INTRODUCTION
The COVID-19 pandemic was particularly alarming because of its unknown means of transmission, rapid development of symptoms that were refractory to available treatment and severe negative outcomes. The immediate effect of COVID-19 was a major impact on mortality, but it also produced family losses, financial difficulties and social dysfunction. Borders were closed and residents were kept under lockdown with no immediate hope of returning to their everyday activities. Previous epidemics had been much shorter and more local, and the academic community knew little of the mental health consequences of this type of worldwide epidemic. Mental health consequences of the pandemic among the population and those treating COVID-19 cases that had tended to be overlooked came to the forefront of discussions, sometimes with pessimistic predictions (Santomauro et al., 2021).
There was an urgent need for information and guidance. In this era of the internet, quick, inexpensive options for obtaining information gained momentum. Typical mental health studies during the initial phases of the pandemic were cross-sectional surveys with self-reported information on mental health symptoms usually but not always validated by screening instruments and scales. These studies were implemented on websites, and sometimes by phone, on self-selected volunteers. As noted, non-probability and convenience samples without response rates and no background information on the population from which the sample had been drawn was then sometimes used to report prevalence rates of the mental health consequences of COVID-19 (Pierce et al., 2020). In a subsequent methodological improvement, cross-sectional surveys of delimited populations calculating non-response rates by basic age/sex groups using standard mental health instruments began to emerge as the epidemic progressed (Ma et al., 2021). Nevertheless, these surveys sometimes lacked estimates of previous mental health issues in the same populations to compare with those taken during COVID-19 (Kunzler et al., 2021). Cross-sectional surveys and accurate longitudinal cohort studies were subsequently instrumented and reported in the international literature (Prati & Mancini, 2021; WHO, 2022; Witteveen et al. 2023). More recently, meta-analyses of longitudinal studies on the mental health consequences of COVID-19 became available with summaries of up to date knowledge on the issue (Ahmed et al., 2023; Witteveen et al., 2023). In general, these meta-analyses of longitudinal cohort studies and large-scale international time-trend studies tended to report much more moderated mental health consequences of the COVID-19 pandemic. A recent meta-analysis of longitudinal studies even reported that anxiety and depression symptoms may have decreased from baseline to follow-up, while other mental health problems showed no change (Cénat et al., 2022).
The COVID-19 pandemic had an immediate impact on Mexico, with over 334,000 deaths and 7,633,355 cases by the end of August 2023 (Worldometer, 2023). As the country recovers and returns to normality, the health sector is attempting to draw lessons from this costly experience to prepare for the future. To what extent was the mental health of the Mexican population affected by COVID-19? What were the main studies and findings? International meta-analyses of both longitudinal and repeated cross-sectional studies do not include any Mexican studies (Ahmed et al., 2023; Witteveen et al., 2023). A meta-analysis of low- and middle-income countries reported six studies in Mexico, with no identifying data on either the studies or their results (Chen et al., 2022). Regardless of the lack of local studies, some international research (GBD, 2021) reported a 42.2% increase in depression and a 39.8% increase in anxiety during the COVID-19 epidemic in Mexico. We have only found one systematic review of Mexican studies, based on large-scale international scientific databases (Hernández-Díaz et al., 2022) including approximately fifteen studies up to December 2021. Updated information is therefore required. Objective: We extended the timeframe of the literature search to February 2023, used a longer list of potential mental health outcomes and more local databases, such as SciELO, and Biblioteca Virtual en Salud (BVS). We analyzed ninety-five studies including data on symptoms of depression, anxiety, suicidal thoughts and behaviours, alcohol use, gaming, and sleep problems in Mexico. We focused on the methodology of these studies, their prevalence estimates and suspected risk factors.
METHOD
Eligibility criteria
We included all the original quantitative research on the Mexican population ages twelve and older, published in English and Spanish from 2020 to 2023. Studies were included regardless of their study design, but were excluded if they were qualitative or narrative (case studies, essays, editorial letters, or commentaries on published papers). When data from the same sample were reported in two or more studies, we included those with the most comprehensive information.
