INTRODUCTION
Emergency medicine is a specialty concerning the evaluation, diagnosis, treatment and coordination of any patient requiring immediate medical, surgical or psychiatric care (Definition of Emergency Medicine, 2016). Efforts have been made in high-income countries to decrease the time spent by patients in Emergency Departments (ED), either by resolving the patient’s problem or by transferring them to another department (Obermeyer et al., 2015). According to international recommendations, a patient’s needs should be addressed within a maximum of eight hours; in the case of the United Kingdom, the maximum is just four hours (National Health Services, 2020). In Mexico, national health regulations state that a patient can be in an ED for a maximum of twelve hours (Secretaría de Salud, 2013).
In the case of low- and middle-income countries, ED stays tend to be longer. It has been reported that patients admitted to an ED experience average stays of 17 hours in Africa and 7.7 hours in Latin America. However, prolonged stays have also been described in Latin America, in some cases totaling 72 to 120 hours. These lengthy stays can result in higher care costs, saturation of ED areas, poor prognosis for patients, patients leaving the ED without being treated and higher mortality rates (Carter et al., 2014; Pearlmutter et al., 2017; Obermeyer et al., 2015).
Several factors influence the saturation of services, such as a shortage of emergency units, limited support and resources, few trained personnel, patient acuity and admission requirements, and inappropriate ED utilization by patients (Andersson et al., 2020; Carter et al., 2014; Obermeyer et al., 2015; Pryce et al., 2021). In addition to the aforementioned factors, several international studies have shown that problems such as anxiety, depression, suicidal ideation and substance abuse can contribute to overcrowding and length of stay within the ED, as these issues are reported to be among the most frequent reasons why patients go to emergency rooms (Hooker et al., 2019; Theriault et al., 2020). These problems may occur concomitantly with a chronic or acute condition, or may be the primary reason why patients decide to visit an ED (Holland et al., 2021).
ED utilization by patients with mental health and substance abuse problems has major consequences, including higher patient care costs (Yap et al., 2020), work overload, and a greater likelihood of dissatisfaction among health providers (Pearlmutter et al., 2017), and could impact the number of patient readmissions, since these patients have up to twice the number of ED visits compared to non-psychiatric patients, (Abar et al., 2017; Baia Medeiros et al., 2019; Blakemore et al., 2019). In addition, it has been observed that patients with mental health problems, previous suicide attempts, substance use and/or mood disorders (usually anxiety or depression), are 2.5 times more likely to be hospitalized and tend to have a longer length of stay (Coates et al., 2019; Santillanes et al., 2020; Smith et al., 2016).
Most of the literature on the interconnected problem of mental health and length of stay in the ED is produced by high-income countries, which usually have health systems with greater resources and a shorter average length of stay than developing countries. This could mean that existing data do not reliably describe what happens in countries such as Mexico, where it has been reported that the emergency system is characterized by a large number of patients, a shortage of beds, few people hired full-time or specializing in emergency medicine, and limited training in assessing mental health problems (Castilla-Puentes et al., 2008; Julián-Jiménez et al., 2019; Obermeyer et al., 2015). There is therefore a need for research on EDs in the context described above, to improve their preparedness for the situations that arise there. To this end, this study sought to evaluate the relationship between mental health and length of stay in patients hospitalized in a Mexico City emergency department. The association between mental health and the number of readmissions of ED patients was also evaluated. Based on previous evidence (Abar et al., 2017; Baia Medeiros et al., 2019; Blakemore et al., 2019; Coates et al., 2019; Holland et al., 2021; Santillanes et al., 2020; Smith et al., 2016; Yap et al., 2020), anxiety and depression symptoms, substance use, and suicide risk were considered the primary mental health variables for these analyses.
METHOD
Study design
A cross-sectional study was undertaken between 2017 and 2020.
