Salud mental 2025;
ISSN: 0185-3325
DOI: 10.17711/SM.0185-3325.2025.004
Received: 23 February 2024
Accepted: 19 July 2024
Evaluation of a Brief Mindfulness-based Intervention to Prevent Problematic Substance Use among First-year Medical Students
Arturo Ortiz Castro1 , Rosalía Pilar Bernal Pérez1 , Ingrid Vargas Huicochea2 , Aurora Farfán Márquez3 , Julio César Flores-Castro4
1 Directorate of Epidemiological and Psychosocial Research. Instituto Nacional de Psiquiatría Ramón de la Fuente Muñiz, Mexico City, Mexico.
2 Research Coordination. Department of Psychiatry and Mental Health. School of Medicine. National Autonomous University of Mexico, Mexico City, Mexico.
3 Academic Excellence Program. General Secretariat. School of Medicine. National Autonomous University of Mexico, Mexico City, Mexico.
4 Analytical Experience Consultant, Mexico City, Mexico.
Correspondence: Arturo Ortiz Castro. Directorate of Epidemiological and Psychosocial Research. National Institute of Psychiatry Ramón de la Fuente Muñiz. Calzada México-Xochimilco 101, San Lorenzo Huipulco, Tlalpan, 14370, Ciudad de México, Mexico. Phone: +52 (55) 4160-5172. email: ortizimp@yahoo.com.mx
Abstract:
Introduction. Beginning a degree in medicine involves a significant change in a student’s lifestyle, particularly during the early years, since stressful situations are difficult to address.
Objective. To evaluate the effectiveness of Mindfulness Based Intervention (MBI) in medical students to reduce problematic substance use, stress, anxiety, and depressive symptomatology.
Method. Experimental study of two groups with simple random assignment in a sample comprising 320 students.
Results. The mean age of participants was 19; 85% reported having consumed alcohol at some time in their lives, 48% tobacco and 18% cannabis. Alcohol and tobacco use decreased slightly from baseline to follow-up in the group that received a MBI. At the same time, there was a statistically significant decrease in stress in the experimental group and anxiety decreased in both groups with statistically significant changes due to a probable imitation effect.
Discussion and conclusion. The downward trend in alcohol and tobacco consumption could have intensified if the full intervention program had been completed, as observed in other studies in which five or more MBI sessions were given, achieving significant improvement. The reduction in the level of the variables examined coincides with studies showing the benefits of MBI as a mechanism for emotional regulation to cope with adverse events.
Keywords: Students, anxiety, depression, stress, alcohol, drugs, mindfulness.
Resumen:
Introducción. Ingresar a la carrera de medicina implica un notorio cambio en el estilo de vida de un estudiante, especialmente durante los primeros años, ya que se presentan situaciones estresantes difíciles de enfrentar.
Objetivo. Evaluar la efectividad de una intervención basada en la Atención Plena (AP) en estudiantes de medicina para atenuar el uso problemático de sustancias, el estrés, la ansiedad y la sintomatología depresiva.
Método. Estudio experimental de dos grupos con asignación aleatoria simple. La muestra estuvo conformada por 320 estudiantes.
Resultados. 69% fueron mujeres y el resto hombres, la media de edad de los participantes fue de 19 años; 85% reportaron haber consumido alcohol alguna vez en la vida, 48% tabaco y 18% cannabis. El consumo de alcohol y de tabaco disminuyó ligeramente de la línea base al seguimiento en el grupo que recibió la AP. A su vez, el estrés tuvo también una disminución estadísticamente significativa en el grupo experimental y la ansiedad disminuyó en ambos grupos con cambios estadísticamente significativos bajo un probable efecto de imitación.
Discusión y conclusión. La tendencia a la baja en el consumo de alcohol y tabaco pudo haberse fortalecido una vez concluido el programa completo de intervención, como se observó de igual manera en otros estudios en que se impartieron cinco o más sesiones de AP, que muestraron mejoras significativas. La reducción en el nivel de las variables estudiadas coincide con estudios que dan cuenta de los beneficios de la AP al actuar como mecanismo de estabilización emocional frente a eventos adversos.
Palabras clave: estudiantes, ansiedad, depresión, estrés, alcohol, drogas, atención plena.
INTRODUCTION
Starting higher education involves stressful changes in the lifestyle of young people (Tian-Ci Quek et al., 2019) and is compounded by the fact that medical students are extremely competitive (Hill et al., 2018).
A low level of stress can enhance various areas of human behavior. However, when stress is present at high levels, it can be associated with depressive symptomatology, poor academic performance, substance use, the desire to drop out of school and, in extreme cases, suicidal ideation (Marcon et al., 2020; Kumar et al., 2019; Hill et al., 2018).
Recurrent exposure of students to stressful events—of varying intensity—can affect their mental health. Thus, for example, the percentage of depression in medical students ranges from 14.3 to 57.6%, while the percentage for anxiety in this same group ranges from 7.7 to 65.5% (Kumar et al., 2019; Tian-Ci et al., 2019; Zeng et al., 2019; Kunwar et al., 2016; Hope & Henderson, 2014). Hill et al. (2018) conducted a study of 978 medical students, finding that 11.2% described their stress as severe and debilitating, while 68.6% considered it significant yet manageable.
Karyotaki et al. (2020) conducted research on first-year medical students from nine countries, including Mexico, observing percentages of depression and anxiety of 13.4 and 13.1%. Benjet et al. (2019) found that first-year students presented similar percentages indicative of suicide attempt (23%), depression (12.6%) and anxiety (13.6%) to those of international studies.
Stress is also associated with alcohol and drug use (Molodynski et al., 2020). Marcon et al. (2020), Steiner-Hofbauer & Holzinger (2020) and Kushwaha et al. (2019) found that 59.6% of a sample of medical students reported alcohol use, 28.2% tobacco use and 11.9% marijuana use. In the case of Mexican students, 46% were found to consume alcohol in alarming amounts (Puig-Nolasco et al., 2011).
Given the evidence of the problems described, programs have been developed to enhance mental health and reduce anxiety, depression and stress levels (Slavin & Chibnall, 2016), as well as suicidal ideation (Witt et al., 2019). Medical students and certain schools have begun to include self-care programs in their syllabuses (Hassed et al., 2008) to provide students with strategies to manage stress and reduce drug use.
One approach used is the Mindfulness-Based Intervention (MBI), whose philosophical, epistemological, theoretical, and phenomenological tenets are based on Buddhism and meditation. It focuses on awareness, attention, acceptance, and remembrance; promotes the observation of the present reality, the understanding of the body and mind, and provides a new understanding of the experiences, sensations, emotions, and thoughts of each person without judgment (Oró et al., 2021; Peláez et al., 2021; Vásquez-Dextre, 2016; Nyanaponika, 1962).
MBI comprises two components: self-regulation of attention and coping with experiences. According to this approach, it is assumed that it is possible to enable people to reduce stress, anxiety, depression and substance use (Tanay et al., 2012). MBIs promote physical and emotional well-being, which is why they have been used in various therapeutic and educational contexts, sometimes with the incorporation of electronic devices (Diez & Castellanos, 2022; Errasti-Pérez et al., 2022; Döllinger et al., 2021; Wielgosz et al., 2019; Kabat-Zinn, 2015; Vettese et al., 2009; Goldin & Gross, 2010).