Information sources and search strategy
Searches were conducted in February 2023 (the last one being performed on February 13) in the following electronic databases: PubMed, Embase, PsycINFO, Web of Science, Scopus, SciELO, and the Biblioteca Virtual en Salud (BVS). We searched for keywords and MeSH terms related to mental health and COVID-19, including depression, anxiety, alcohol, drugs, sleep problems, eating disorders, suicide, gaming, COVID-19, and SARS-CoV-2. By way of an example, our PubMed search algorithm was entered as: (“Mexico”[Mesh]) AND (“COVID-19”[Mesh] OR “SARS-CoV-2”[Mesh]) AND (“Anxiety Disorders”[Mesh] OR “Mental Health”[Mesh] OR “Ethanol”[Mesh] OR “Alcoholism”[Mesh] OR “Internet Addiction Disorder”[Mesh] OR “Behavior, Addictive”[Mesh] OR “Illicit Drugs”[Mesh] OR “Psychotropic Drugs”[Mesh] OR “Synthetic Drugs”[Mesh] OR “Cannabis”[Mesh] OR “Marijuana Use”[Mesh] OR “Suicide”[Mesh] OR “Suicide, Attempted”[Mesh] OR “Suicide Prevention”[Mesh] OR “Suicide, Completed”[Mesh] OR “Suicidal Ideation”[Mesh] OR “Self-Injurious Behavior”[Mesh] OR “Anxiety”[Mesh] OR “Anxiety Disorders”[Mesh] OR “Depression”[Mesh] OR “Depressive Disorder”[Mesh] OR “Sleep”[Mesh] OR “Feeding and Eating Disorders”[Mesh]). The full lists of search terms for each database are available as supporting information (Appendix A1). Bibliographic references listed in previous systematic reviews were screened for literature not included in the main searches, and we also searched the reference sections of the manuscripts included.
Records were retrieved in RIS format for each database and deduplicated in EndNote, used for the systematic removal of duplicate records in seven stages, based on a series of combinations for author, year, title, pages, and volume (Bramer et al., 2016).
Selection process
One author (BS) screened the deduplicated results for eligibility, based on their titles and abstracts, and the full texts of all potentially eligible studies were examined for inclusion. In the event of doubt, the final decision was made in conjunction with the senior author (GB). Each selected manuscript was classified by at least one of six mental outcomes.
Data items
For each manuscript, the following data were identified by all the authors and extracted and captured on an ad hoc spreadsheet by one author (BS), and subsequently reviewed by another (RO):
-
Author and publication year
-
Research scope. We classified studies as international (distinguishing between those that disaggregated Mexican data from those that only reported pooled data), national (if a population of two or more Mexican states were included in the study) or local (at the state, municipal, or city level)
-
Sample size. Number of people included in the study. Whenever an international study disaggregated data by country, we recorded the sample size for the Mexican sample alone
-
Target population. The type of population intended to be studied (such as adults, college students and healthcare workers)
-
Sampling method. If a sample was selected based on the intended census of the target population, if there was a sampling frame or any kind of random sampling was used, or if it was a convenience sample (usually based on an open invitation through social media), when no further information on the sampling method was provided, we classified it as unclear. We included the response rate whenever it was reported
-
Type of data collection. Online or telephone survey, face-to-face, or any other type
-
Sample characteristics. We extracted the proportion of males (females, or any other population) in the sample, as well as their mean age in years
-
Research design. We distinguished between cross-sectional (including surveys with only one measurement or panel studies with more than one), longitudinal, and any other kind of studies
-
Assessment tool. We extracted the psychometric scale, subscale, or question used to assess the main outcome of the study
-
Prevalence of the mental health indicator assessed. We included the prevalence (specifying its time frame, such as “in the past two weeks”) of the main mental health measure. If reported, we included prevalence by severity levels and/or sex
-
Main results. We extracted the main results for each outcome in terms of its association with the mental health of the Mexican population and other mental health variables.
Any issues regarding data extraction were resolved by consensus among all the authors.
Summary measures
Since this was a systematic review with no meta-analysis, we did not report any pooled measures.