Subjects / description of the sample
Sample size was calculated for a significant correlation equal to .45 (Aguilar-Barojas, 2005), considered the minimum clinically important value. Calculations considered a statistical power of 80%, a confidence level of 95% and potential patient losses of up to 20% (Hazra & Gogtay, 2016), resulting in the inclusion of a sample of 225 subjects. At the end of the study, 236 patients were recruited by convenience sampling. Severely ill patients, with cognitive impairment, unconscious, with delirium or who did not answer at least 80% of the psychological evaluation, were excluded from this study.
Measurements
The Hospital Anxiety and Depression Scale (HADS) was used to identify anxiety and depression symptoms in medical patients (Zigmond & Snaith, 1983). This scale comprises 14 items (seven for anxiety, seven for depression) with four Likert-type response options (ranging from zero to three). This research used a version of HADS adapted to the Mexican population with good reliability (Cronbach’s alpha = .86) resulting in a depression cut-off point of seven and an anxiety cut-off point of eight (López-Alvarenga et al., 2002).
This study used the Alcohol, Smoking and Substance Involvement Screening Test (ASSIST), designed to evaluate and identify the level of risk in the use of psychoactive substances such as alcohol, tobacco and illegal drugs (WHO ASSIST Working Group, 2002). It comprises eight questions identifying the types of use (lifetime use, current use, dependence problems and risk) of ten substances (alcohol, tobacco, cannabis, cocaine, amphetamine-type stimulants, inhalants, sedatives, hallucinogens, opioids, and other drugs). The scale considered the cultural aspects of the countries where it was evaluated and has been shown to have adequate levels of reliability in Spanish-speaking countries (Cronbach’s alpha = .93; Rubio Valldolid et al., 2014).
Section C of the International Neuropsychiatric Interview (MINI) was used to assess the presence of suicide risk. The MINI is a brief diagnostic interview developed to assess neuropsychiatric disorders based on the criteria of the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) and the International Classification of Diseases, 10th edition (ICD-10; Sheehan et al., 1998) Despite its extensive clinical use, its psychometric qualities have not been validated in the Mexican population. However, the following cut-off points are recommended for the interpretation of results: mild suicide risk (score 1-5), moderate suicide risk (score 6-9), high suicide risk (score over 10; Ferrando et al., 2000).
The sociodemographic data and length of stay were obtained from hospital records. Length of stay was taken as the number of hours from the patient’s admission to the emergency room to their discharge either because their health issue was resolved or because the patient was transferred to another department in the hospital. Although it was originally planned to obtain the number of hospital readmissions from hospital records, that information was unavailable. As a result, the number of hospital readmissions to the ED was obtained from the patient or their relatives self-reporting for the last year prior to the current stay.
Procedure
Patients hospitalized in the ED were invited to participate in the study. Due to the severity of the illness of the patients, only those who were conscious with adequate self-reported clinical conditions were assessed. Evaluations were performed by the psychology staff in the ED of the hospital where the research was conducted. Patients were informed of the research and signed an informed consent form. The scales were subsequently administered. Evaluation time ranged from 30 to 60 minutes. Finally, immediate psychological support was provided for patients in whom the presence of depression or anxiety symptoms, harmful substance use and/or suicide risk was identified.
Statistical analyses
The socio-demographic information obtained from patients was analyzed with descriptive statistics. Numerical variables were described by measuring the mode and standard deviation at 95%; categorical variables were described in terms of frequencies and percentages. For mental health and hospital stay variables, Kolmogorov-Smirnov normality tests were performed to determine the normality of the data distribution. In addition, Spearman-ordered rank correlations were performed to identify the association between these variables and length of stay, considering correlation coefficient intervals of ± .96 to ± 1.0 (perfect correlation), ± .85 to ± .95 (strong correlation), ± .70 to ± .84 (significant correlation), ± .50 to ± .69 (moderate correlation), ± .20 to ± .49 (weak correlation), ± .10 to ± .19 (very weak correlation) and ± .09 to ± .00 (null or nonexistent correlation), and a statistical significance level of p < .0527. Statistical analyses were performed using the R program version 4.0.1 with the psych, tidy verse, ggplot2 and lmtest packages (Hothorn et al., 2022; Revelle, 2020; Wickham, 2016; Wickham et al., 2019).
