INTRODUCTION
Sleep plays a crucial role in maintaining health and well-being in a variety of ways. Chronic sleep deprivation has been associated with an increased risk of developing cardiovascular diseases (Guasch-Ferré et al., 2022), obesity (Hur et al., 2021), Type 2 diabetes mellitus (Mostafa et al., 2022), metabolic syndrome (Smiley et al., 2019), and a weakened immune response (Prather et al., 2021). Sleep deprivation has also been associated with a higher incidence of depressive and anxiety disorders (Chen et al., 2017; Chunnan et al., 2022), exacerbation of suicidal behavior (Wang et al., 2019), substance abuse, and psychotic disorders (Hertenstein et al., 2019).
Since sleep patterns can be modified using health interventions, they constitute a modifiable risk factor for various conditions (Kyle & Henry, 2017). They provide an opportunity for health damage prevention and improving the quality of life and functioning of individuals. To understand the development of changes in sleep quality, it is crucial to realize that it is shaped by the complex interaction of various factors. This will make it possible to identify targets for therapeutic strategies, enabling the enhancement and individualization of treatment (Grandner & Fernandez, 2021).
Personality is a promising determinant of modifying sleep quality because its relatively stable nature can enhance understanding of the development of health conditions across the lifespan (Kern & Friedman, 2017). The Five Factor Model (FFM) categorizes personality traits into five measurable domains: neuroticism, conscientiousness, extraversion, agreeableness, and openness to experience (John, 2021). Certain features of this model make it suitable for the context of health psychology. The clear division into independent and measurable domains is useful since it permits direct correlations with specific outcomes. Moreover, its well-established cross-cultural validity enables the comparison of results across different world regions (Kern & Friedman, 2017).
According to FFM, neuroticism is associated with greater vulnerability to stress and an increased likelihood of experiencing negative emotions such as sadness, fear, and anger. Conversely, conscientiousness is associated with a predilection for self-discipline, organization, diligence, and goal-orientation. Extraversion describes individuals who lean towards sociability, are active, and often experience positive emotions. Agreeableness is characterized by a tendency to be cooperative, empathetic, trustworthy, and altruistic. Lastly, openness to experience denotes an inclination towards creativity, imagination, and embracing new experiences (John, 2021).
Evaluations of the personality traits of the Five-Factor Model (FFM) and their potential correlations with sleep have found that neuroticism consistently demonstrates a negative correlation with sleep quality, which is more pronounced than that of other personality traits. On the other hand, the traits of conscientiousness and extraversion were associated with better sleep quality in most studies. However, the traits of agreeableness and openness to experience showed inconsistent results (Souza, 2023).
It is crucial, however, to assess personality traits together with the determinants of sleep quality because they may have unique relationships with personality and enhance our understanding of the association between personality and sleep (Costa et al., 2019; Sutin et al., 2011; Weisberg et al., 2011; Williams et al., 2021). Since multivariate analyses can compare the predictive power of each variable, they were used to determine the extent to which each variable contributes to sleep quality.
The present study primarily aimed to explore the relationship between personality traits and sleep quality. It therefore sought to describe the sample profile in terms of sleep quality, personality profile based on the FFM model, sociodemographic and clinical data, and test a multiple regression model designed to predict sleep quality based on these variables.
METHOD
Participants
The questionnaire was answered by 489 participants from the general population, aged eighteen and over, regardless of gender and residing in any region of Brazil. Convenience sampling was used to recruit participants. An online survey was disseminated through social media (such as Instagram, email, and WhatsApp), targeting those in this age bracket. The invitation specified that the study involved a questionnaire on sleep quality, explaining that participation would be voluntary. The informed consent form (ICF) was provided in the first section of the online survey, requiring participants to provide their consent before accessing the main questionnaire. The self-administered questionnaire showed an average response time of approximately fourteen minutes.
A total of 489 individuals answered the online survey. However, fourteen participants were excluded due to the incorrect completion of the questionnaires, nineteen were excluded for being sixty-five years or older, four for being under 18, and one for frequently appearing as an outlier, indicating incorrect completion. Furthermore, four participants who identified as transgender or another gender were excluded because the small sample size would make statistical analysis unfeasible. The final data analysis therefore included 447 participants. Answer spaces left blank for weight and height items were completed with average values.
