depressive symptoms. If a score of 14 points or higher was reached, the patient was considered as “probable perinatal depression”. Any patient reaching said score, was given a results certificate and was referred to the nearest available psychiatry service, while this was not the objective of the study per se. Besides, a clinical and demographic questionnaire was applied in order to get information about general medical history, use of tobacco, alcohol consumption and use of illegal drugs, as well as gynecologic-obstetric history. Prior substance abuse disorders were ruled out during the interview.
Data were collected by means of a pretested, face-to-face interviewer-administered structured questionnaire. The questionnaire included three sections: sociodemographic characteristics, gynecological-obstetric, family and social factors. Sociodemographic characteristics included age, educational status, ethnicity, current marital and occupational status. Also, information about past and current domestic violence was examined. As for ethnicity, this was considered a relevant matter, since HIES treats many people of different ethnicities, and, as any minority, they are more exposed to adverse conditions, including violence, which, by itself, produces stress and trauma; although violence is not exclusive to them.
Obstetric factors included number of pregnancies, deliveries, caesarean deliveries, abortions, whether or not the current gestation was planned and/or desired, gestational age, menarche, and number of sexual partners. Personal medical history included systemic arterial hypertension, type 2 diabetes mellitus, hypothyroidism, syphilis, or other diseases. Besides, alcohol, tobacco, and illegal drugs were investigated during current pregnancy, such as smoking and number of cigarettes per day, alcohol drinking and number of drinks per day, as well as drugs use, type of drugs, and frequency.
Measurements
The EPDS is a screening tool for perinatal depression symptoms but does not give a definitive diagnosis of depression (Cox et al., 1987). It is a simple, free to use tool with a sensitivity and specificity of 84.6% and 77.0% respectively, and a Cronbach’s reliability coefficient of .85 (Cox et al., 2014). The EPDS comprehends 10 items, each of which describes a specific symptom of depression with a four-point Likert-scale response option (‘most of the time’, ‘sometimes’, ‘not often’, ‘never’) scored 0–3, with a total score ranging from 0 to 30. The cut-off value of 14 was used to identify pregnant women with considerable depressive symptoms (Morales et al., 2004; Oquendo-Cortez et al., 2008). The EPDS is the most commonly used screening tool in pregnancy as it does not include the somatic symptoms of pregnancy such as nausea, headache, appetite or weight changes that are all symptoms associated with depression and may result in higher depression scores (Chorwe-Sungani & Chipps, 2017). It is also particularly recommended for low-resource settings for screening for perinatal depression because of its potential to detect common perinatal mental disorders in culturally diverse low-income and lower middle-income countries, since its validity and reliability have been studied in these settings and found to be acceptable (Stewart et al., 2013).
Statistical analyses
Data were coded and exported into Statistical Package for the Social Sciences (SPSS) for recoding, categorization, and statistical analysis. Data were summarized using descriptive statistics such as frequency and percentages for categorical data, and for mean and standard deviation (SD) and range for numerical data. A prevalence of the depressive symptomatology was estimated and its confidence interval was set at 95%. Subsequently, this was adjusted for variables such as: age, marital status, education, occupation, domestic violence, trimester of pregnancy, planned/desired pregnancy, alcohol consumption, use of tobacco and illegal drugs, among other gynecologic-obstetric variables. The SPSS 25.0 (SPSS, Chicago, IL, USA) was used for all statistical analyses.
Ethical considerations
The research was conducted according to the highest ethical standards in accordance with the Declaration of Helsinki, and national ethical and legal requirements. The HIES Institutional Research Ethics Committee authorized the protocol (registry N. 002/21), and also all participants signed an informed consent form prior to inclusion in the study, which could be revoked at any time. Underage participants were required to be accompanied by her guardian, who, apart from the participant herself, signed the informed consent document. The objectives and implications of the study were explained in detail to underage participants, asking them for any questions they had and to paraphrase what was told to them, in order to ensure they fully understood the study.
