BACKGROUND
Although often overlooked or misinterpreted as mere sadness, depression is a multifaceted condition that manifests itself in various ways, affecting not only mood but also the physical health and daily functioning of afflicted individuals (Organización Panamericana de la Salud [OPS], 2017). Depression is not just a temporary state of sadness; it constitutes a persistent condition plunging those affected into a profound emotional abyss. It is often accompanied by feelings of hopelessness, loss of interest in previously pleasant activities, constant fatigue, difficulty concentrating, loss of appetite, disrupted sleep patterns, cognitive impairment, and feelings of worthlessness or guilt (American Psychiatric Association, 2016).
According to data provided by WHO in 2015, the prevalence of depression increased by 18.4% over ten years from 2005 to 2015. Current estimates suggest that nearly 322 million individuals worldwide suffer from depression. Its incidence is more pronounced among women than men, with a percentage difference of 1.5 %. Furthermore, depression manifests across all age groups, with a higher prevalence among women ages between 55 and 74 (OPS, 2017).
Treatment of depression includes psychotherapy and pharmacotherapy. The latter involves the use of antidepressant drugs, which work through various mechanisms of action, mainly regulating the monoaminergic system composed of the neurotransmitters serotonin (5HT), dopamine (DA), and norepinephrine (NA) (Pérez-Esparzaet al., 2017). However, although this pharmacological treatment is highly effective, there is a group of patients in whom remission is not achieved, indicating the need for further investigation of alternative or adjuvant treatments.
In recent years, the importance of the intestinal bacterial flora (microbiota) in both physical and mental health has been identified, finding that disruptions to this flora may be associated with various chronic diseases, including mental health disorders such as depression and anxiety (Hou et al., 2022; Kumar et al., 2023). Moreover, a spectrum of intrinsic factors linked to the host can compromise the integrity of the intestinal bacterial flora, which can lead to dysbiosis. Some of these factors are genetic factors, chronic or infectious diseases, lifestyle habits such as unhealthy dietary patterns (unbalanced, high sugar content, and low fiber), and poor hygiene habits. Extrinsically, environmental factors, including exposure to xenobiotics such as drugs (particularly antibiotics), food additives, and other substances, have also been identified as contributors to dysbiosis (Hrncir, 2022).dysbiosis (Hrncir, 2022).dysbiosis (Hrncir, 2022).dysbiosis (Hrncir, 2022).
In this respect, treating depression and other mental health disorders could go beyond standard psychotherapeutic and pharmacological modalities and include therapeutic alternatives that restore and/or boost intestinal bacterial flora, such as a dietary regimen abundant in fruits, leafy green vegetables, fish, and polyphenols. Concurrently, the consumption of beneficial microorganisms, known as probiotics, of substances that promote their growth (prebiotics), or a combination of both (symbiotics), stands as a pertinent adjunct to these therapeutic strategies (Kumar et al., 2023).
Probiotics, found naturally in our digestive system and considered an essential part of the gut microbiota, may also be supplemented by specific live microorganisms that, when ingested as nutritional supplements, adapt to the intestinal environment, conferring benefits similar to naturally occurring probiotics. Conversely, prebiotics are selectively fermentable ingredients that cause specific changes in the composition and/or activity of the gastrointestinal microbiota (Sarkar et al., 2016). Finally, symbiotics are selective formulations of probiotics and prebiotics.
The mechanism of action of probiotics is an extraordinary process owing to their multifaceted beneficial effects. These encompass the establishment of eubiosis within the intestinal microbiota, helping the host metabolism through immune system stimulation, inflammation regulation, and the production of metabolites, including short-chain fatty acids and neurotransmitters (Sikorska et al., 2023). A specific category within probiotics is psychobiotics, live microorganisms affording health benefits to individuals with mental illness when ingested in adequate doses. This is achieved through the production of neurotransmitters or their precursors, thereby influencing the microbiota-gut-brain axis (MGB) and modulating the hypothalamic-pituitary-adrenal (HPA) axis, consequently decreasing its activity. As such, certain probiotics may have positive effects on mood and cognitive function by modulating the gut microbiota and improving gut-brain communication (Dinan et al., 2013; Sikorska et al., 2023).