Several studies have observed an improvement in those who received an MBI, in comparison with control groups with stress, depressive, somatic, anxious and emotional exhaustion symptoms, in the perception of their quality of life, perceived difficulty, personal and social well-being, burnout and, of course, drug use. They were also observed to have better treatment adherence (Félix-Junior et al., 2022; Bazzano et al., 2022; Kriakous et al., 2020; Chmielewski & Łuczyński, 2021; Oró et al., 2021; Zemestani & Fazeli Nikoo, 2020; Buizza et al., 2020; Kwok et al., 2019; Lomas et al., 2018; Ruiz-Fernández et al., 2019; Spinelli et al., 2019).
Likewise, studies such as those by Nogueira et al. (2022), López et al. (2021), Santiago & Urcuhuaranga (2021), Zúñiga et al. (2021), Alvarado& Daza (2020) and Buizza et al. (2020), have observed positive results in the improvement of stress management, burnout, resilience, concentration, attention, anxiety, motivation, self-acceptance and social support among medical students.
Single et al. (2019) found that behaving with awareness, nonjudgment, and nonreactivity to internal experience predicted decreased alcohol consumption, which was mediated by low levels of emotional psychopathology.
Li et al. (2017) conducted a systematic review of studies evaluating MBI interventions for substance use. They observed a reduction in substance use, craving, and withdrawal symptoms at the end of treatment and at follow-up in subjects who had received the intervention compared to those who had received treatment as usual, such as relapse prevention, cognitive behavioral therapy and/or joining a support group. This review was updated by Korecki et al. (2020), finding the same results.
Finally, it has been observed that MBI can reduce the likelihood of drug and alcohol use among students directly or through emotion regulation (Garland et al., 2022; Nosratabadi & Halvaiepour, 2019; Black et al., 2011).
The aim of the present article was therefore to evaluate the effectiveness of an MBI in medical students to prevent problematic substance use, stress, anxiety and depressive symptomatology.
METHOD
Study design
We used an experimental study of two groups with simple random assignment.
Sample description
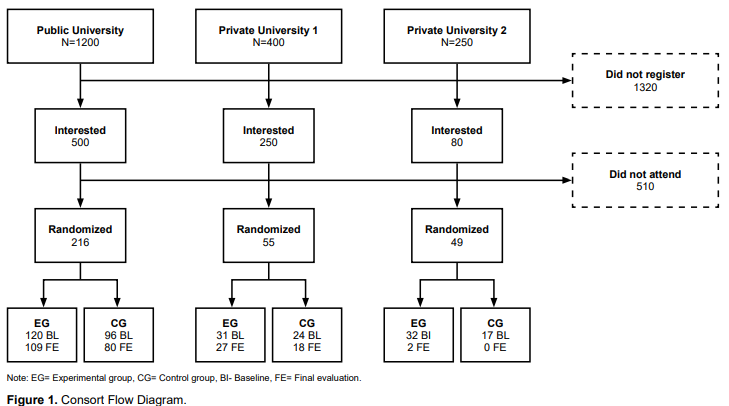
The study was conducted at three universities in Mexico City, one public and two private, from October 2019 to March 2020. A total of 2,150 students were invited to participate, of which 830 showed interest in participating in the workshops. Three hundred and twenty were randomized and divided into two groups: experimental and control, after filling in the informed consent form, meeting the inclusion criteria and completing the baseline (BL), and 236 completed the final evaluation (FE) (Figure 1).
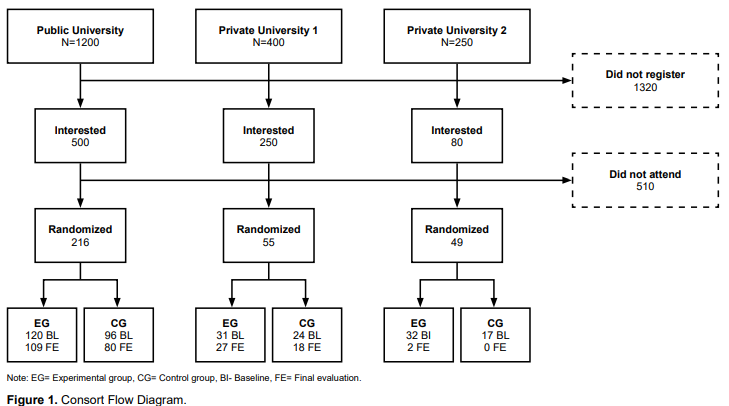
view
Measurements
The questionnaire comprised the following six sections:
Sociodemographic data. This section comprised 16 questions on sex, age, pregnancy status, date of birth, place of birth, school, group, medical diagnosis, specific diagnosis, medication intake, specific medication, pharmacological treatment for psychiatric or neurological problems, name, email, cell phone, and other means of contact. For the purposes of the study, the seven main variables are reported in the results and tables sections: sex, age, birthplace, school, medication intake, medical diagnosis, pharmacological treatment.
Perceived Stress Scale (PSS). Developed by Cohen et al. (1983), this scale assessing the level of perceived stress during the past month comprises 14 items with a five-point Likert-type response format (0 = never to 4 = very often). The total PSS score is obtained by inverting the scores of items 4, 5, 6, 7, 9, 10 and 13 and adding the 14 items, with a higher score corresponding to a higher level of perceived stress. The results of the adaptation tested in a Mexican population, conducted by González et al., (2007), indicate adequate internal consistency (α = .83).
Beck Anxiety Inventory (BAI). Comprises 21 items describing common anxiety symptoms and assesses the degree of distress of each item during the past week on a 4-point Likert-type scale (0 = not at all to 3 = severely). According to Beck et al. (1993), the BAI showed internal consistency of .92. The Mexican version for adults has obtained alphas of .94 and .83 (Hernández et al. 2022; Robles et al., 2001).
Beck Depression Inventory (BDI). Developed by Beck et al. (1987), this inventory comprises 21 items describing common depression symptoms, used to evaluate the degree of distress of students in the past week on a 4-point Likert-type scale (0 = absence to 3 = maximum severity). The total score is obtained from the sum of the items, with a score above 10 indicating the presence of depression. Jurado et al. (1998) translated, adapted, and standardized the inventory for the Mexican population, with adequate concurrent validity (r = .70) and high internal consistency (α = .87), while Hernández et al. (2022) obtained internal consistency of .92.
Five Facets of the Mindfulness Questionnaire (FFMQ-M; Baer et al., 2006; Baer et al., 2008). The questionnaire comprises 39 items with a 5-point Likert-type response format (1 = never to 5 = very often), measuring mindfulness, based on five main facets: “Observing,” “Describing,” “Acting with Awareness,” “Not judging the internal experience,” “Not reacting to the internal experience” and “Taking a step back.” The questionnaire has been validated in the Spanish population by Cebolla et al. (2012) and in the Mexican population by Meda et al. (2015).