RESULTS
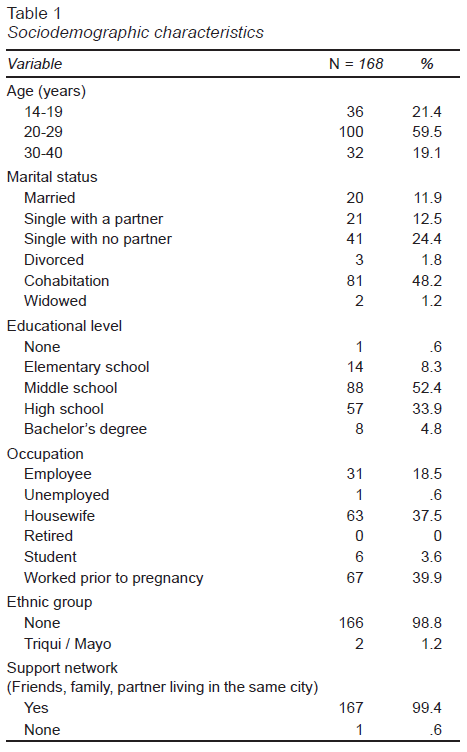
The sample size was 168 patients. None of them were eliminated from the study, so the expected sample was completed and remained intact. After obtaining the complete sample, patients were classified into three age groups. From 14 to 19 years, from 20 to 29 years and 30 years or older. Thirty-six (21.4%) corresponded to the 14-19 age group; most of them, 100 (59.5%), were in the 20-29 age group; finally, 32 (19.1%) classified in the group of 30 years or older. The important proportion of young people between 14 and 19 years of age is worth noting. Sociodemographic characteristics, such as marital status, educational level, ethnic group, support network (whether or not they had social/family support in their city), for the full sample are stated in Table 1. While there is no specific data on their socioeconomic background, it is specified that, those with a partner, said the partner was their provider at home. Regarding single women without a partner, it was the parents who provided.
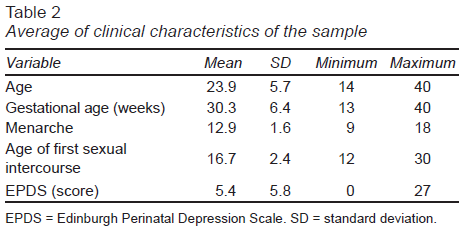
Regarding the average clinical characteristics of the pregnant women interviewed in this study, the average age was 23.9 years, with a standard deviation (SD) of 5.7, with a minimum of 14 and a maximum of 40 years. The rest of these variables, including the EPDS score, are described in Table 2.
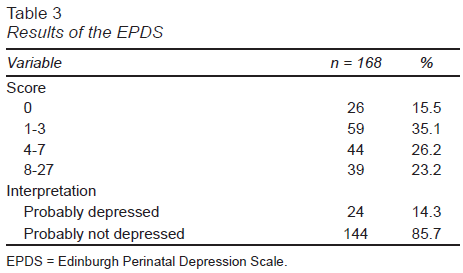
Elaborating on the results of the EPDS, 26 (15.5%) patients obtained a score of zero. Fifty-nine (35.1%) obtained a score of 1-3. 44 (26.2%) patients had a result of 4-7 points. Thirty-nine (23.2%) resulted with 8-27 points. Taking into account the cut-off value established at 14, regarding probable depression / probably without depression, 24 (14.3%) patients obtained a score past this value; while 144 (85.7%) remained below it. Reiterating, a 14.3% prevalence of depressive symptoms (probable depression) was obtained among the women in the study (Table 3).
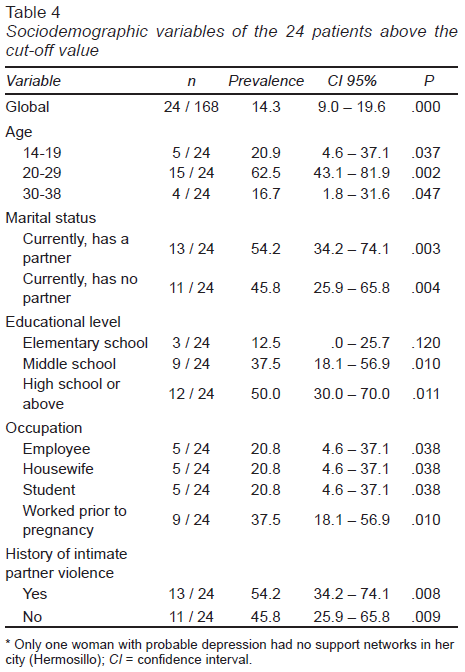
Subsequently, the prevalence is detailed according to different variables of the patients. The overall prevalence was 14.3%, with a 95% confidence interval (CI) of 9.0 – 19.6, statistically significant with a P value of < .001. Regarding these 24 patients above the cut-off value, the sociodemographic variables are established in Table 4.