Synthesis of results
Each manuscript was classified into one or more of the following six mental health outcomes: alcohol use, anxiety, depression, gaming, sleep disorders, and suicide. We performed a qualitative synthesis of results for each of these issues, as we decided not to pool results using meta-analysis techniques due to the high degree of heterogeneity in the instruments used in each study, the populations under study, and the representativeness of the samples.
RESULTS
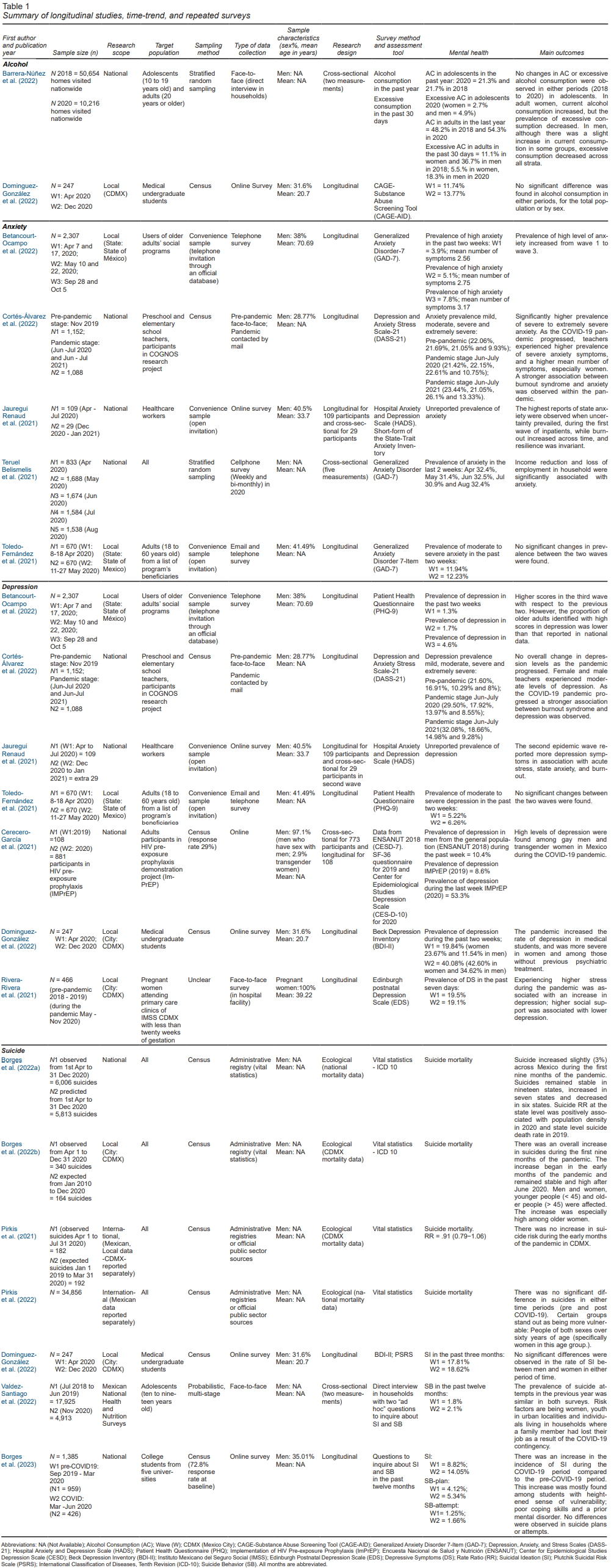
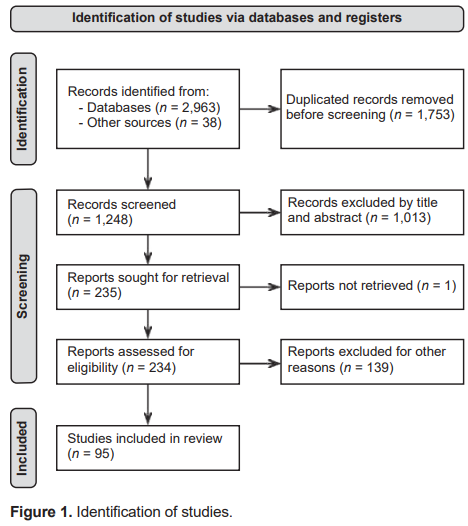
Our search by using common bibliographical databases yielded an initial 2,963 candidates, in addition to thirty-eight references located manually by the three authors. At the end of the process, we identified ninety-five references that included data for Mexico or, in a small number of reports, included Mexico as part of international surveys that only provided overall results. Six studies were published in 2020, thirty-seven in 2021, forty-six in 2022 and six by February 2023. Appendix A2 contains a list of these publications. In Table 1, we present a summary of studies using longitudinal, time-trend or repeated surveys for our six outcomes. In Annex A3-A8, we present detailed information with all studies for each outcome (Figure 1).