Measurements
Sociodemographic Questionnaire: This was prepared by the research team to identify the characteristics of the study sample. It included age (in years), gender (male, female, or other), educational attainment (complete or incomplete primary, secondary, or tertiary education), employment status, family income (in minimum wages), and previous medical and psychiatric history.
Brazilian Portuguese version of the Pittsburgh Sleep Quality Index (PSQI-BR): This instrument comprises ten items assessing sleep quality across seven components: subjective quality, latency, duration, habitual efficiency, sleep disturbances, use of sleep medication, and daytime dysfunction. The sum of the seven components yields a global score ranging from 0 to 21. The cutoff point of five can be used to distinguish “good sleepers” from “poor sleepers.” The index has been used across various populations, including those with clinical illnesses, and can be used to assess sleep impairment regardless of the underlying cause. In the Brazilian validation study, it demonstrated a high degree of internal consistency with a Cronbach’s alpha of .82 (Bertolazi et al., 2011; Buysse et al., 1989).
Patient Health Questionnaire (PHQ-4): This is an ultra-brief tool comprising four items useful for screening depressive and anxiety symptoms. It contains two subscales: the first two assessing depressive symptoms and the last two evaluating anxiety symptoms, yielding two scores ranging from zero to six. Scores above three on each scale indicate the presence of depression or anxiety symptoms (Kroenke et al., 2009). A Brazilian study identified a Cronbach’s alpha of .77 and .79 for depression and anxiety, respectively (Silva & Faro, 2021).
Big Five Inventory (BFI): This comprises forty-four items, with four items for each personality factor. Each item is rated from one to five based on agreement or disagreement with propositions about self-perception. Each factor receives an independent score calculated from the arithmetic mean of the scores of the four items assessing them. In a Brazilian sample, internal consistency, as indicated by Cronbach’s alpha, was .72, .69, .56, .69, and .69 for extraversion, agreeableness, conscientiousness, neuroticism, and openness to experience, respectively (Gouveia et al., 2021).
Statistical analysis
The data analysis was conducted using JAMOVI 2.3. Initially, descriptive-exploratory statistical analyses were performed to determine sample characteristics and verify normality assumptions for the variables included in the study. Outlier values in personality trait measurements were filled with the mean value plus or minus one standard deviation, depending on their original trend: conscientiousness, three cases; extraversion, two cases; agreeableness, six cases; and openness to experience, three cases. Student’s t-tests or Mann-Whitney U tests were performed to explore the association between sleep quality and binary variables, while correlation tests were used to assess the association between sleep quality and continuous variables. Statistical significance was set at p value < .05. Based on the correlation test results, variables were selected for inclusion in the multiple linear regression model (using the “Enter” method), in which the overall PSQI-BR score was used as the dependent variable.
Ethical considerations
The Human Research Ethics Committee of the Federal University of Sergipe (CAAE: Tag: 59193422.8.0000.5546) approved the project associated with this study. The online ICF was placed in the initial section of the online survey, requiring participants to provide their agreement before accessing the actual questionnaire. The ICF informed participants of their rights when participating in the study and provided a brief explanation of the topic of the study and its overall objective. Since the survey was intended for adults, participants who indicated that they were under eighteen were excluded from the data analysis.
RESULTS
The majority of the sample were female (74.5%, 333). The average age was 37.7 years (SD = 13.0), with 86.1% (385) having completed or partially completed higher education and 13.9% (62) having completed or partially completed secondary or primary education. The family income of 37.6% (168) of the participants was less than or equal to three minimum wages. The average score for the PSQI-BR was 7.84 (SD = 3.89). According to the established cut-off point of ≥ 6, it was found that 69.4% (310) of participants had poor sleep.
The PHQ-4 results showed that 34.2% (153) of participants displayed depression symptoms and 42.1% (188) anxiety symptoms. Combining the results of the two subscales revealed that 52.6% (235) showed no symptoms, 13.2% (59) only anxiety symptoms, 5.4% (24) only depression symptoms, while 28.9% (129) displayed both symptoms. Women showed more anxiety (X2[1] = 13.3, p < .001) and depression (X2[1] = 67.8, p < .001) symptoms.