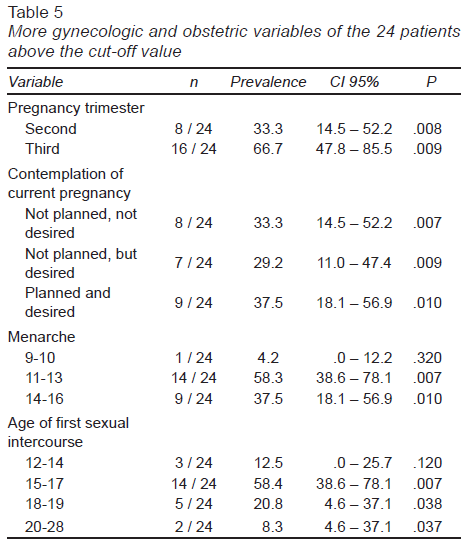
Apropos to the gynecologic and obstetric variables of the 24 patients, among them, 12 (50%) claimed to have had one or two sexual partners. Seven of them (29.2%), answered three; five claimed having had four or five sexual partners. As for the number of gestations, including the current one, nine (37.5%) were going through their first pregnancy; six (25%) were experiencing their second pregnancy; five (20.8%) were on their third pregnancy; and four, were experiencing their fourth or fifth one. As for previous vaginal deliveries, 15 (62.5%) had had none, five (20.8%) had had one; and four (16.7%) had had two or three. The rest of these variables are described in Table 5.
Concerning the personal history of illness and substance use in these 24 patients: three (12.5%) had a diagnosis of arterial hypertension; three (12.5%) had type 2 diabetes mellitus; two (8.3%) had a history of syphilis, which had been treated; two more patients (28.3%) had a diagnosis of hypothyroidism. As for the current weight of the patients, only seven (29.2%) were in a status of normal weight, according to their body mass index, with 17 (70.8%) overweight or obese (overweight predominating in 58.3%). Regarding the consumption of substances, all of them stated that they did not know about their pregnancy the last time they consumed them. Thirteen (54.2%) reported alcohol consumption, 10 (41.7%) reported tobacco use, and seven (29.2%) acknowledged to an illegal substance use (marijuana).
DISCUSSION AND CONCLUSION
The objective of this study was to determine the prevalence of depressive symptoms in pregnant women treated at HIES. For this, the EPDS was used, with a cut-off value of 14. When this result was obtained, it was classified as “probable perinatal depression”; this is what, in this study, was considered for the prevalence of depressive symptoms.
The sample size was 168 patients, of which 24 resulted with “probable perinatal depression”, that is, 14.3%. It is worth mentioning that Wagner et al. (2012) state that 9.2% of the general population has suffered at least one depressive episode; specifically, existing an underdiagnosis of depression from early stages of pregnancy. The obtained percentage in this study, is clearly higher than the aforementioned data.
Regarding general characteristics of the sample, in partner violence, the majority denied it in current and previous partners. In the study conducted by Aguilera-Ortiz (2022) on intimate partner violence in Sonora, the largest group was 20-24 years old, similar to the age group found in this study, with a history of violence.
The global prevalence was 14.3% (24 patients out of 168). Lartigue et al. (2004), using the same scale, reported a prevalence of approximately 17%, although using a lower cut-off value (12-13). It is important to compare it with that reported by Morales et al. (2004), since it was there that the cut-off value was adjusted to a stricter one, obtaining 17.8%. Compared with the study in Mérida from Rodríguez-Baeza et al. (2017), in which a prevalence of 16.6% was reported, the prevalence in this study was slightly lower.
The prevalence in Sonora was considerably higher than that reported in Quintana Roo by Ceballos-Martínez et al. (2010); that is, 6.4%. The results for Sonora were similar to those reported by Sumano-López and Vargas-Mendoza (2014) in Oaxaca (14%). Gaviria et al. (2019) describe in a similar population regarding age and sociodemographic characteristics, in Colombia, the prevalence of perinatal depression between 14-23%, mentioning that it increases as pregnancy progresses. These differences are possibly related to cultural differences; even in the same country, culture differs vastly. Also, Sonora, being close to the United States, is also influenced by its culture. There is not much information available regarding depression during pregnancy, but Dagher et al. (2021), report its prevalence in the United States as 8.5-11%, which is lower than in Sonora. Although some culture traits might be shared, sociodemographic settings tend to be worse for Mexico. The same authors describe higher perinatal depression rates in Hispanic women living in the United States. Perhaps genetics plays an important role here, though we don’t know the context of these Hispanic people. Still, genetics has been and continues to be researched in matters of mental health (Dagher et al., 2021). Moreover, Mitchell et al. (2023) describe that depression is common in low- and middle-income countries, affecting one in four perinatal women, although it remains an understudied field.