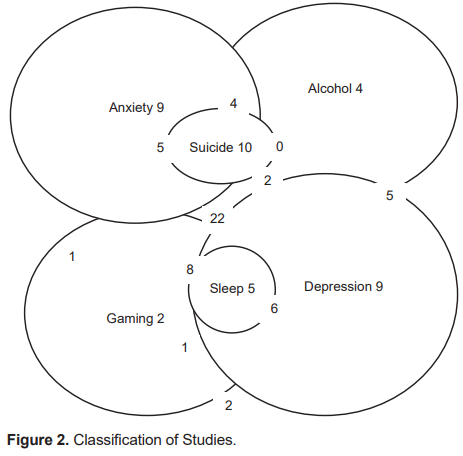
We classified these ninety-five papers on mental health issues and COVID-19 exploring the following issues: anxiety (n = 57), depression (n = 58), suicide (n = 19), sleep problems (n = 15), alcohol (n = 12), and gaming (n = 5).Of these papers, some examined a single issues: anxiety (n = 9), depression (n = 9), suicide (n = 10), sleep problems (n = 5), alcohol (n = 4), or gaming (n = 2). Most papers reported more than one issue, with anxiety and depression being the most common combination (n = 32), while thirteen reported three to four combinations (anxiety, depression, and suicide were reported in four publications, while one paper reported anxiety, depression, suicide, and sleep problems) (Figure 2).
Alcohol use
We found twelve studies dealing with alcohol use during the pandemic, with only one also including information on drugs among elderly Facebook users (Pinelo Camacho et al., 2022). Several studies used standard instruments such as the Alcohol, Smoking and Substance Involvement Screening Test (ASSIST), Alcohol Use Disorders Identification Test (AUDIT-C), and CAGE-Substance Abuse Screening Tool (CAGE-AID). Most studies used cross-sectional stand-alone one-time surveys among self-selected populations recruited by website advertising. Some of these surveys included questions on alcohol consumption during the pre-pandemic period that was used as a comparison with current alcohol use.
Two studies have distinctive methodology: a repeated survey of two large-scale national health and nutrition surveys (Encuesta Nacional de Salud y Nutrición, Spanish acronym Ensanut), one in 2018 and another in 2020.
(Barrera-Núñez et al., 2022), N 2018 = 50,654 and N 2020 = 10,216 is an exception in methodological terms. According to this report, “Alcohol consumption in women increased from 33.5% in 2018 to 42.5% in 2020. During the same period, the prevalence of excessive alcohol consumption decreased from 11.1% to 5.5% in women and from 36.7% to 18.3% in men,” with no changes in alcohol consumption or excessive alcohol consumption being observed between the two periods (2018 to 2020) in adolescents. There was no report of response rates in either of the two surveys.
We found one longitudinal study (Domínguez-González et al., 2022) for a small group of 247 self-selected, undergraduate medical students. According to the authors “The prevalence of risky alcohol consumption was 11.74% in April and 13.77% in December (χ2 = .500).”