Several studies and systematic reviews have recently been published on the efficacy of probiotics, prebiotics, and/or symbiotics addressing depressive symptomatology or depression. This paper aims to present a meta-review outlining and summarizes the main findings in methodologically rigorous systematic reviews.
In regard to specific objectives, this meta-review seeks to describe the characteristics of published systematic reviews with quantitative synthesis, exploring subpopulations (classified by age group and health conditions) and treatment modalities (classified by length of treatment, monotherapy and add-on therapy), in which the effectiveness of probiotics, prebiotics, and symbiotics have been tested, to compare the efficacy between these different subpopulations and treatment modalities.
METHOD
A systematic review of systematic reviews — also known as a “meta-review” or “umbrella review” — (Aromataris et al., 2015; Smith et al., 2011) was conducted to analyze the efficacy of interventions based on probiotic, prebiotic, or symbiotic treatment for the management of depressive symptomatology and/or depression. A team comprising the six co-authors worked on the review. A review protocol was registered with the Research Registry platform and the identifying number was review registry1817 (Anguiano-Morán et al., 2024). A research question was formulated based on the identification of the components of the PICO strategy (population, intervention, comparison, and outcomes): P = healthy individuals with depressive symptomatology or diagnosed depression at various stages of evolution; I = treatment with probiotics, prebiotics, or symbiotics either as monotherapy or adjunctively to pharmacological treatment; C = administration of a placebo and/or standard pharmacological treatment; and O = evaluation of depression levels through self-reporting using psychometric depression scales. Only systematic reviews of Randomized Controlled Trials (RCT) reporting quantitative data synthesis (meta-analysis) were considered.
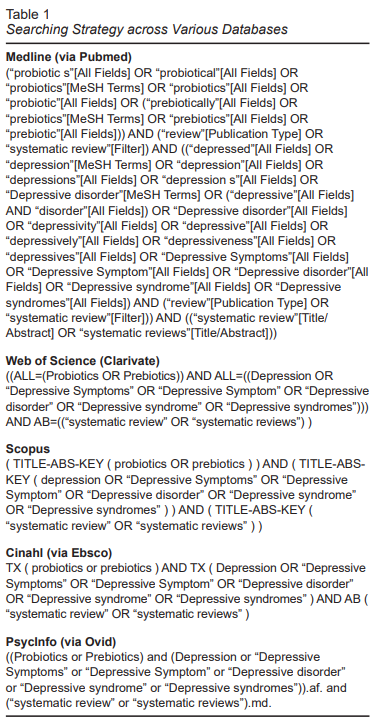
The research involved searches across databases such as Medline (via PubMed), Web of Science, Scopus, Cinahl (via Ebsco), and PsycInfo (via Ovid), using keywords and Boolean operators. The specific search strategies for each database consulted are detailed in Table 1.
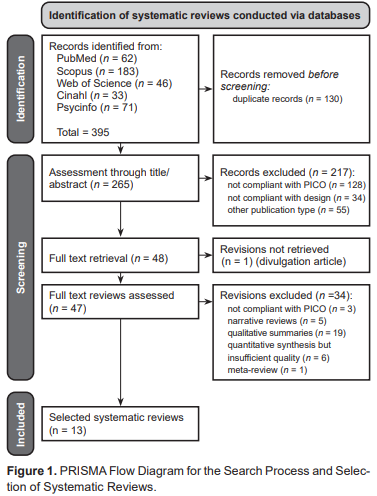
The Zotero bibliographic manager was used to manage the reference database and identify duplicate reviews, while the Rayyan online system was used to select studies through title and abstract by two reviewers. Inclusion criteria comprised having all the elements of the PICO strategy and publication in either English or Spanish. The full texts of the reviews selected through this process were acquired and analyzed by other two reviewers who carried out a painstaking selection considering the previous criteria, in addition to whether they included quantitative synthesis, and fulfilled certain quality considerations. A PRISMA flow diagram (Page et al., 2021) was generated to illustrate the search, screening, and article inclusion processes (Figure 1).