Of the 24 patients in question, 54.2% reported having a partner, whether it was cohabitation, marriage, or in a relationship in general. This is consistent with what Rodríguez-Baeza et al. (2017) reported, since they mention that living in cohabitation was identified as a risk factor, and most of the patients in the sample in this study were in said situation. The same authors describe marriage as a protective factor. They also state marriage is considered more of a protective factor than cohabitation, since the commitment in marriage tends to be great than in cohabitation. However, this needs to be taken carefully, since other factors might interfere. For example, a married couple may stay married and together even if they don’t want to, anymore, because of legal implications and matrimonial assets, whereas cohabitation could be easier to end, if desired.
Referring to intimate partner violence, 54.2% reported some type of prior partner violence (physical, psychological, etc.); two of them mentioned it with a previous and current partner; Two more patients referred only with current partner. This information is consistent with what was reported by Silva Lima et al. (2020), mentioning that pregnant women with depressive symptoms have a higher average level of violence than those who did not present these symptoms.
Regarding the type of violence reported in this study, a specific instrument was not applied to explore it; it was only explored verbally. There was a predominance of psychological violence such as insults during arguments, the prohibition of certain types of clothing or having male friends, looking through mobile phones, social networks, etc.
Rogathi et al. (2017), in their study, noted that exposure to domestic violence at least once increased the risk of postpartum depression more than threefold. In fact, two of the strongest predictors of postpartum depression were prenatal depression and current abuse with an odds ratio of three or higher (Norhayati et al., 2015; Wu et al., 2012 as cited by Hutchens and Kearney, 2020).
Said information could work as a predictor of the prognosis of women who presented domestic violence, being more than half of the 24 patients in question. While local statistics do not describe types of violence and the outcome regarding pregnancy and depression, physical/sexual violence may directly lead to unwanted pregnancies, and psychological violence could increase emotional vulnerability, low self-esteem or malaise in the victims.
Concerning ethnicity, Benítez-Pinto and Puente-Peñaranda (2021) explored postpartum depression, finding that 64% of depressed patients corresponded to mestizo patients, 34% to indigenous patients and 2% to white patients. However, when analyzing each of the groups, they found that, of the 100% sample of indigenous patients, 77% presented postpartum depression compared to 23% without depression; finding a statistically significant relationship P = .08 in relation to the indigenous patients. While this does not refer to depression during pregnancy, the fact that about 50% of postpartum major depressive disorders actually begin prior to delivery, needs to be seriously considered (APA, 2022). Dagher et al. (2021) mention racial/ethnic disparities in accessing perinatal depression screening and treatment services as an understudied research area.
Regarding support networks, the only woman in the sample who reported not having friends or family in the city scored for probable depression, which is consistent with the bibliography that describes support networks as a protective factor against depression, described by authors such as Krauskopf and Valenzuela (2020). In Sonora, amicability is rather common, being part of cultural context, which may, in turn, increase patients’ support networks.
Turning to educational level, it should be noted that 50% of the 24 patients reported a maximum level of high school studies, which is striking, since the bibliography usually mentions that the lower the level, the greater the probability of scoring above the cutoff, as pointed out by Morales et al. (2004) and Chan-Vázquez (2012). In addition to this, it is not overlooked that a large part of the patients had middle school as top reached level, being an important point described by Contreras-Carreto et al. (2022), who report that this situation is a risk factor with an OR of 5.61, specifically in Mexican population.
As for the trimester of pregnancy, 66.7% of the 24 patients with probable depression corresponded to the third trimester, consistent with Gaviria et al. (2019), who stated perinatal depression increases along with gestation time itself, possibly due to the expectations and qualms about the pregnancy being over and moving forward to the next stage, along with the psychosocial demands Aguilar-Abrego (2008) describes. It is observed that most of the patients with probable depression reported having desired the current pregnancy. This does not correspond to what is usually reported about unwanted pregnancies as a greater risk factor for depressive symptoms, when compared to the desired ones. Rodríguez-Baeza et al. (2017), similarly, describe a fairly similar proportion between whether the pregnancy was planned or not, in women with probable depression, which, apparently, shows that there is no major difference with respect to possible subsequent depression.