The conclusion of both these surveys, regarding the insignificant or null impact of the pandemic on heavy alcohol uses, contrasts with certain reports using one-time surveys among self-selected participants. For example, a small national survey of 866 participants, (Ibarrola-Peña et al., 2022) concluded that, “Participants used alcohol as a substance of choice to minimize the psychological effects of the COVID-19 pandemic. Substance use patterns were affected by the pandemic, with an increase in the number of users and consumption rate…”. Other authors, using studies with a similarly limited methodology (Villaseñor-López et al., 2021) concluded, on the other hand, that “During the COVID-19 lockdown, the majority of the population indicated that they had not increased or decreased their consumption of alcoholic beverages.”
The only survey including drugs (Pinelo Camacho et al., 2022) reported that in the previous thirty days, non-prescription tranquilizers had been used by 16.05% and marijuana by 7.89% of participants. Use of other illegal drugs did not exceed 2.6% of the population. No data is reported for the pre-COVID-19 period for the elderly population.
Anxiety
A total of fifty-seven reports in Mexico, explored anxiety symptoms during the pandemic. The modal study here is a one-time, cross-sectional survey of anxiety symptoms performed of a group of self-selected volunteers contacted through a website. This can be done locally, nationally or internationally. No study reported any response rates, and only rarely were self-selected samples reported as a possible limitation in the conclusions. Most of these reports used standard instruments for detecting anxiety symptoms. We identified fourteen different instruments used for anxiety (see Table A4 Anxiety, notes). Those instruments are not directly comparable, and some authors used the same instruments but with different cut-off points while others reported means of symptoms and still others reported the prevalence of a certain cut-off point. Time frames for prevalence also varied. Sample size varied widely from thirty-one military ophthalmologists (Mier-Bolio et al., 2020) to a survey with 18,449 respondents (Morales Chainé et al., 2022). A survey of 1,338,320 participants throughout Latin America was also reported (Herrera-Añazco et al., 2022), although no sample size or data are available for each country individually.
Some reports are more methodologically sound because they used a longitudinal design or multiple, repeat and comparable surveys. A study obtained a sample of 2,307 older adults in the State of Mexico, enrolled in social programs for older adults, with the first evaluation conducted between April 7 and 17, 2020 (wave 1- W1); wave 2 was completed the same year between May 10 and 22, and wave 3 was conducted between September 28 and October 5 (Betancourt-Ocampo et al., 2022). The authors concluded that more anxiety symptoms were observed among older adults in the last wave (prevalence of anxiety symptoms at W1 = 3.9%, W2 = 5.1% and W3 = 7.8%). However, the proportion of older adults identified with high scores was lower than that reported in national data, at least for depressive symptoms.
Another study focused on a longitudinal sample of teachers at two stages: pre-pandemic (November 2019, n = 1,152) and during the pandemic (June-July 2020 and June-July 2021, n = 1,088) (Cortés-Álvarez et al., 2022). This is the only study to report pre-pandemic prevalence. Extremely severe anxiety was reported by 9.93% prior to the pandemic, 10.75% in first measurement during the pandemic period and 13.33% in the second pandemic period. They concluded that “As the COVID-19 pandemic progressed, teachers experienced higher prevalence of severe anxiety symptoms, higher mean number of symptoms, especially among women…”
A small study of 109 health care workers (Jáuregui Renaud et al., 2021) was conducted from April to July 2020, with a second measurement being taken from December 2020 to January 2021 during the pandemic, with no pre-pandemic data. They concluded that, “During the first epidemic wave (April 2020), health workers reported acute stress related to COVID-19, which was related to state anxiety. After the first epidemic wave, acute stress decreased, with no increase during the second epidemic wave (December 2020), and further decreased when vaccination started.”
Five repeated surveys of a national sample of cellphone respondents was performed (Teruel Belismelis & Pérez Hernández, 2021) on April 2020, n = 833, May 2020, n = 1,688, June 2020, n = 1,674, July 2020 n = 1,584 and August 2020, n = 1,538. Prevalence of anxiety in the previous two weeks, determined through the GAD-7 (see Table A4 of Anxiety, notes), remained stable during the pandemic: April 32.4%, May 31.4%, June 32.5%, July 30.9% and August 32.4%. The authors reported no pre-pandemic prevalence of anxiety for comparison.