Ethical considerations
This research was approved by the Ethics and Research Committee of Hospital General Dr. Manuel Gea González (Registration number 27-152-2017).
RESULTS
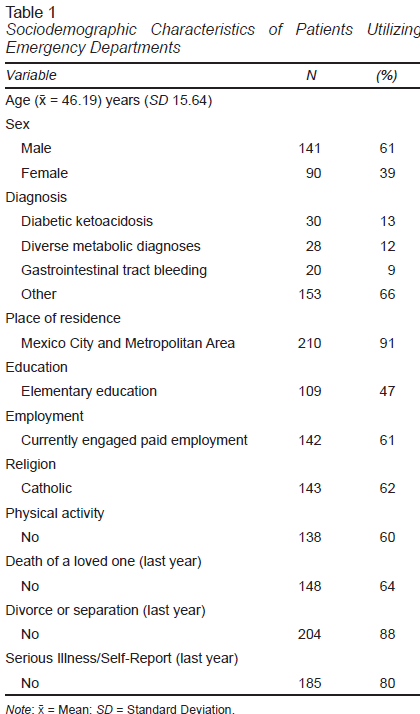
Of the 236 patients originally considered, five were omitted from the analysis because they failed to complete their evaluations, meaning that information was provided for 231 patients. Of these 231 patients, 61% (n = 141) were men, with an average age of 46 (standard deviation [SD] = 15 years). Seventy-two per cent of participants reported residing in Mexico City and the Metropolitan Area, 69% (n = 160) reported having completed high school, 61% (n = 143) reported professing Catholicism, and 59% (n = 138) of participants reported not being engaged in any type of work. In regard to substance use, 51% (119) reported frequent substance use, 21.6% of whom (n = 50) reported alcohol use and 16% of whom (n = 37) reported alcohol and tobacco use. Twenty-four percent (n = 56) reported taking medication to regulate their glucose levels, and 33.30% (n = 77) reported not having taken any medication prior to their hospitalization. In regard to mental health care, 26% (n = 60) reported having received psychological support or therapy at some point in their lives. Thirty-four per cent of patients reported having experienced the death of a family member, 10% had been separated or divorced from their partners, 18% received a new diagnosis of illness and 18.30% had experienced family fights during the previous year (Table 1).
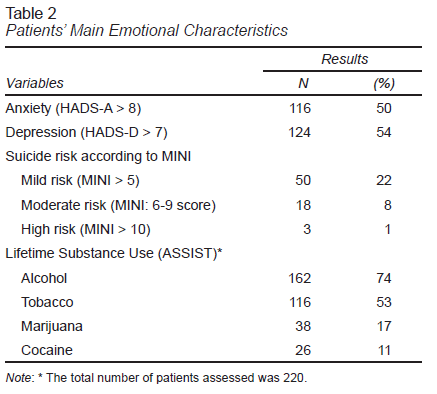
Data indicate that the average length of stay in an ED was 69.6 hours (SD = 65.68) and that the average number of readmissions was .4 (SD = .88). In regard to the emotional variables, it was found that 50% of the study population had anxiety symptoms (HADS-A > 8), 54% had depression symptoms (HADS-D > 7) while 1.3% had a moderate risk and 8% a high risk of suicide according to MINI. According to ASSIST, alcohol, tobacco, marijuana and cocaine were the most common substances used by patients in their lifetime. However, in the evaluation of substance use through ASSIST, the authors experienced problems administering the instrument, as a result of which no more data will be presented. This point will be taken up in the study limitations (Table 2).