Alcohol, Tobacco and Substance Use Screening Test (ASSIST). This test identifies the use of tobacco, alcohol, marijuana, cocaine, amphetamine-type stimulants, inhalants, sedatives, hallucinogens, opiates, and other drugs. It comprises eight questions enquiring about use and associated problems in the past three months (Ali et al., 2002). Each substance is assessed for a risk score: low (0-3 points), moderate (4-26 points) and high risk (> 26 points). International studies have reported both validity and reliability, with a test-retest coefficient of .58-.90 and internal consistency of .80. Internal consistency of .87 was found in the Mexican population (Tiburcio et al., 2016; Khan et al., 2011).
Procedure
An agreement was initially sought with three universities. Once this had been established, first-year medical students were invited to participate through a poster and information sessions, the standard pre-pandemic means employed at institutions for this purpose. Interested students were offered more information about the project and invited to participate in the study and to sign the informed consent form. The control and experimental groups were formed with students from the three universities and BL measurements taken of each group. The experimental group received an intervention based on MBI, through five two-hour sessions. At the end of the intervention, the final evaluation was administered, using the same instruments as in the BL.
Inclusion and exclusion criteria
Inclusion criteria: First-semester medical students at the time of the study, who agreed to participate voluntarily.
Exclusion: Presence of severe pathology or receiving any type of psychotherapy at the time of the study or in the past six months.
Elimination: failure to complete the registration and/or the interventions, and conditions that prevented them from answering the questionnaires or participating in the interventions (such as headaches, wakefulness, nausea, and the influence of psychoactive substances).
Data analysis
Frequencies and measures of central tendency were obtained for each question. To establish comparisons by demographic data, X2 or Student’s t analyses were performed according to the level of measurement of each variable. Analysis of variance (ANOVA) was calculated using treatment condition as the independent variable. Data were analyzed using the IBM SPSS v26 statistical software. For the purposes of the analysis, the control groups from the three universities and the experimental groups were combined.
Ethical considerations
The present study constituted minimal risk research because the main objective was to promote the emotional well-being of participants. The original research protocol was approved by the Fundación Gonzalo Río Arronte and the Ethics Committee of the Medicine Faculty (FM/DI/098/2019).
RESULTS
Sample characteristics: 137 (42.8%) of the randomized students were in the control group and 183 (57.2%) in the experimental group. Most of the participants were female (69.4%), with a mean age of 19 (SD = 1.5±). Regarding their place of birth, 51% were originally from Mexico City and 67.5% studied at a public university. It is worth noting that 13.1% reported taking some form of medication, 15.5% had been given a medical diagnosis and 5.9% were under pharmacological treatment for a psychiatric or neurological problem (Table 1).

view
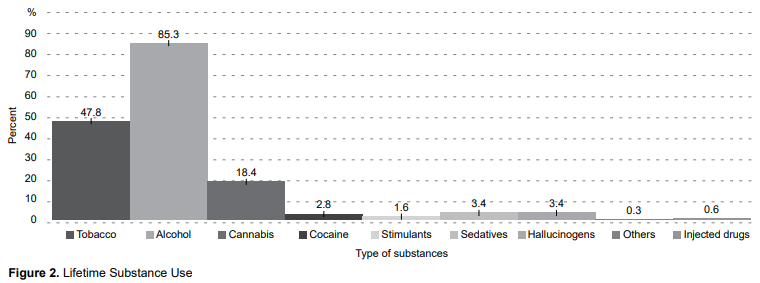
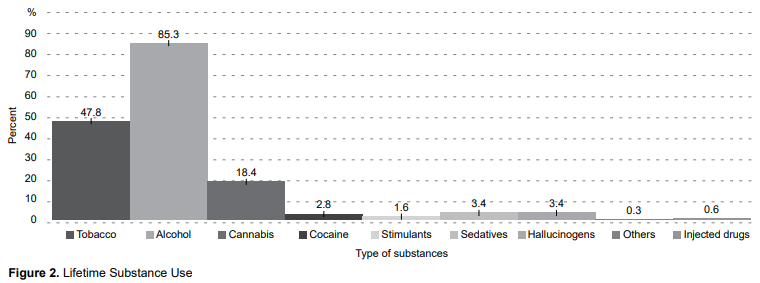
In terms of substance use, alcohol was the substance most commonly reported by students, with 85.3% of lifetime users, followed by tobacco (47.8%) and cannabis (18.4%). Although the use of other substances was reported, percentages were so low that they were not included in the following analyses (Figure 2).
view
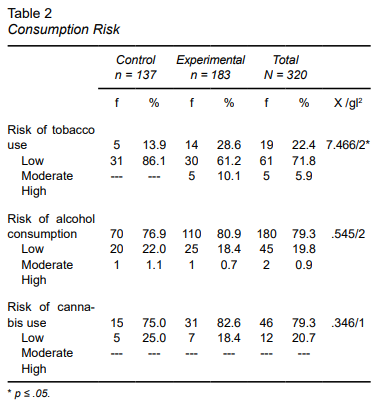
With respect to the difference in risky consumption between the control and experimental groups, significant differences were only found in tobacco use levels, with 10.1% of members of the experimental group presenting a high risk of tobacco dependence (Table 2).
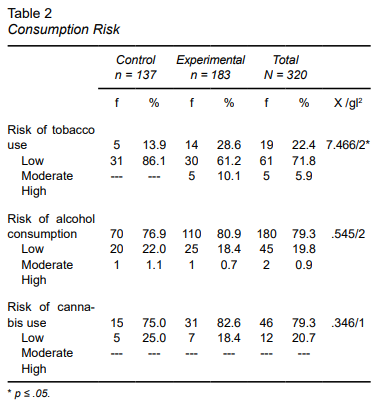
view
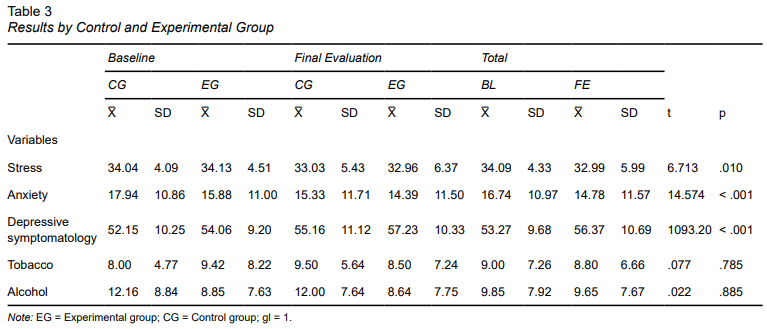
Stress underwent a statistically significant decrease in the experimental group; and anxiety decreased in both groups with statistically significant changes. However, depression showed a statistically significant increase in both the experimental and control groups (Table 3).