Finally, a local longitudinal survey in the State of Mexico was conducted of 670 adult respondents (ages eighteen to sixty), on the list of beneficiaries of a government program interviewed first from April 8 to 18 2020 and subsequently from May 11 to 27 2020 (Toledo-Fernández et al., 2021). Prevalence of moderate to severe anxiety in the previous two weeks was 11.94% in the first measurement and 12.23% in the second. “No significant changes between the two waves” were observed.
Depression
A total of fifty-eight studies focused on depression. As with what was found for studies on anxiety symptoms, most studies are one-time, cross-sectional surveys with online recruitment with various levels of aggregation (local, national and international). Response rates are not usually provided. Thirteen instruments (see Table A5 Depression) were used to screen for depression symptoms. The different time frames, populations, and age groups surveyed make comparisons difficult. One study reported data for just fourteen adolescents (Fernandes et al., 2020) while another surveyed 1,338,320 participants across Latin America (Herrera-Añazco et al., 2022), but no sample size or data are available for each country individually.
Several of the best reports we have identified for anxiety symptoms also included measurement for depression (see the section on Anxiety for the overall methodology of these studies), namely (Betancourt-Ocampo et al., 2022; Cortés-Álvarez et al., 2022; Jáuregui Renaud et al., 2021; Toledo-Fernández et al., 2021). Betancourt-Ocampo et al. (2022) found higher scores in the third wave with respect to the two previous ones. However, the proportion of older adults with high scores in depression was lower than that reported in national data. Cortés-Álvarez (Cortés-Álvarez et al., 2022) reported a prevalence of extremely severe depression symptoms during the pre-pandemic of 8% and for two periods during the pandemic, of 8.55% from June to July 2020 and of 9.28% from June to July 2021. No significant differences in depression were reported. The study by Jauregui did not report changes in depression symptoms and concluded that “The second epidemic wave reported more symptoms of depression in association with acute stress, state anxiety, and burnout.”
Another three longitudinal studies focused on depression symptoms alone. The first was a small study of participants in HIV pre-exposure prophylaxis (IMPrEP), interviewed in 2019 (with a prevalence of 8.6% of depression symptoms according to CED-D in the past week) and again in 2020 (prevalence of 53.3%), compared with a national prevalence of 10.4% reported by the ENSANUT 2018 (Cerecero-Garcia et al., 2021). This is one of the few studies to report response rates (29% of those invited to take part and 67% of participants who completed the survey). The authors concluded that, “Our findings suggest high levels of depression among MSM and TGW in Mexico during the COVID-19 pandemic.”
Another longitudinal study of a sample of 247 medical undergraduate students at La Salle University in Mexico City using the Beck Depression Inventory (with no response rate being reported) found that in April 2020, the prevalence of depression during the past two weeks had been 19.84% (23.67% in women and 11.54% in men) whereas in December 2020, it had been 40.08% (42.60% in women and 34.62% in men). They concluded that, “The pandemic has increased the rate of depression in medical students, being more severe in women and those without previous psychiatric treatment.”
Finally, a longitudinal study of 466 expectant mothers first interviewed in 2018-2019 and subsequently in May–November 2020 was reported using the Edinburgh Postnatal Depression Scale (Rivera-Rivera et al., 2021). No response rate was provided. Prevalence of depression symptoms in the past seven days was 19.5% at baseline (2018-2019) and 19.1% in 2020. The authors concluded that, “While we did not find significant differences in the prevalence of depression before and during the pandemic, we did find that the direction of the change in depressive symptoms during a global pandemic was predicted by both negative life events and social support.”
Gaming
Only five studies reported on gaming or internet use during the pandemic. Given the dearth of studies in Mexico in the past decade, since the definition of internet gaming disorder in the DSM-5, the lack of interest in the topic by researchers is hardly surprising, even though concern was expressed during the pandemic about the increased time spent on online games among youth. Three out the five studies were international efforts that included Mexico and only two were stand-alone surveys in Mexico. One of these international studies (Fernandes et al., 2020) only surveyed 185 self-selected students (including fourteen in Mexico) and a single cross-sectional survey concluded that “adolescents have generally increased their use of social media sites and streaming services.” The other studies delved into risk factors for internet use during the pandemic, such as being infected with COVID-19 or fears associated with COVID-19. No clear conclusion is possible from these limited studies.