In the correlation analysis, a very weak, statistically significant negative correlation was identified between length of stay and anxiety variables (rho = -.15, p = .02) and a very weak, statistically significant positive correlation was identified between length of stay and age (rho = .13, p = .05). No statistically significant correlation was established between the number of readmissions and other variables: suicide (rho = -.01, p = .87), age (rho = -.03, p = .07, anxiety (rho = .03, p = .72) and depression (rho = .09, p = .22). Regarding the suicide risk variable, a very weak but statistically significant negative correlation was identified with the age variable (rho = -.19, p < .001), and a weak, statistically significant positive correlation was identified with the depression (rho = .38, p < .001) and anxiety variables (rho = .44, p < .001).
DISCUSSION AND CONCLUSION
This study sought to evaluate the relationship between mental health, length of stay and the number of readmissions in patients hospitalized at a medical emergency department in Mexico City. From the data obtained, there does not appear to be any association between the mental health variables included and length of stay and number of hospital readmissions. Although a statistically significant association was found between anxiety and length of hospitalization, it was very weak. This finding differs from those reported in previous international studies, identifying an association between mood variables (Abar et al., 2017; Baia Medeiros et al., 2019; Blakemore et al., 2019) and psychiatric problems (Coates et al., 2019; Santillanes et al., 2020; Smith et al., 2016) and length of stay and number of readmissions to the ED.
Several factors could explain why the data differ from those reported in the international literature, such as the characteristics of the patients studied. As can be seen from the data on Mexican patients, the latter have a much greater length of stay than those reported worldwide. Some papers have found that on the first day of hospital admission, patients have higher levels of anxiety, which significantly increase after five days of hospitalization and decrease when the patient is discharged (Alzahrani, 2021). Most patients evaluated in the ED were admitted and discharged within 7.7 hours after hospitalization (Smith et al., 2016) whereas in this study, most patients were hospitalized for two to three days before being transferred to other medical specialties or being discharged from the ED.
Furthermore, several previous studies that have observed an association between the aforementioned variables have used retrospective, multicenter designs of large samples (ranging from 4,000 to over 100,000 patients; Baia Medeiros et al., 2019; Coates et al., 2019) from which information is retrieved by reviewing electronic records. Using electronic records to collect large samples from which to analyze variables would seem to be an effective strategy. However, to the authors’ knowledge, there is as yet insufficient coordination and infrastructure in Mexican ED that would enable access to such a large amount of information and data. In the future, it could be useful to create the necessary infrastructure to implement a national registration system. The importance of this research is that it is an incipient means of exploring the variables of interest.
Another explanation for the differences found may lie in the original reason why patients came to the ED. In most studies, patients were divided between those who went to the ED for mental health reasons (Holland et al., 2021; Theriault et al., 2020) and those with a health problem (Baia Medeiros et al., 2019). In our case, the hospitalized patients had both metabolic complications and mental health problems. It is highly likely that this condition is a particular characteristic of patients seen in EDs in developing countries and may be affecting waiting times and resolutions in EDs (Obermeyer et al., 2015; Polanco-González et al., 2013).
The length of stay observed in this study (an average of 69.6 hours) is striking, as it far exceeds the time suggested in international policy recommendations (four to eight hours; National Health Service, 2020) and Mexican policy (12 hours; Secretaría de Salud, 2013) to meet and resolve patients’ needs in medical emergencies. However, the average length of stay is similar to the average length of stay reported in developing countries, particularly in Latin America (ranging from 72 to 120 hours; Obermeyer et al., 2015). The conditions of emergency services in Mexico, as well as the nature of the emergencies attended (such as critical illnesses, armed conflict, and natural disasters), may well contribute to the long length of stay reported in this study and the region (Obermeyer et al., 2015; Polanco-González et al., 2013).
The number of readmissions observed in this study (.4) is significantly lower than what has been reported in other studies of patients with mood problems or psychiatric diagnoses, who use emergency departments up to twice as many times as those who do not suffer from mental health problems (Sims et al., 2021). Unfortunately, due to the way the hospital keeps its medical records, it proved impossible to obtain objective information on the number of readmissions of each patient, a common problem in EDs (Kaji et al., 2014). Although self-reporting by the patient was the most practical means of obtaining information, since there is a significant risk that this information may be inaccurate, results should be interpreted with caution. Finally, based on clinical experience, it was observed that several of these patients were in fact readmitted to an ED at a different hospital, and were therefore not recorded as readmissions in this study. Readmissions in this study are therefore likely to have been under-reported.