In this sample, being primigravida predominated in those with probable depression. However, among those who were not primigravida and had probable depression, the predominance was not having had previous vaginal deliveries.
Ceballos-Martinez et al. (2010) reported the opposite, as a history of previous vaginal deliveries predominated in pregnant women with probable depression. Morales et al. (2004), as well as Contreras-Carreto et al. (2022) describe that the greater the number of gestations, the greater the probability of depression, which was not demonstrated in this study.
Turning to the personal history, out of the five patients with hypothyroidism (of the total sample), two had results of probable depression. The relationship between thyroid function and mood disorders has been described for more than 50 years (Caneo et al., 2020). However, all patients with hypothyroidism were in adequate control, according to their most recent thyroid function tests.
Among the patients with probable depression, 70.8% were overweight or obese, which is transcendental, due to findings that not only speak of an increased risk of depression due to being overweight, but also of consequences for offspring (Cattane et al., 2021). However, these findings should be taken with caution in the present study, since there is no previous information regarding overweight or obesity in patients.
Regarding substance use, 54.2% had a history of alcohol use, at least before pregnancy. More than half of the patients in the Rodríguez-Baeza et al. (2017) study had a history of alcohol use. About tobacco consumption, 41.7% referred it, being similar to what was found by Rodríguez-Baeza et al. (2017) and Contreras-Carreto et al. (2022). Finally, 29.2% had a history of use of illegal substances. This shows that most of the patients with probable depression had a history of some type of substance use. Despite the mention of substance use prior to pregnancy, during the clinical interview, the context in which they came to use the substances was intentionally sought, ruling out criteria for a substance use disorder.
The referred consumption occurred in social situations, denying that it functioned at any time as a negative reinforcer. This type of reinforcer happens when the consumption is sought in order to eliminate or attenuate discomfort, being the consumption that usually occurs in depressive disorders (Wise & Koob, 2014). Although the fact that consumption occurs as a positive reinforcer does not rule out an affective problem, this study did not find a relationship between substance use and a possible previous depressive episode. However, it does not exempt them from complications in the future.
Contreras-Carreto et al. (2022) emphasize several determinants that affect maternal mental health. Among them are minimization of symptoms [by the patient, family and/or health care provider], abandonment of a partner, lack of support networks, a history of any type of abuse, which have been identified in a large part of the 24 patients suspected of depression.
Sociodemographic factors did not predict prevalence of postpartum depression in a cross-national meta-analysis and meta-regression, according to Hahn-Holbrook et al. (2018), whose findings showed that nations with higher wealth inequality, higher risk of maternal or infant mortality and higher percentages of young women working ≥ 40 h a week, were the nations with the highest prevalence of perinatal depression, drawing the attention to macroeconomic and health conditions as important predictors of depression in perinatal period. Mexico’s prevalence of perinatal depression in this analysis was in the mean -19%- of all considered nations, which is consistent with our findings.
Regardless of the score, 100% of the pregnant women with probable depression mentioned that they had been told that what was happening to them was “normal” and some even mentioned that they were told that they should “put up with it” sic, because it was “what was expected”. This falls within the minimization of symptoms, previously described. Aguilar-Abrego (2008) talks about these expectations and social demands and how they have an important impact.
As Aguilar-Abrego (2008) states, there are different psychosocial demands. One of the expected biological objectives is the birth of a healthy child and as a psychosocial objective, the new mother is expected to grow and mature as a woman, reflecting this by being “unconditionally strong” and not showing any difficulties, even if present. However, each culture has strong beliefs about proper conduct in pregnancy. These expectations must be adopted by the pregnant woman, since society demands and if said woman does not respond, she is usually judged. For this reason, it is not uncommon for women to minimize their own symptoms or try to ignore them, since they have been taught that they must comply with these social demands, sometimes as part of their own worth.
Adlington et al. (2023) talk about loneliness as a central role in the experience of perinatal depression. It is particularly described that issues relating to the interaction between perinatal depression and loneliness included self-isolation and hiding symptoms; this, due to stigma of perinatal depression and fear of judgment as a “bad mother”; a sudden sense of emotional disconnection after birth; and a mismatch between expected and actual support provided by partner, family, and community. They strived to be a “perfect mother”. There was a sense that they were expected to be happy and relishing their role as a new mother. Additionally, a double burden of loneliness was identified for women from disadvantaged communities, due to increased stigma and decreased social support. Some of the testimonies said they were told to “just snap out of it” when they were feeling uneasy. A quote from these testimonies was “and my husband would always really try to tell me to be more cheerful, but it would always seem impossible and of course it added to more guilt on my part”. Telling pregnant women to “just put up with it” when they’re not feeling well is, unfortunately, rather common in many cultures, as was seen in these women in Hermosillo, Sonora.