Sleep problems
A total of fifteen studies included data on sleep problems or quality (SQ) during the pandemic. They were almost all based on convenience samples without pre-COVID-19 data, except for one study of students (Delgadillo-Arteaga et al., 2021). These studies usually only have 25%-35% of male participants, but regardless of this limitation, several studies concluded that women were more affected than men. While some studies were very small (for example, (Arrona-Palacios et al., 2022) N = 214, a large study of healthcare workers was also reported (Robles et al., 2021a) N = 4,670.
This last study was timely, since it was conducted at an early stage of the pandemic (between May 8 and August 18, 2020) and focused on healthcare workers. It used standard instruments, adhered to ethical guidelines, performed rigorous data analyses and was cautious about its conclusions. It also shows the limitations of open platforms for the online recruitment of early studies. According to the authors, “Mexican HCWs were invited to participate in the survey through official media,” and “A convenience sample of Mexican nurses, general practitioners, medical residents and specialists was obtained by inviting healthcare workers dealing with COVID-19 patients to complete an online, cross-sectional survey.” Although it stated that, “The study target population includes approximately 315,000 nurses, 270,600 general practitioners, 22,613 medical residents, and 147,910 medical specialists,” there was no attempt to calculate or report on response rates by basic demographics or target population. Comparisons were not age/sex standardized. It did not use Mexican data on healthcare workers to compare them with those in this survey, at least for some variables such as depression. The authors concluded that insomnia was “more frequent in frontline healthcare workers and women,” which was attributable to their lack of rest time.
Other studies with convenience samples were less cautious about attributing sleep alterations to the pandemic, such as the one by (Rodríguez-Hernández et al., 2021): “The quality and quantity of sleep has been severely affected during the COVID-19 pandemic.”
Suicidal thoughts and behaviours
There were four reports on suicide deaths using modern time-trend methodology (Borges et al., 2022a; 2022b; Pirkis et al., 2022; 2021). These reports showed that, depending on the stage of the pandemic and the number of years used for comparison with the COVID-19 period, suicide increased or decreased slightly in Mexico. Suicide remained stable during the first nine months of COVID-19 in nineteen states, decreased in seven, and increased in six. Mixed trends were also reported when Mexico was included in international comparisons, particularly when age/sex groups were examined separately.
Five studies reported on suicide attempts, including a longitudinal study of university students (Borges et al., 2023) and a repeated cross-sectional face-to-face national survey (Valdez-Santiago et al., 2022). Neither surveys observed an increase in suicide attempts during the pandemic. The other three surveys used convenience samples of self-selected internet users and although they explored risk factors for suicide attempts during the pandemic, did not comment on trends.
Studies on suicide ideation were far more common. Comparison of results is difficult because these studies used different instruments, time periods for measuring prevalence and cut-off points for caseness. Most surveys were cross-sectional, using self-selected samples without any controls for suicide ideation prior to the pandemic. The risk factors for suicide ideation in these cross-sectional surveys varied widely, depending on the interest of the authors. A few studies on suicide ideation included a longitudinal comparison (Domínguez-González et al., 2022) of suicide ideation in two comparable surveys (Valdez-Santiago et al., 2022), with neither report finding differences in suicide ideation in the two measurements (pre- and during COVID-19). Another longitudinal study including suicide ideation (Borges et al., 2023) concluded that there had been an increase in the incidence of suicide ideation during the COVID-19 period compared to the pre-COVID-19 period. This increase was mostly found among students with a greater sense of vulnerability, poor coping skills and a previous mental disorder.