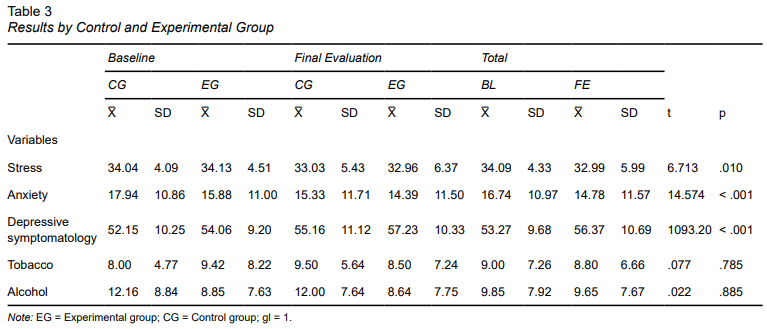
view
It is important to note that although there were no statistically significant differences in substance use, there was a slight decrease in tobacco and alcohol use in the baseline follow-up of the group that received the MBI.
DISCUSSION AND CONCLUSION
The aim of the present study was to evaluate the effectiveness of a Mindfulness-based intervention in medical students to prevent stress, anxiety, depressive symptomatology, and problematic substance use. The study was conceptualized and undertaken in keeping with the mental health status of students at the levels of the pre-pandemic context. In this regard, 85% of the students surveyed reported lifetime use of alcohol, 47.8% of tobacco and 18.4% of cannabis.
The literature review responds to a limited context regarding studies focused on substance consumption in first-year medical students in Mexico City prior to lockdown. However, some international studies (Martínez et al., 2018; Haas et al., 2018; Sommet et al., 2012; Akvardar et al., 2003) report similar percentages to this study, while others report different percentages (Lemos-Santos et al., 2024: Fernández et al., 2018; Newbury-Birch et al., 2000). Since the difference in results could be due to the different sample populations, further research is required in Mexico.
Although no statistically significant decrease in substance use was found after participants had received the intervention, a slight decrease in alcohol and tobacco use was observed in the experimental group. This trend may have increased with the completion of the full intervention program (Baeza-Velasco et al., 2020; Black et al., 2011), as significant improvements have been observed in studies where more than five sessions of MBI were provided, (Barros et al., 2021; Zamboni et al., 2021; Nawi et al., 2021; Goldberg et al., 2021; Wupperman et al., 2019; Cavicchioli et al., 2019).
The results also indicate that stress symptoms decreased with statistically significant differences in the group receiving the MBI, consistent with what has been reported in other studies with medical students (Polle, & Gair, 2021; Daya & Hearn, 2017; Khoury et al., 2015), in which students’ improvement was attributed to increased awareness, and recognition of levels of tension, pain, bodily and mental rigidity.
The literature points out that although MBI achieves positive results in cross-sectional studies, these studies are still considered to have certain limitations in regard to the safety of medium and long-term effects, so it is suggested that actions designed to narrow these gaps be implemented, as this could enhance the effectiveness of MBI in this population (Sekhar et al., 2021).
At the same time, a decrease in anxiety symptoms was found, coinciding with the systematic review by Krishnan et al. (2022), in which significant decreases were observed in various studies worldwide. Anxiety is regarded as one of the most prevalent problems (Aljuwaiser et al., 2023) and one of the most intractable among students themselves, as they perceive it as “a complication inherent to the nature of the degree course” due to the academic workload, the competitiveness of the environment and the uncertainty regarding job opportunities in the future (Tian-Ci et al., 2019; Hill et al., 2018).
The study was conducted at the beginning of the pandemic (October 2019-March 2020), a period that overlapped with the first cases of COVID 19 in Mexico (January-February 2020) as reported by WHO (2020) and the Ministry of Health (2020). The outbreak of the pandemic may have contributed to the significant increase in depressive symptoms in both the control and experimental groups, as the uncertainty and fear caused by the announcement of lockdown affected medical, paramedical and trainee staff more than the general population or students in other degree courses (Piñel et al., 2021; Shao et al., 2020). The uncertainty and fear were partly due to concerns about the negative impact of COVID-19 on education, employment and their future (Xie et al., 2021).
This study has several limitations. It began before the pandemic and was conducted at the beginning of the latter, which did not allow for effective follow-up of participants. Moreover, the announcement of lockdown may have influenced answers in the evaluations of the two groups. Due to the limited availability of universities and the restrictions imposed by lockdown (Delgado et al., 2021), the eight sessions originally planned were reduced to five. However, the literature suggests that seven or more sessions are required for the internationalization of MBI principles in participants (Oró et al., 2021).
Given the importance of positively impacting the mental health of medical students, recommendations for future research include the following:
The use of manuals resulting from this experience, such as the “Mindfulness Instructor’s Manual for Mental Health Professionals” and the “User’s Manual on the Mindfulness Technique for students and the general public.”
Include other study variables, such as suicidal ideation, which can be by MBI (Bazzano et al., 2022).
Incorporate MBI into the curriculum, so that it influences all levels of training, to prevent drop out and emotional and behavioral problems derived from the strain inherent to professional training.
Finally, it should be noted that the COVID-19 epidemic was a phenomenon that was not considered at the beginning of the research. There were no indicators to suspect its outbreak or the subsequent lockdown stage, as a result of which students lost contact with the research team and each other, due, among other causes, to dropping out of their degree courses, returning to their places of origin (the provinces) and being assigned to hospitals to attend patients with COVID-19. In addition, the use of social networks was not as widespread as it is today, which made data collection difficult. However, despite these setbacks, relevant data supporting the efficacy of MBI for the management of substance use were obtained.
The results achieved through a reduction of stress and anxiety symptoms coincide with other studies showing the benefits of MBI, which serves as an emotional regulation mechanism in the face of adverse events. Likewise, substance use showed a downward trend. However, since these findings are not conclusive for this study population, it is suggested that the subject be further explored with other medical students, who present frequently situations of emotional imbalance.
Funding
This study was partly funded by the Fundación Gonzalo Río Arronte (SA-337) in conjunction with the Instituto Nacional de Psiquiatría Ramon de la Fuente Muñiz (INPRFM).
Conflict of interest
The authors declare that they have no conflicts of interest.
Acknowledgments
We would like to thank MSc. Mauricio Ramos Cruz for his comments and suggestions on the statistical and methodological aspects of this article, which proved extremely valuable for improving the quality of our study.
REFERENCES
Akvardar, Y., Demiral, Y., Ergör, G., Ergör, A., Bilici, M., & Akil Özer, Ö. (2003). Substance use in a sample of Turkish medical students. Drug and Alcohol Dependence, 72(2), 117-121. https://doi.org/10.1016/s0376-8716(03)00192-3
Ali, R., Awwad, E., Babor, T., Bradley, F., Butau, T., Farrell, M., Formigoni, M. L. O. S., Isralowitz, R., Boerngen de Lacerda, R., Marsden, J., McRee, B., Monteiro, M., Pal, H., Rubio-Stipec, M., & Vendetti, J.(WHO ASSIST Working Group) (2002). The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): Development, reliability and feasibility. Addiction, 97(9), 1183–1194. https://doi.org/10.1046/j.1360-0443.2002.00185.x
Aljuwaiser, S., Brazzelli, M., Arain, I., & Poobalan, A. (2023). Common mental health problems in medical students and junior doctors – an overview of systematic reviews. Journal of Mental Health, 33(6), 779-815. https://doi.org/10.1080/09638237.2023.2278095
Alvarado, E. & Daza, L. (2020). Mindfulness and its contribution to emotional balance in medical and nursing students at the Fundación Universitaria Juan N. Corpas. In: : Luis Miguel Piñeros, Luis Miguel Pombo, Carol A. Zuluaga & Liliana A. Naranjo (eds), Anuario de Investigación 2019-2020 (pp. 33-34), Fundación Universitaria Juan N. Corpas, Bogotá, Colombia.