Associations with higher PSQI-BR scores were found in the following variables: older age (r[445] = .176, p < .001), higher BMI (r[445] = .161, p < .001), female gender (U[445] = 16109, p = .009), primary or secondary educational attainment (t[445] = 6.18, p < .001), family income of less than three minimum wages (t[445] = 5.71, p < .001), presence of depression symptoms (t[445] = -10.4, p < .001), and presence of anxiety symptoms (U[445] = 10095, p < .001).
The presence of anxiety and depressive symptoms was associated with high neuroticism (t[44] = -12.861, p < .001 and t[445] = -11.309, p < .001) and low conscientiousness (t[445] = 3.352, p < .001 and t[445] = 3.980, p < .001), extraversion (U[445] = 19516, p < .001 and t[445] = 5.334, p < .001), and agreeableness (t[445] = 4.136, p < .001 and t[445] = 5.739, p < .001).
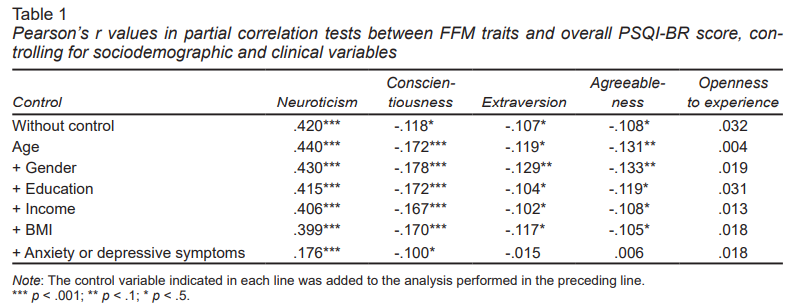
Sleep quality was correlated with low neuroticism (r[445] = .420, p < .001) and high conscientiousness (r[445] = -.181, p = .012), extraversion (r[445] = -.107, p = .024), and agreeableness (r[445] = -.108, p = .022), but showed no correlation with openness to experience (r[445] = .032, p = .500). Table 1 displays the results of partial correlation tests between PSQI-BR and personality traits, controlling for sociodemographic and clinical variables.
To test the multiple regression model, the “depression symptoms” and “anxiety symptoms” variables were reformulated into a trichotomous variable. The variable was encoded in the regression model as a dummy comprising the following items: absence of depression or anxiety symptoms, presence of only depression or anxiety symptoms, and concurrent presence of depression and anxiety symptoms. This choice was made due to the strong association between the presence of anxiety and depression symptoms (X2[1] = 170, p < .001, Cramer’s V = .617), which could result in multicollinearity.
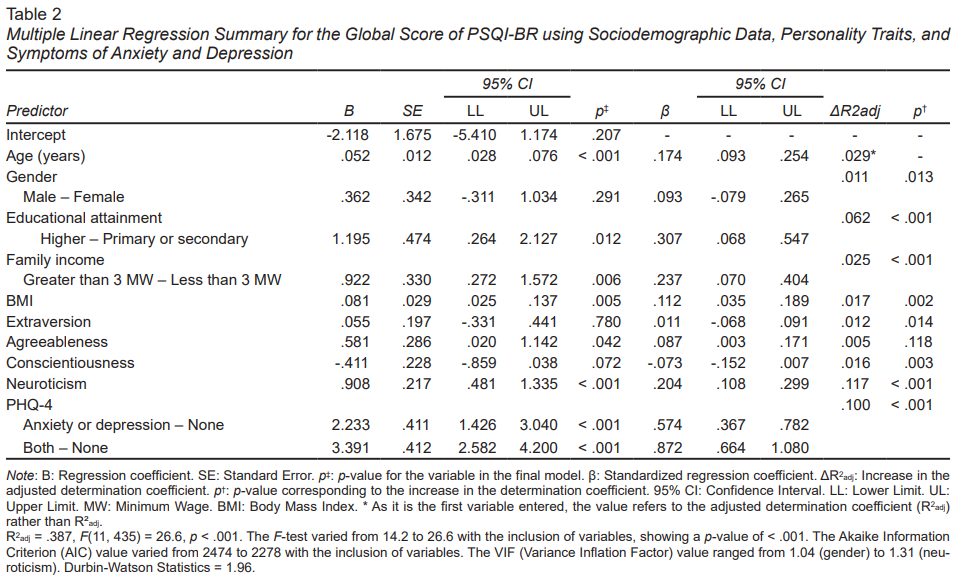
The final regression model showed a satisfactory fit, with an adjusted coefficient of determination (R2adj) of .387, indicating that it could explain 38.7% of the PSQI-BR score variance. Despite showing statistically significant associations at the bivariate level, the gender, conscientiousness, and extraversion variables were not found to predict sleep quality in the multiple linear regression model (Table 2).