Lartigue et al. (2008) describe the difficulties that pregnant women go through, with several of them being presented by the patients in this study. Some particular cases reported that part of what increased their symptoms were changes in their autonomy. As can be seen, numerous variables can influence how women feel during pregnancy. Mareckova et al. (2023) assessed a 30-year follow-up of a Czech prenatal birth cohort with a within-participant design neuroimaging component in young adulthood conducted from 1991 to 2022, in the offspring of mothers in context of maternal depression and stressful life events in the past year experienced by the young adult offspring. A gap between estimated neuroanatomical vs. chronological age at magnetic resonance imaging (MRI) was identified. This gap was calculated once in participants’ early 20s and once in their late 20s, and pace of aging calculated as the differences between brain age gap estimation at the 2 MRI sessions in young adulthood. They state that maternal depression and recent stress may have independent associations with brain age and the pace of aging, respectively, in young adulthood. Thus, they present more evidence that prevention and treatment of depression in pregnant women may have long-term implications for offspring brain development.
All 168 patients were provided with information on affective disorders and what to expect in their pregnancy, in addition to answering any questions they might have had. As a result, 100% of them appreciated feeling listened regarding their pregnancy experience.
It is important to mention that this study focused on detection of pregnant women who had ongoing depressive symptoms, as well as psychoeducation, not actively treating them at the moment. As mentioned before, they were referred to the psychiatry service. Still, it is imperative to state some of the available options for treatment. Numerous patients with mild-moderate depression can respond to psychotherapeutic interventions. Wenzel and Kleiman (2015) have described the usefulness of cognitive-behavioral therapy in pregnancy and postpartum, as has Spinelli (2017) with interpersonal therapy. In moderate-severe depressions that have not responded to psychotherapy or are considered to have a high probability of recurrence, pharmacotherapy is used; the evidence indicates that selective serotonin reuptake inhibitors ‒preferably avoiding paroxetine‒ are a good therapeutic option (AILANCYP, 2021).
The working hypothesis was met, since the present study demonstrated a prevalence of depressive symptoms of 14.3%, similar to that described by various authors, also corresponding to other variables such as age group, lack of support networks, marital status, and contrasting with results such as a lower prevalence of depressive symptoms in adolescent pregnancy. In addition to this, the results are consistent with rest of the investigations carried out in Mexico and in other parts of the world, so it could be generalized.
To conclude, as Chin et al., (2022) assert, pregnancy and the first postpartum year is a period of increased access to health care for many, thus implying a greater opportunity for detection and intervention. Universal screening for perinatal depression, along with increased access to mental health services, can reduce adverse outcomes, including suicidal risk.
Taking everything into account, there is a high prevalence of depressive symptoms during pregnancy, going unnoticed for reasons such as insufficient knowledge (patient/health care providers), since there is no routine screening. It is imperative to work on prevention, detection and treatment, since it entails multiple consequences at a binomial, family and social level.
Limitations
Mentioning some limitations, while previous psychiatric history was investigated in the clinical interview and patient records, we have no certain way of knowing about previous undetected depressive episodes. Likewise, HIES/HIMES does not include the population treated in other medical services, such as the private sector. As for women who reached the minimum score of 14, even though they were given a certificate and a referral to the psychiatry service, due to matters of time and infrastructure, follow-up was not conducted by our team as a part of this study, nor full diagnoses confirmation by means of the most frequently employed instruments in our field, since they take, at least, an additional 10-30 minutes to complete and score. To mention a few, these are the Beck Depression Inventory (BDI), Hamilton Depression Rating Scale (HAM-D), and Montgomery-Åsberg Depression Rating Scale (MADRS). However, the database is held by the authors, making it possible to establish a further line of research.
Another possible limitation is that the EPDS, as efficient but plain as it is, might not be fully adjusted regarding various psychosocial factors that could act as mediators or predictors, such as ethnicity, violence, number of deliveries, and comorbidities; especially, violence, since it can potentially lead to developing post-traumatic stress disorder (PTSD) and not just depression. It is certainly an area of opportunity for new lines of research. However, since many of the participants had been exposed to some type of violence, it is imperative to say that, during the clinical interview, no PTSD symptoms were detected.