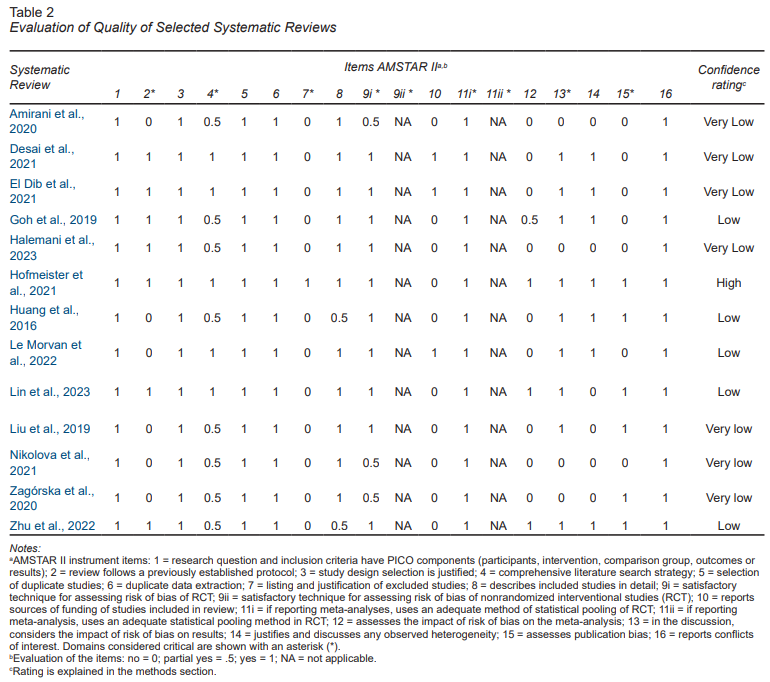
The quality of the selected reviews was assessed through the AMSTAR II instrument, which contains seven critical domains and nine non-critical domains. For each item, the answer could be “yes,” “no,” or “partly so.” According to this instrument, overall confidence of the systematic reviews can be rated as the following: 1) “High,” for no or one non-critical weakness; 2) “Moderate,” for two or more non-critical weaknesses; 3) “Low,” for one critical flaw with or without a non-critical weakness; and 4) “Very low,” for two or more critical flaw with or without non-critical weakness (Shea et al., 2017).
Data extraction for the characteristics of the selected systematic reviews included study populations, interventions, comparators, and outcomes, participants enrolled in the studies, and the main outcomes obtained, both overall and by subgroup. Information on the heterogeneity reported as the I2 statistic for overall and subgroup meta-analyses was also collected. According to this index, heterogeneity of effect estimates across trials can be described as small (I2 < 25%), moderate (I2 between 26 and 74%), or substantial (I2 ≥ 75%) (Higgins et al., 2003). Additionally, data on the risk of bias assessment reported in the systematic reviews was collected.
RESULTS
Flowchart
The diagram in Figure 1 shows the systematic review search and selection process. After the review process, 13 quantitative systematic reviews (meta-analyses) were selected.
Quality Analysis of Selected Systematic Reviews
Table 2 shows the quality analysis of the selected systematic reviews. Most systematic reviews had unsatisfactory results, with confidence being rated as “Low” or “Very low” and only one achieving a “High” (Hofmeister et al., 2021). In regard to the results for the critical items, some reviews did not report having a protocol registry before the review (item 2), others did not report the search strategies clearly (item 4), most failed to report the studies excluded or their justification for this (item 7), and still others did not provide a detailed discussion of the impact of the risk of bias in the selected studies on the findings (item 13), with several failing to report publication bias (item 15). The low frequency of compliance with item 7 was particularly striking; only one review reported the list of studies excluded and their justification (Hofmeister et al., 2021). Failure to comply with this item affected the overall results of the other reviews.