Baer, R. A., Smith, G. T., Hopkins, J., Krietemeyer, J., & Toney, L. (2006). Using Self-Report Assessment Methods to Explore Facets of Mindfulness. Assessment, 13(1), 27-45. https://doi.org/10.1177/1073191105283504
Baer, R. A., Smith, G. T., Lykins, E., Button, D., Krietemeyer, J., Sauer, S., Walsh, E., Duggan, D., & Williams, J. M. G. (2008). Construct Validity of the Five Facet Mindfulness Questionnaire in Meditating and Nonmeditating Samples. Assessment, 15(3), 329-342. https://doi.org/10.1177/1073191107313003
Baeza-Velasco, C., Genty, C., Jaussent, I., Benramdane, M., Courtet, P., & Olié, E. (2020). Study protocol of a multicenter randomized controlled trial of mindfulness-based intervention versus relaxation to reduce emotional exhaustion in medical students in France: the “Must prevent” study. BMC Psychiatry, 20(1), https://doi.org/10.1186/s12888-020-02529-9
Barros, V. V., Opaleye, E. S., Demarzo, M., Curado, D. F., Bowen, S., Hachul, H., & Noto, A. R. (2021). Effects of Mindfulness-Based Relapse Prevention on the Chronic use of Hypnotics in Treatment-Seeking Women with Insomnia: a Randomized Controlled Trial. International Journal of Behavioral Medicine, 29(3), 266-277. https://doi.org/10.1007/s12529-021-10002-4
Bazzano, A. N., Sun, Y., Chavez-Gray, V., Akintimehin, T., Gustat, J., Barrera, D., & Roi, C. (2022). Effect of Yoga and Mindfulness Intervention on Symptoms of Anxiety and Depression in Young Adolescents Attending Middle School: A Pragmatic Community-Based Cluster Randomized Controlled Trial in a Racially Diverse Urban Setting. International Journal of Environmental Research and Public Health, 19(19), 12076. https://doi.org/10.3390/ijerph191912076
Beck, A., Epstein, N., Brown, G. & Steer, R. (1993). Beck anxiety inventory. Journal of consulting and clinical psychology, 56(6). https://doi.org/10.1037/t02025-000
Beck, A., Steer, R. & Brown, G.. (1987). Beck depression inventory. New York: Harcourt Brace Jovanovich.
Benjet, C., Gutiérrez-García, R. A., Abrego-Ramírez, A., Borges, G., Covarrubias-Díaz, A., Durán, M. D. S., González-González, R., Hermosillo-de la Torre, A. E., Martínez-Martínez, K. I., Medina-Mora, M. E., Mejía-Zarazúa, H., Pérez-Tarango, G., Zavala-Berbena, M. A., & Mortier, P. (2019). Psychopathology and self-harm among incoming first-year students in six Mexican universities. Salud Pública de México, 61(1), 16. https://doi.org/10.21149/9158
Black, D. S., Semple, R. J., Pokhrel, P., & Grenard, J. L. (2011). Component Processes of Executive Function—Mindfulness, Self-control, and Working Memory—and Their Relationships with Mental and Behavioral Health. Mindfulness, 2(3), 179-185. https://doi.org/10.1007/s12671-011-0057-2
Buizza, C., Ciavarra, V., & Ghilardi, A. (2020). A Systematic Narrative Review on Stress-Management Interventions for Medical Students. Mindfulness, 11(9), 2055-2066. https://doi.org/10.1007/s12671-020-01399-2
Cavicchioli, M., Movalli, M., & Maffei, C. (2019). Difficulties with emotion regulation, mindfulness, and substance use disorder severity: the mediating role of self-regulation of attention and acceptance attitudes. The American Journal of Drug and Alcohol Abuse, 45(1), 97-107. https://doi.org/10.1080/00952990.2018.1511724
Cebolla, A., García-Palacios, A., Soler, J., Guillen, V., Baños, R., & Botella, C. (2012). Psychometric properties of the Spanish validation of the Five Facets of Mindfulness Questionnaire (FFMQ). The European Journal of Psychiatry, 26(2), 118-126. https://doi.org/10.4321/s0213-61632012000200005
Chmielewski, J., Łoś, K., & Łuczyński, W. (2021). Mindfulness in healthcare professionals and medical education. International Journal of Occupational Medicine and Environmental Health, 34(1), 1-14. https://doi.org/10.13075/ijomeh.1896.01542
Cohen, S., Kamarck, T., & Mermelstein, R. (1983). A Global Measure of Perceived Stress. Journal of Health and Social Behavior, 24(4), 385-396. https://doi.org/10.2307/2136404
Daya, Z., & Hearn, J. H. (2017). Mindfulness interventions in medical education: A systematic review of their impact on medical student stress, depression, fatigue and burnout. Medical Teacher, 40(2), 146-153. https://doi.org/10.1080/0142159x.2017.1394999
Delgado Ramos, G. C., Zanella, R., Cota Araiza, L., & López Torres, R. (2021). Impacto de la pandemia COVID-19 en la investigación y docencia en las nanociencias y la nanotecnología en México. Mundo Nano. Revista Interdisciplinaria en Nanociencias y Nanotecnología, 14(27), 1e-19e. https://doi.org/10.22201/ceiich.24485691e.2021.27.69685
Diez, G. G., & Castellanos, N. (2022). Investigación de mindfulness en neurociencia cognitiva. Revista de Neurología, 74(5), 163-169. https://doi.org/10.33588/rn.7405.2021014
Döllinger, N., Wienrich, C., & Latoschik, M. E. (2021). Challenges and Opportunities of Immersive Technologies for Mindfulness Meditation: A Systematic Review. Frontiers in Virtual Reality, 2, https://doi.org/10.3389/frvir.2021.644683
Errasti-Pérez, J., Al-Halabí, S., López-Navarro, E. & Pérez-Álvarez, M. (2022). Mindfulness: Whyitmayworkandwhy it is sure to succeed. Behavioral Psychology / Psicología Conductual, 30(1), 235-248. https://doi.org/10.51668/bp.8322112s
Fernández VAT, Geroy FA, Pérez RGI, Naranjo HL, Villafuerte RY. (2018). Sexual behavior of first year medical students at the Cienfuegos Medical Faculty. Influence of the gender role in risky conducts. Medisur, 16(2). https://www.medigraphic.com/cgi-bin/new/resumenI.cgi?IDARTICULO=81599.