The variables found to be significant in predicting sleep quality were age (β = .174, p < .001), educational attainment (β = .307, p = .012), family income (β = .237, p = .006), BMI (β = .112, p = .005), neuroticism (β = .204, p < .001), agreeableness (β = .087, p = .042), and presence of psychopathological symptoms (anxiety or depression symptoms [β = .574, p < .001] and both symptomologies [β = .872, p < .001]). In terms of individually explained variance, the most significant variables, in descending order, were neuroticism (ΔR2adj = .117, p < .001), psychopathological symptoms (ΔR2adj = .100, p < .001), educational attainment (ΔR2adj = .062, p < .001), age (ΔR2adj = .029), family income (ΔR2adj = .025, p < .001), and BMI (ΔR2adj = .017, p = .002).
DISCUSSION AND CONCLUSION
The global scores for the PSQI-BR in the present study were higher than those of similar studies worldwide. The average score was 7.84 (SD = 3.89), compared to 4.76 (SD = 2.92) in Italy (Cellini al., 2017), and 6.93 (SD = 4.31) in the USA (Gamaldo et al., 2020). This outcome was expected, given that Brazil has one of the highest global prevalence rates of insomnia (Morin & Jarrin, 2022). In a bivariate analysis, the PSQI-BR score was associated with higher neuroticism and lower conscientiousness, extraversion, and agreeableness. This finding aligns with the results of previous studies (Souza, 2023). The present study therefore contributes to advancing the understanding of this association by proposing a multivariate analysis, considering other determinants of sleep quality, as discussed below.
Neuroticism demonstrated predictive power for sleep quality (β = .204, p < .001), displaying the most significant increase in explanatory capacity in the regression model (ΔR2aj = .117, p < .001). This finding underscores the significance of this trait over others, encouraging more in-depth research. In the existing literature, various mechanisms have been proposed to explain the link between neuroticism and the deterioration of sleep quality. These include increased stress sensitivity and vulnerability to anxiety and depressive disorders that may present with sleep-related symptoms (Lai, 2018; Gamaldo et al., 2020), the presence of unhealthy sleep habits (Sella et al., 2020), heightened cognitive activation and the inability to control one’s thoughts (Cellini et al., 2017), together with an inflated assessment of sleep impairment (Sutin et al., 2020). The association between neuroticism and sleep could explain the positive outcomes achieved through mindfulness-based therapies for insomnia symptoms (Perini et al., 2023). This is because individuals with high neuroticism exhibit greater stress reactivity and benefit more from emotional regulation strategies (Carver & Connor-Smith, 2010).
Despite correlating with sleep quality at a bivariate level, conscientiousness and extraversion traits failed to show predictive capacity in the regression model tested (β = -.073, p = .072 and β = .011, p = .780, respectively). Nevertheless, it was observed that the conscientiousness trait maintained a statistically significant correlation with sleep quality, even when all other non-personality trait variables had been controlled for. This suggests that the loss of this trait in the regression model was linked to its association with other personality traits. The tendency toward impulsivity is a prime example of behavior that intersects with traits from the FFM. Impulsivity has a strong inverse correlation with the “self-control” facet of conscientiousness, but can also stem from novelty-seeking in highly extroverted individuals or manifest as neuroticism when stemming from emotional instability (Jackson & Roberts, 2017). The main mechanism proposed to explain the relationship between conscientiousness and sleep is the adoption of healthy habits. Individuals with higher conscientiousness are more likely to engage in regular physical exercise and follow a healthy diet, thereby reducing the risk of obesity and other conditions that can negatively impact sleep (Duggan et al., 2014; Rochefort et al., 2019). At the same time, possible explanations for the association between extraversion and sleep include increased physical activity (Gamaldo et al., 2020) and reduced stress sensitivity (Lai, 2018).