Characteristics of the Systematic Reviews Selected
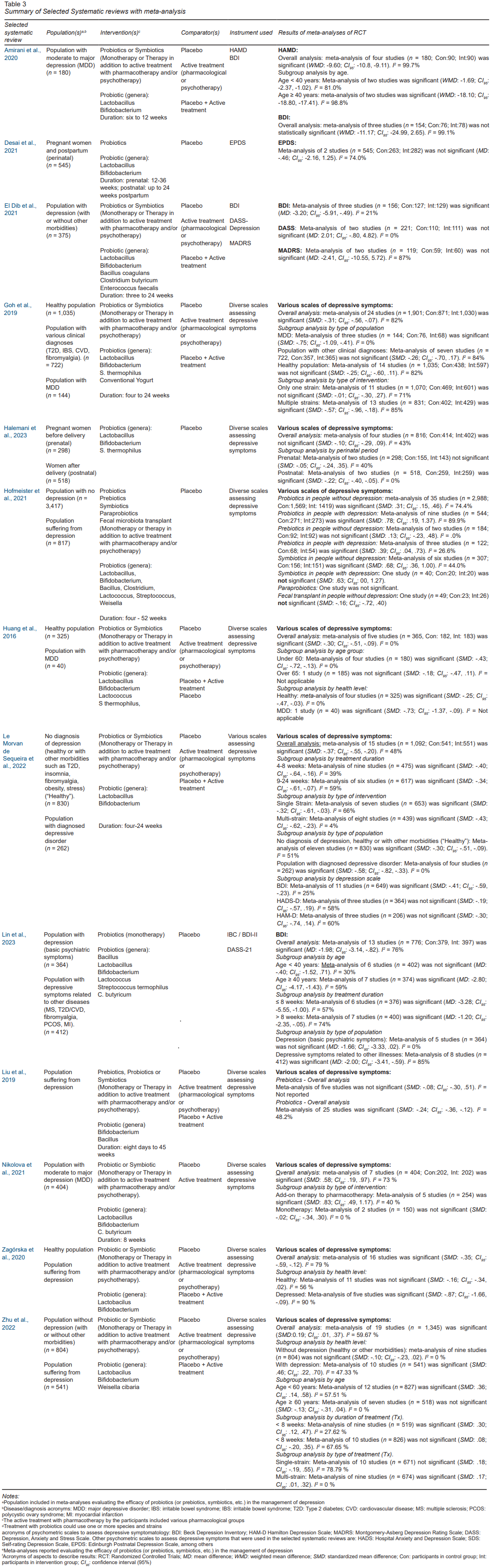
Table 3 outlines the general characteristics and main results of the systematic reviews selected. In regard to the population of interest, these reviews included individuals with depressive symptomatology or a depressed population at various stages with or without other comorbidities. In regard to the intervention, most of the systematic reviews evaluated the efficacy of probiotics, although some also included the evaluation of prebiotics, symbiotics, and even paraprobiotics. These systematic reviews included studies using probiotics as monotherapy or adjunctive interventions to pharmacological treatment. Furthermore, the intervention encompassed both single and multiple strain therapies. Placebos or standard pharmacological treatment, whether separately or combined, were used as comparators. Depressive symptomatology was assessed using various psychometric scales.
Meta-analyses, as reported in these systematic reviews, evaluated effect size using metrics such as weighted mean difference (WMD), mean difference (MD), or standardized mean difference (SMD). Some systematic reviews opted for meta-analyses using various depression assessment scales (Amirani et al., 2020; El Dib et al., 2021) and intervention types (Liu et al., 2019), a combination of intervention types and populations (Hofmeister et al., 2021), or specific subpopulations (Desai et al., 2021). However, most systematic reviews involved an overall meta-analysis with subgroup analysis, explaining the factors influencing efficacy (Goh et al., 2019; Halemani et al., 2023; Huang et al., 2016; Le Morvan de Sequeira et al., 2022; Lin et al., 2023; Nikolova et al., 2021; Zagórska et al., 2020; Zhu et al., 2022).
Efficacy of Probiotics
The assessment of probiotic efficacy was examined across 13 selected systematic reviews, focusing on the treatment of depressive symptomatology and depression itself.
Within the healthy population, probiotic efficacy was evaluated in three reviews (Goh et al., 2019; Huang et al., 2016; Zagórska et al., 2020). Only Huang et al. (2016)demonstrated a statistically significant meta-analysis from four studies (n = 325, SMD: -.25; CI95%: -.47, -.03).
Five reviews evaluated probiotic efficacy in populations with depressive symptomatology, predominantly associated with chronic diseases (Goh et al., 2019; Hofmeister et al., 2021; Le Morvan de Sequeira et al., 2022; Lin et al., 2023; Zhu et al., 2022). Statistically significant meta-analyses were observed in three reviews: 1) Hofmeister et al. (2021)with 35 studies (n =2,988,SMD: .31;CI95%: .15, .46); 2)Le Morvan de Sequeira et al., (2022) with 11 studies (n = 830, SMD: -.30; CI95%: -.51, -.09); and 3) and Lin et al. (2023) with eight studies (n = 412, SMD: -2.00; CI95%: -3.41, -.59).