Félix-Junior, I. J., Donate, A. P. G., Noto, A. R., Galduróz, J. C. F., Simionato, N. M., & Opaleye, E. S. (2022). Mindfulness-based interventions in inpatient treatment for Substance Use Disorders: A systematic review. Addictive Behaviors Reports, 16, 100467. https://doi.org/10.1016/j.abrep.2022.100467
Garland, E. L., Hanley, A. W., Nakamura, Y., Barrett, J. W., Baker, A. K., Reese, S. E., Riquino, M. R., Froeliger, B., & Donaldson, G. W. (2022). Mindfulness-Oriented Recovery Enhancement vs Supportive Group Therapy for Co-occurring Opioid Misuse and Chronic Pain in Primary Care. JAMA Internal Medicine, 182(4), 407. https://doi.org/10.1001/jamainternmed.2022.0033
Goldberg, S. B., Pace, B., Griskaitis, M., Willutzki, R., Skoetz, N., Thoenes, S., Zgierska, A. E., & Rösner, S. (2021). Mindfulness-based interventions for substance use disorders. Cochrane Database of Systematic Reviews, 2021(10), https://doi.org/10.1002/14651858.cd011723.pub2
Goldin, P. R., & Gross, J. J. (2010). Effects of mindfulness-based stress reduction (MBSR) on emotion regulation in social anxiety disorder. Emotion, 10(1), 83-91. https://doi.org/10.1037/a0018441
González Ramírez, M. T. & Landero Hernández, R. (2007). Factor Structure of the Perceived Stress Scale (PSS) in a Sample from Mexico. The Spanish Journal of Psychology, 10(1), 199-206. https://doi.org/10.1017/s1138741600006466
Haas, A. L., Wickham, R. E., McKenna, K., Morimoto, E., & Brown, L. M. (2018). Evaluating the Effectiveness of a Medical Amnesty Policy Change on College Students’ Alcohol Consumption, Physiological Consequences, and Helping Behaviors. Journal of studies on alcohol and drugs, 79(4), 523–531. PMID: 30079866.
Hassed, C., de Lisle, S., Sullivan, G., & Pier, C. (2008). Enhancing the health of medical students: outcomes of an integrated mindfulness and lifestyle program. Advances in Health Sciences Education, 14(3), 387-398. https://doi.org/10.1007/s10459-008-9125-3
Hernández Hernández, V. A., Marrufo, R. M., Esparza Del Villar, O. A., & Robles Ramírez, A. J. (2022). Validation of the Beck scales (anxiety and depression) in a border population (northern Mexico) during the COVID-19 pandemic. Sapienza: International Journal of Interdisciplinary Studies, 3(5), 155-168. https://doi.org/10.51798/sijis.v3i5.452
Hill, M. R., Goicochea, S., & Merlo, L. J. (2018). In their own words: stressors facing medical students in the millennial generation. Medical Education Online, 23(1), 1530558. https://doi.org/10.1080/10872981.2018.1530558
Hope, V., & Henderson, M. (2014). Medical student depression, anxiety and distress outside North America: a systematic review. Medical Education, 48(10), 963-979. https://doi.org/10.1111/medu.12512
Jurado, S., Villegas, M., Méndez, L., Rodríguez, F., Loperena, V., & Varela, R. (1998). La estandarización del Inventario de Depresión de Beck para los residentes de la Ciudad de México. Salud Mental, 21(3), 26-31.
Kabat-Zinn, J. (2015). Mindfulness. Mindfulness, 6(6), 1481-1483. https://doi.org/10.1007/s12671-015-0456-x
Karyotaki, E., Cuijpers, P., Albor, Y., Alonso, J., Auerbach, R. P., Bantjes, J., Bruffaerts, R., Ebert, D. D., Hasking, P., Kiekens, G., Lee, S., McLafferty, M., Mak, A., Mortier, P., Sampson, N. A., Stein, D. J., Vilagut, G., & Kessler, R. C. (2020). Sources of Stress and Their Associations With Mental Disorders Among College Students: Results of the World Health Organization World Mental Health Surveys International College Student Initiative. Frontiers in Psychology, 11, https://doi.org/10.3389/fpsyg.2020.01759
Khan, R., Chatton, A., Nallet, A., Broers, B., Thorens, G., Achab-Arigo, S., Poznyak, V., Fleischmann, A., Khazaal, Y., & Zullino, D. (2011). Validation of the French Version of the Alcohol, Smoking and Substance Involvement Screening Test (ASSIST). European Addiction Research, 17(4), 190-197. https://doi.org/10.1159/000326073
Khoury, B., Sharma, M., Rush, S. E., & Fournier, C. (2015). Mindfulness-based stress reduction for healthy individuals: A meta-analysis. Journal of Psychosomatic Research, 78(6), 519-528. https://doi.org/10.1016/j.jpsychores.2015.03.009
Korecki, J. R., Schwebel, F. J., Votaw, V. R., & Witkiewitz, K. (2020). Mindfulness-based programs for substance use disorders: a systematic review of manualized treatments. Substance Abuse Treatment, Prevention, and Policy, 15(1), 1-37. https://doi.org/10.1186/s13011-020-00293-3
Kriakous, S. A., Elliott, K. A., Lamers, C., & Owen, R. (2020). The Effectiveness of Mindfulness-Based Stress Reduction on the Psychological Functioning of Healthcare Professionals: a Systematic Review. Mindfulness, 12(1), 1-28. https://doi.org/10.1007/s12671-020-01500-9
Krishnan, A., Odejimi, O., Bertram, I., Chukowry, P. S., & Tadros, G. (2022). A systematic review of interventions aiming to improve newly-qualified doctors’ wellbeing in the United Kingdom. BMC Psychology, 10(1), 1-12. https://doi.org/10.1186/s40359-022-00868-8
Kumar, B., Shah, M. A. A., Kumari, R., Kumar, A., Kumar, J., & Tahir, A. (2019). Depression, Anxiety, and Stress Among Final-year Medical Students. Cureus, https://doi.org/10.7759/cureus.4257
Kunwar, D., Risal, A., & Koirala, S. (2016). Study of Depression, Anxiety and Stress among the Medical Students in two Medical Colleges of Nepal. Kathmandu University medical journal (KUMJ), 14(53), 22–26.