It is important to note that the percentages of anxiety (50%) and depression (54%) symptoms obtained are similar to those reported in a retrospective study (anxiety = 42%; depression = 46%) evaluating and reviewing the records of patients admitted to the same hospital (Murillo et al., 2022). These data are similar to those described in other international studies and the Latin American context, where a range of anxiety oscillating between 30% and 40% of the patients evaluated has been observed (Castilla-Puentes et al., 2008; Webster et al., 2014). In regard to depression, figures obtained in this study are higher than those reported in the international literature and in the Latin American context, where the prevalence of depression is approximately 30% (Castilla-Puentes et al., 2008). In both cases, the increase in the frequency of presentation could be attributed to the time that has elapsed since the publication of earlier studies and the fact that in recent years, an increase of up to 26% has been reported in cases of people with depression seeking care in emergency services (Ballou et al., 2019).
A total of 8.3% of the population showed a moderate to high suicide risk according to the MINI instrument. These data are very similar to those reported in evaluations previously described in emergency medical patients in the United States (approximately 5-8%) (Boudreaux et al., 2016; Ilgen et al., 2009; Miller et al., 2017). This underscores the high number of emergency patients who display suicidal ideation or behavior when hospitalized. Recent studies have therefore pointed to the importance of screening to determine suicide risk in emergency medical patients and to implement actions to address this situation (Boudreaux et al., 2016; Ilgen et al., 2009).
A major problem of this study was the impossibility of obtaining data on substance use measured by the ASSIST instrument. The problem was due to the inadequate administration of the instrument by the evaluation team, resulting in incomplete information on items six and seven of the instrument (leading to losses of over 30%). Although this inadequate administration constitutes a major barrier to obtaining information, the authors of this paper believe it is only ethical to point out the failure, thereby promoting transparency in the information presented and perhaps encouraging greater replicability of psychological research (Open Science Collaboration, 2015).
Likewise, it is important to share the lessons learned to attempt to avoid making the same mistakes in the future. In this regard, the team of researchers identified 1) the need to design or use specialized training programs for evaluators (currently, and due to the COVID-19 pandemic, a large number of online courses have been offered, which could help achieve these goals); 2) the need to constantly supervise the evaluators’ procedure in order to detect any deviation from the process to be followed in a timely fashion (the use of work diaries has been recommended for this purpose); and 3) the importance of regularly recording data to identify any anomalies that may arise with the data (Antes & Maggi, 2021).
Finally, since this is a cross-sectional study, the data show what the participants were like at the time of evaluation, yet fail to provide complementary information on the evolution of symptoms (Wang & Cheng, 2020). Similarly, a social desirability bias could be present. Previous research with relatives of hospitalized patients in Mexico has shown that Mexican cultural beliefs encourage people to maintain a positive view of daily problems that arise, which could lead patients to minimize the expression of their mental health symptoms to health personnel even though the latter could affect their perception of their hospital stay (Toledano-Toledano & Domínguez-Guedea, 2019).
Despite the limitations described above, in the authors’ view, this study presents valuable, novel data. This is the first study in Mexico to assess the association between mental health variables and hospital stays/utilization. From the data presented it is possible to identify a high presence of mental health problems in patients hospitalized in medical emergencies. The data could undoubtedly support the replication of evaluations and interventions at other hospitals. Likewise, the data show the number of hours required to attend patients in emergency departments. This number is far higher than the international and national recommendations for attending patients. It would also be worthwhile to replicate these data at other facilities to identify the source of this delay.
Finally, the authors conclude that there is little or no relationship between the mental health, length of stay and number of readmissions of patients hospitalized in an emergency department. Further studies are recommended to corroborate the data presented.