Eight systematic reviews found statistical significance in populations diagnosed with varying stages of depression that involved probiotic treatment as monotherapy or as an adjunct intervention to pharmacological treatment (Amirani et al., 2020; El Dib et al., 2021; Hofmeister et al., 2021; Le Morvan de Sequeira et al., 2022; Liu et al., 2019; Nikolova et al., 2021; Zagórska et al., 2020; Zhu et al., 2022). Some of the most outstanding reviews, such as Hofmeister et al. (2021) with nine studies (n = 544, SMD: .78; CI95%: .19, 1.37); Zhu et al. (2022) with ten studies (n = 541, SMD: .46; CI95%: .22, .70); and Liu et al. with 25 studies (SMD: -.24; CI95%: -.36, -.12), had substantial sample sizes. Two reviews evaluated probiotic efficacy in monotherapy (Lin et al., 2023; Nikolova et al., 2021) yet reported no statistically significant differences compared to the placebo in their meta-analyses.
In the population with major depressive disorder (MDD), probiotic efficacy was evaluated through a subgroup analysis as part of a systematic review (Goh et al., 2019) including three studies, and was statistically significant (n = 144, SMD: -.75; CI95%: -1.09, -.41). Another review (Huang et al., 2016) included one study focusing on this population, which was statistically significant (n = 40, SMD: -.73; CI95%: -1.37, -.09).
Regarding the analysis of probiotic efficacy across various age categories, four reviews implemented subgroup analyses within their meta-analyses (Amirani et al., 2020; Huang et al., 2016; Lin et al., 2023; Zhu et al., 2022). Two reviews established 40 years as the threshold, creating two age groups (< 40 years and ≥ 40 years): 1) Amirani et al. (2020) included studies involving patients with depression and found statistically significant evidence in both age groups, while 2) Lin et al. (2023)included patients with depressive symptomatology and depression, only finding statistically significant evidence in the ≥ 40 years old age group. The remaining two reviews (Huang et al., 2016 and Zhu et al., 2022) established 60 years as the threshold, creating two age groups (< 60 years and ≥ 60 years). both reviews only found statistically significant evidence in the age group of 60 years old.
Additional subgroup analyses considered factors that could influence probiotic treatment efficacy, including the number of strains in the formulation and treatment duration. Regarding the number of strains, three reviews categorized two treatment types: one strain and two or more strains (multi-strain) (Goh et al., 2019; Le Morvan de Sequeira et al., 2022; Zhu et al., 2022). Statistically significant evidence for one-strain treatment was found in Le Morvan de Sequeira et al., 2022, while all three reviews reported statistically significant evidence for multi-strain treatment.
Three reviews analyzed treatment duration (Le Morvan de Sequeira et al., 2022; Lin et al., 2023; Zhu et al., 2022) and established an eight-week threshold, creating two groups with different durations (< 8 weeks and ≥ 8 weeks). while each review found statistically significant evidence for the < 8-week duration group, only two reported statistically significant evidence for the ≥ 8-week duration group (Le Morvan de Sequeira et al., 2022; Lin et al., 2023).
Two reviews evaluated probiotic efficiency in pregnant women with perinatal depressive symptomatology or depression (Desai et al., 2021; Halemani et al., 2023). Desai et al. (2021)collectively evaluated probiotic efficacy in perinatal depression (prenatal and postnatal), with no statistically significant differences being found from the comparison group. However, Halemaniet al. (2023) found no statistically significant evidence in a subgroup analysis of two prenatal studies although they did find statistically significant evidence in two postnatal studies (n = 518, SMD: -.22; CI95%: -.40, -.05).
Efficacy of Prebiotics
Prebiotic efficacy was assessed in two reviews (Hofmeister et al., 2021; Liu et al., 2019). Liu’s review found no evidence of statistically significant efficacy, whereas Hofmeister found evidence of probiotic efficacy in individuals with depression in a meta-analysis of three studies (n = 122, SMD: .39; CI95%: 04, .73).
Efficacy of Symbiotics
The efficacy of symbiotics has only formally been evaluated by Hofmeister et al., 2021. This review reported evidence of statistically significant efficacy in individuals without depression through a meta-analysis of six studies (n = 307, SMD: .68; CI95%: .36, 1.00).