Kushwaha, R., Rauniar, G. P., Koirala, B., & Mandal, N. K. (2019). Prevalence of Substance Use among Undergraduate Students in a Medical College of Nepal. Journal of Nepal Medical Association, 57(219), https://doi.org/10.31729/jnma.4605
Kwok, J. Y. Y., Kwan, J. C. Y., Auyeung, M., Mok, V. C. T., Lau, C. K. Y., Choi, K. C., & Chan, H. Y. L. (2019). Effects of Mindfulness Yoga vs Stretching and Resistance Training Exercises on Anxiety and Depression for People With Parkinson Disease. JAMA Neurology, 76(7), 755-763. https://doi.org/10.1001/jamaneurol.2019.0534
Lemos-Santos, P., Blumrich, L., Debia, J. B., Castaldelli-Maia, J. M., Suen, P. J. C., & Malbergier, A. (2024). Drug use among medical students in São Paulo, Brazil: a cross-sectional study during the coronavirus disease 2019 pandemic. Sao Paulo Medical Journal, 142(2), https://doi.org/10.1590/1516-3180.2022.0493.r1.150623
Li, W., Howard, M. O., Garland, E. L., McGovern, P., & Lazar, M. (2017). Mindfulness treatment for substance misuse: A systematic review and meta-analysis. Journal of Substance Abuse Treatment, 75, 62-96. https://doi.org/10.1016/j.jsat.2017.01.008
Lomas, T., Medina, J. C., Ivtzan, I., Rupprecht, S., & Eiroa-Orosa, F. J. (2018). A Systematic Review and Meta-analysis of the Impact of Mindfulness-Based Interventions on the Well-Being of Healthcare Professionals. Mindfulness, 10(7), 1193-1216. https://doi.org/10.1007/s12671-018-1062-5
López Secanell, I., Gené Morales, J., & Hernaiz Agreda, N. (2021). Mindfulness y educación física en la población universitaria. Una revisión sistemática (Mindfulness and physical education in University population. A systematic review). Retos, 42, 821-830. https://doi.org/10.47197/retos.v42i0.86382
Marcon, G., Massaro Carneiro Monteiro, G., Ballester, P., Cassidy, R. M., Zimerman, A., Brunoni, A. R., von Diemen, L., Hauck, S., & Passos, I. C. (2020). Who attempts suicide among medical students?. Acta Psychiatrica Scandinavica, 141(3), 254-264. https://doi.org/10.1111/acps.13137
Martínez, D., Martínez, F. & Velázquez, A. (2018). Alcohol and tobacco consumption in first-year students of Medicine at the University of the Basque Country. Spanish journal of drug addiction, 43(1). https://dialnet.unirioja.es/servlet/articulo?codigo=6453627.
Meda, R., Herrero, M., Blanco-Donoso, L., Moreno-Jiménez, B. & Palomera, A. (2015). Psychometric properties of the five facet mindfulness questionnaire (five facet mindfulness questionnaire, FFMQ-M) in Mexico. Behavioral Psychology/Psicologia Conductual, 23(3). 467-487.
Molodynski, A., Lewis, T., Kadhum, M., Farrell, S. M., Lemtiri Chelieh, M., Falcão De Almeida, T., Masri, R., Kar, A., Volpe, U., Moir, F., Torales, J., Castaldelli-Maia, J. M., Chau, S. W. H., Wilkes, C., & Bhugra, D. (2020). Cultural variations in wellbeing, burnout and substance use amongst medical students in twelve countries. International Review of Psychiatry, 33(1-2), 37-42. https://doi.org/10.1080/09540261.2020.1738064
Nawi, A. M., Ismail, R., Ibrahim, F., Hassan, M. R., Manaf, M. R. A., Amit, N., Ibrahim, N., & Shafurdin, N. S. (2021). Risk and protective factors of drug abuse among adolescents: a systematic review. BMC Public Health, 21(1), https://doi.org/10.1186/s12889-021-11906-2
Newbury-Birch, D., White, M., & Kamali, F. (2000). Factors influencing alcohol and illicit drug use amongst medical students. Drug and Alcohol Dependence, 59(2), 125-130. https://doi.org/10.1016/s0376-8716(99)00108-8
Nogueira Pires, R., Mentz da Silva, W., Granemann Piola da Silva, R. G., Ribeiro Rossi, E., Moraes Marques, C., Meister Coelho, I. C., & Guetter Mello, R. (2022). Evaluación de intervenciones que promueven la calidad de vida de los estudiantes de medicina: una revisión sistemática.Revista Española de Educación Médica, 3(2), https://doi.org/10.6018/edumed.514541
Nosratabadi, M. & Halvaiepour, Z. (2019). Psychological determinants of drug abuse among male adolescents in Isfahan: A structural model. International Journal of Preventive Medicine, 10(27). https://doi.org/10.4103/ijpvm.IJPVM_23_17.
Nyanaponika, T. (1962). The heart of Buddhist meditation: A handbook of mental training based on the Buddha’s way of mindfulness. London Rider & Company.
Oró, P., Esquerda, M., Mas, B., Viñas, J., Yuguero, O., & Pifarré, J. (2021). Effectiveness of a Mindfulness-Based Programme on Perceived Stress, Psychopathological Symptomatology and Burnout in Medical Students. Mindfulness, 12(5), 1138-1147. https://doi.org/10.1007/s12671-020-01582-5
Peláez Lopez, M. A., Lozano Zuluaga, J. J., Narváez Andrade, M. J., & Becerra Hernández, L. V. (2021). El cerebro del meditador de atención plena: de la prospección a la tarea. Universitas Médica, 62(4), https://doi.org/10.11144/javeriana.umed62-4.brai
Piñel, C., Gómez-Roso, M. & López, J. (2021). Percepción y ansiedad de los estudiantes de Medicina en su rotación clínica en Obstetricia durante la pandemia por COVID-19. Revista Española de Educación Médica 2(1):13-21 https://doi.org/10.6018/edumed.460561
Polle, E., & Gair, J. (2021). Mindfulness-based stress reduction for medical students: a narrative review. Canadian Medical Education Journal, https://doi.org/10.36834/cmej.68406
Puig-Nolasco, A., Cortaza-Ramirez, L., & Cristina Pillon, S. (2011). Consumo de alcohol entre estudiantes Mexicanos de medicina. Revista Latino-Americana de Enfermagem, 19(spe), 714-721. https://doi.org/10.1590/s0104-11692011000700008
Robles, R., Varela, R., Jurado, S. & Páez, F. (2001). The Mexican version of Beck Anxiety Inventory: Psychometric properties. Revista Mexicana de Psicología, 18(2), 211-218.
Ruiz-Fernández, M. D., Ortíz-Amo, R., Ortega-Galán, Á. M., Ibáñez-Masero, O., Rodríguez-Salvador, M. D. M., & Ramos-Pichardo, J. D. (2019). Mindfulness therapies on health professionals. International Journal of Mental Health Nursing, 29(2), 127-140. https://doi.org/10.1111/inm.12652
Santiago, S. & Urcuhuaranga, A. (2021). Effectiveness of an intervention program in mental disorders in university students of the Unheval medical school, 2019. Universidad Nacional Hermilio Valdizán, Published undergraduate thesis. https://hdl.handle.net/20.500.13080/6385.