The trait of agreeableness showed predictive power for poor sleep quality in the regression model (β = .087,
p = .042), contrary to what was found in the bivariate analysis (r[445] = -.108, p = .022). However, when added to the model, it did not significantly increase explained variance (ΔR2aj = .005, p = .118). Furthermore, this trait showed no correlation with sleep quality when controlling for the same variables in the model, excluding other personality traits. These findings suggest that most of the information provided by the agreeableness trait may be redundant or already explained by other traits, thereby only minimally contributing to predicting sleep quality.
Another crucial point to consider is the weakening strength of the correlations between all four personality traits and sleep quality when the effects of anxiety and depressive symptoms are controlled for. This result suggests that a significant portion of the predictive power of personality traits for sleep quality stems from their exposure to or protection against the development of psychopathological symptoms. Both depression and anxiety disorders follow a pattern in relation to the personality traits of the FFM: high neuroticism and low conscientiousness and extraversion (Kotov et al., 2010). Findings on agreeableness show contradictions across studies, while openness to experience typically has no correlation with the incidence of mental disorders (Bagby et al., 2017).
Age was a predictive variable for sleep quality in the regression model tested (β = .174, p < .001). As age increases, sleep tends to deteriorate in regard to both quality and quantity. Changes can manifest as difficulty falling and remaining sleep, a reduction in total sleep duration, changes in sleep patterns, and alterations in sleep architecture. Although these changes are more intense among older adults, they may be observed during adulthood (Chaput et al., 2018). Furthermore, personality traits can change as a person ages. In the present study, the association between conscientiousness and sleep quality strengthened when age was controlled for as a variable. This can be explained by the normative pattern of modification of this trait, characterized by its increase over time (Costa et al., 2019).
BMI was a predictor of sleep quality in the regression model (β = .112, p = .005). Sleep disruption has been associated with the disruption of satiety-related hormones, resulting in increased food intake. Furthermore, increased fatigue, decreased physical activity, and increased opportunities to eat can contribute to the exacerbation of obesity (St-Onge et al., 2011). Conversely, a higher BMI has been associated with the worsening of Obstructive Sleep Apnea Syndrome (OSAS) (Bacaro et al., 2020). BMI therefore has a complex, bidirectional relationship with sleep, as observed in the regression model. However, contrary to expectations, this variable showed no correlation with conscientiousness and did not alter the association between this trait and sleep (Jia et al., 2022).
Educational attainment (β = .307, p = .012) and family income (β = .237, p = .006) were also significant predictors of sleep quality. The literature indicates that socioeconomic variables such as educational attainment, parents’ educational attainment, annual family income, perception of financial well-being, type of employment, and employment status can influence sleep patterns, thereby supporting the findings of the present study (Philippens et al., 2022; Sosso et al., 2021).
The main limitations of this study are associated with its non-probabilistic sampling. Most participants, for instance, have either completed or partially completed higher education (86.1%), a figure that contrasts with the 23.3% reported by the Brazilian Institute of Geography and Statistics (IBGE, 2022) for the total Brazilian population. This may have occurred due to the fact that the survey was disseminated on social media restricted to the university environment. Another example is the predominance of females in the sample. This demographic skew could potentially introduce a bias into average PSQI scores, suggesting that results should be interpreted with caution, although the higher incidence of insomnia among women has been well-documented (Zeng et al., 2020). Nonetheless, a similar pattern can be observed in previous studies (Souza, 2023), suggesting that this should not restrict the comparison of the findings of this study with those of others. Due to methodological and statistical limitations, this study did not consider other sleep-related determinants such as sleep habits, type of occupation, geographical and climatic factors, and family history of sleep alterations. Another potential limitation is the lack of objective sleep measures such as actigraphy or polysomnography. Comparing objectively and subjectively measured sleep can provide insights into the role of individual sleep assessment, which is of interest when evaluating personality (Catherman et al., 2023).
Despite these limitations, the present study contributes to the understanding of the association between personality traits and other variables in predicting sleep quality. In short, the importance of neuroticism in predicting sleep quality is emphasized over other personality traits in the FFM. Beyond personality-related aspects, neuroticism has shown significant importance when compared to other determinants of sleep quality, prompting further investigations into its role in sleep and overall health. Future research on this topic could also use objective sleep measurements and opt for a longitudinal design, allowing for an understanding of the role of personality over time in its association with sleep and other variables. Understanding and improving sleep care is an opportunity for health psychology, with potential implications for various aspects of health and well-being.