DISCUSSION AND CONCLUSION
In Mexico, as elsewhere, the COVID-19 pandemic led to urgent efforts to address its possible mental health consequences. This urgency yielded an initial wave of studies that were mostly cross-sectional and based on self-selected samples of respondents recruited through websites. Prevalences obtained from these samples, including the largest ones, are not representative of the Mexican population or of certain sectors of the population (such as students or the elderly). While several of these cross-sectional surveys included validated instruments for screening for symptoms of mental disorders (anxiety, depression, and alcohol use disorders), the prevalence they reported is not directly comparable with surveys prior to the pandemic period, as recruitment methods varied. Moreover, most surveys fail to provide readers with any Mexican data collected before COVID-19. While some of these prevalences found during COVID-19 are alarming, we have no way of knowing how much they differ from previous estimates. Although Mexico lacks a large stock of national or local surveys of the general population or specific groups to compare with surveys taken during COVID-19, efforts to gather this information are valuable. For example, during COVID-19, a 17.5% prevalence of Depression Symptoms (DS) in the past seven days was reported among pregnant women using the Edinburgh Depression Scale (Medina-Jiménez & Ródenas, 2022). A search of common databases yielded a national study, the Mexican National Health and Nutrition Survey (Instituto Nacional de Salud Pública, 2012) in which DS were measured by CESD-7, showing a prevalence of 21.36% (de Castro et al., 2017). Data were also obtained from the National Addictions Survey (ENA) 2008 on women pregnant at the time of the interview, among whom the prevalence of depressive symptoms was 16.2% (CES-D ≥ 16) (Lara-Cantú et al., 2014). These earlier national estimates could shed light on figures reported by cross-sectional studies during the COVID-19 period, with the caveat that some of these pre-COVID-19 studies are not representative of a specific population.
Limited efforts in Mexico to provide pre- and post-COVID-19 estimates were found, together with longitudinal studies, mostly performed at two or more time points of data collection during the pandemic. Some longitudinal or repeated surveys lacked a pre-COVID-19 estimate to compare with the COVID-19 period. It is important to distinguish between two issues explored by longitudinal or repeated surveys. One is whether the prevalence of mental health symptoms increased during COVID-19, compared with the pre-pandemic period. In Mexico this was explored by comparing national surveys prior to and during COVID-19 on alcohol use (Barrera-Núñez et al., 2022), time-trend studies on suicide (Borges et al., 2022a; 2022b), suicide ideation and attempts by cohort (Borges et al., 2023) and repeated surveys (Valdez-Santiago, 2022). A second issue, also addressed by Mexican researchers, is whether the symptoms of mental health problems changed during the initial and subsequent phases of the pandemic, as borne out by studies on alcohol (Domínguez-González et al., 2022), anxiety (Betancour-Ocampo et al., 2022), depression (Toledo-Fernández et al., 2021), suicide ideation (Domínguez-González et al., 2022), and a range of mental health outcomes (Robles et al., 2021a; Robles et al., 2021b). As mentioned earlier, cohort studies and large-scale international time-trend studies have found fewer mental health consequences of the COVID-19 pandemic than cross-sectional studies of the early phase of the pandemic. Accordingly, the results of these fourteen longitudinal datasets in Mexico suggest a more cautious interpretation of the effects of the COVID-19 pandemic on the mental health of Mexicans. This conclusion is in line with recent meta-analyses on the issue (Witteveen et al., 2023; Ahmed et al., 2023). A meta-analysis of longitudinal studies on mental health and COVID-19 even reported that “anxiety and depression symptoms may have decreased from baseline to follow up, while other mental health problems showed no change” (Cénat et al., 2022).
In conclusion, the COVID-19 pandemic resulted in a series of initial quick studies which, while serving as a warning sign, did not necessarily follow standard epidemiological principles. These initial efforts were followed by rigorous epidemiological studies. An earlier review of the international literature on COVID-19 and mental health suggested several areas for improvement for new studies: better definition of outcomes and use of standard instruments, reports on symptom severity, and definition of sample characteristics and response rates, to define and expand the population under study and the use of more longitudinal study designs (Chen et al., 2022). These suggestions for improving results should obviously be implemented in Mexico, to enhance preparedness and offer guidance for future contingencies.