Secretaría de Salud, (2020). 077. Se confirma en México caso importado de coronavirus COVID- 19. https://www.gob.mx/salud/prensa/077-se-confirma-en-mexico-caso-importado-de-coronavirus-covid-19
Sekhar, P., Tee, Q. X., Ashraf, G., Trinh, D., Shachar, J., Jiang, A., Hewitt, J., Green, S., & Turner, T. (2021). Mindfulness-based psychological interventions for improving mental well-being in medical students and junior doctors. Cochrane Database of Systematic Reviews, 2021(12), https://doi.org/10.1002/14651858.cd013740.pub2
Shao, R., He, P., Ling, B., Tan, L., Xu, L., Hou, Y., Kong, L., & Yang, Y. (2020). Prevalence of depression and anxiety and correlations between depression, anxiety, family functioning, social support and coping styles among Chinese medical students. BMC Psychology, 8(1), https://doi.org/10.1186/s40359-020-00402-8
Single, A., Bilevicius, E., Johnson, E. A., & Keough, M. T. (2019). Specific Facets of Trait Mindfulness Reduce Risk for Alcohol and Drug Use Among First-Year Undergraduate Students. Mindfulness, 10(7), 1269-1279. https://doi.org/10.1007/s12671-019-1092-7
Slavin, S. J., & Chibnall, J. T. (2016). Finding the Why, Changing the How: Improving the Mental Health of Medical Students, Residents, and Physicians. Academic Medicine, 91(9), 1194-1196. https://doi.org/10.1097/acm.0000000000001226
Sommet, A., Ferrières, N., Jaoul, V., Cadieux, L., Soulat, J., Lapeyre-Mestre, M., & Montastruc, J. (2012). Use of Drugs, Tobacco, Alcohol and Illicit Substances in a French Student Population. Therapies, 67(5), 429-435. https://doi.org/10.2515/therapie/2012056
Spinelli, C., Wisener, M., & Khoury, B. (2019). Mindfulness training for healthcare professionals and trainees: A meta-analysis of randomized controlled trials. Journal of Psychosomatic Research, 120, 29-38. https://doi.org/10.1016/j.jpsychores.2019.03.003
Steiner-Hofbauer, V., & Holzinger, A. (2020). How to Cope with the Challenges of Medical Education? Stress, Depression, and Coping in Undergraduate Medical Students. Academic Psychiatry, 44(4), 380-387. https://doi.org/10.1007/s40596-020-01193-1
Tanay, G., Lotan, G., & Bernstein, A. (2012). Salutary Proximal Processes and Distal Mood and Anxiety Vulnerability Outcomes of Mindfulness Training: A Pilot Preventive Intervention. Behavior Therapy, 43(3), 492-505. https://doi.org/10.1016/j.beth.2011.06.003
Tian-Ci Quek, T., Wai-San Tam, W., X. Tran, B., Zhang, M., Zhang, Z., Su-Hui Ho, C., & Chun-Man Ho, R. (2019). The Global Prevalence of Anxiety Among Medical Students: A Meta-Analysis. International Journal of Environmental Research and Public Health, 16(15), 2735. https://doi.org/10.3390/ijerph16152735
Tiburcio Sainz, M., Rosete-Mohedano, M. G., Natera Rey, G., Martínez Vélez, N. A., Carreño García, S., & Pérez Cisneros, D. (2016). Validity and Reliability of the Alcohol, Smoking, and Substance Involvement Screening Test (ASSIST) in University Students. Adicciones, 28(1), 19. https://doi.org/10.20882/adicciones.786
Vettese, L. C., Toneatto, T., Stea, J. N., Nguyen, L., & Wang, J. J. (2009). Do Mindfulness Meditation Participants Do Their Homework? And Does It Make a Difference? A Review of the Empirical Evidence. Journal of Cognitive Psychotherapy, 23(3), 198-225. https://doi.org/10.1891/0889-8391.23.3.198
Vásquez-Dextre, E. R. (2016). Mindfulness: Conceptos generales, psicoterapia y aplicaciones clínicas. Revista de Neuro-Psiquiatria, 79(1), 42. https://doi.org/10.20453/rnp.v79i1.2767
Wielgosz, J., Goldberg, S. B., Kral, T. R., Dunne, J. D., & Davidson, R. J. (2019). Mindfulness Meditation and Psychopathology. Annual Review of Clinical Psychology, 15(1), 285-316. https://doi.org/10.1146/annurev-clinpsy-021815-093423
Witt, K., Boland, A., Lamblin, M., McGorry, P. D., Veness, B., Cipriani, A., Hawton, K., Harvey, S., Christensen, H., & Robinson, J. (2019). Effectiveness of universal programmes for the prevention of suicidal ideation, behaviour and mental ill health in medical students: a systematic review and meta-analysis. Evidence Based Mental Health, 22(2), 84-90. https://doi.org/10.1136/ebmental-2019-300082
World Health Organization “WHO”. (2020). COVID-19: chronology of WHO action. https://www.who.int/es/news/item/27-04-2020-who-timeline---covid-19.
Wupperman, P., Burns, N., Pugach, C., & Edwards, E. (2019). Treatment for Individuals With Severe Mental Illness Who Use Illicit Drugs While Maintained on Methadone: Mindfulness and Modification Therapy. The Journal of Nervous and Mental Disease, 207(12), 1005-1011. doi:10.1097/NMD.0000000000001066.
Xie, J., Li, X., Luo, H., He, L., Bai, Y., Zheng, F., Zhang, L., Ma, J., Niu, Z., Qin, Y., Wang, L., Ma, W., Yu, H., Zhang, R., & Guo, Y. (2021). Depressive Symptoms, Sleep Quality and Diet During the 2019 Novel Coronavirus Epidemic in China: A Survey of Medical Students. Frontiers in Public Health, 8, https://doi.org/10.3389/fpubh.2020.588578
Zamboni, L., Centoni, F., Fusina, F., Mantovani, E., Rubino, F., Lugoboni, F., & Federico, A. (2021). The effectiveness of cognitive behavioral therapy techniques for the treatment of substance use disorders: a narrative review of evidence. The Journal of nervous andmental illness, 209(11), 835-845. https://doi.org/10.1097/NMD.0000000000001381.
Zemestani, M., & Fazeli Nikoo, Z. (2020). Effectiveness of mindfulness-based cognitive therapy for comorbid depression and anxiety in pregnancy: a randomized controlled trial. Archives of Women’s Mental Health, 23(2), 207-214. https://doi.org/10.1007/s00737-019-00962-8
Zeng, W., Chen, R., Wang, X., Zhang, Q., & Deng, W. (2019). Prevalence of mental health problems among medical students in China: A meta-analysis. Medicine, 98(18), e15337. https://doi.org/10.1097/md.0000000000015337
Zhang, B., Fu, W., Guo, Y., Chen, Y., Jiang, C., Li, X., & He, K. (2022). Effectiveness of mindfulness-based cognitive therapy against suicidal ideation in patients with depression: A systematic review and meta-analysis. Journal of Affective Disorders, 319, 655-662. https://doi.org/10.1016/j.jad.2022.09.091
Zúñiga, D., Torres-Sahli, M., Nitsche, P., Echeverría, G., Pedrals, N., Grassi, B., Cisternas, M., Rigotti, A., & Bitran, M. (2021). Reduced burnout and higher mindfulness in medical students after a self-care program during the COVID-19 pandemic. Revista médica de Chile, 149(6), 846-855. https://doi.org/10.4067/s0034-98872021000600846"> https://doi.org/10.4067/s0034-98872021000600846
Citation:
Ortiz Castro, A., Bernal Pérez, R. P., Vargas Huicochea, I., Farfán Márquez, A., Flores-Castro, J. C. (2025). Evaluation of a Brief Mindfulness-based Intervention to Prevent Problematic Substance Use among First-year Medical. Salud Mental, 48(1), 21-30. https://doi.org/10.17711/SM.0185-3325.2025.004