Efficacy of Paraprobiotics
One systematic review formally evaluated the efficacy of paraprobiotics (Hofmeister et al., 2021). However, the authors only included one study that reported no evidence of statistically significant efficacy.
Risk of Bias and Heterogeneity assessments
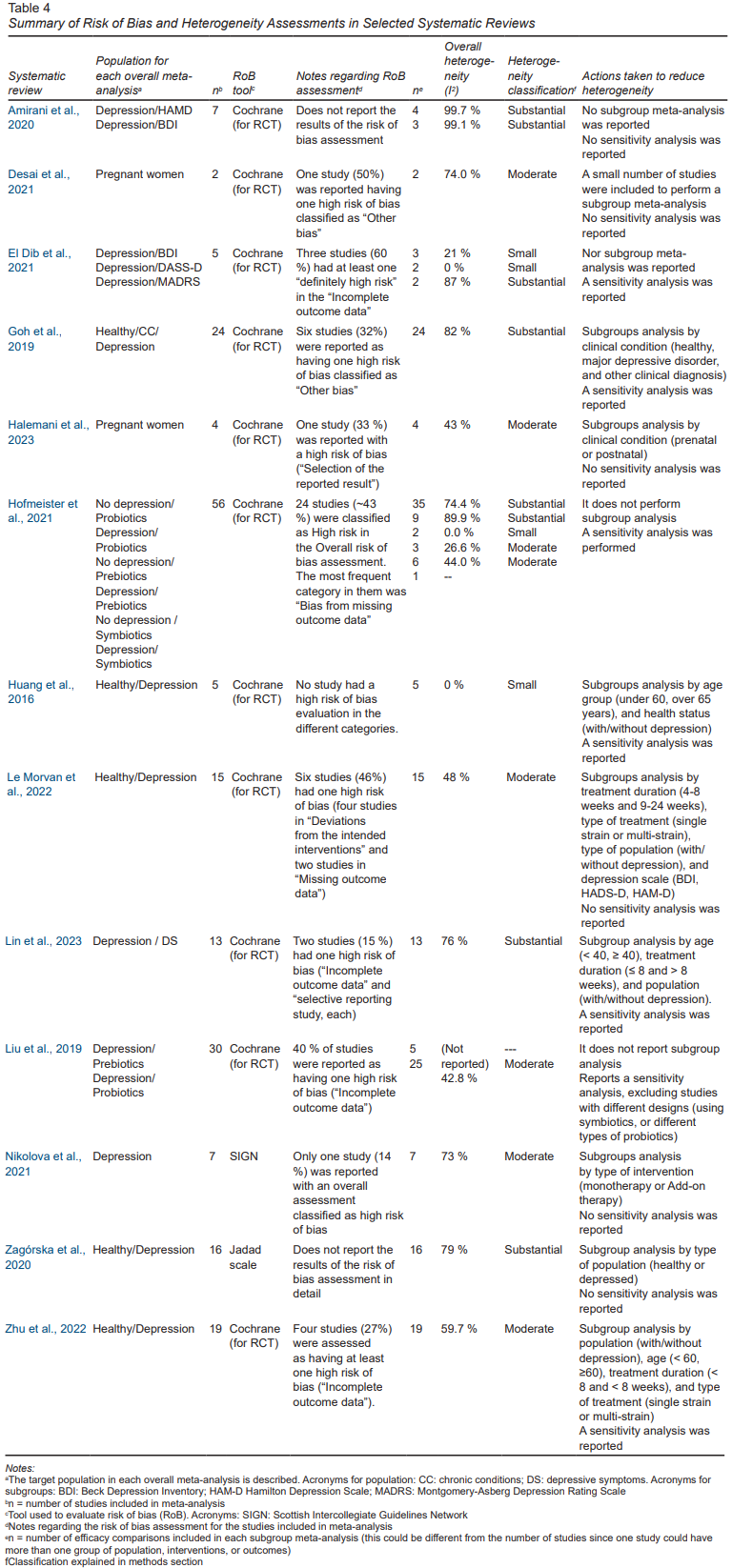
Table 4 summarizes information on the population included in the studies of the selected systematic reviews, the number of studies included, the risk of bias assessment, as well as the heterogeneity assessment (I2) for the reported overall meta-analyses, as well as the actions undertaken to reduce this heterogeneity.
Concerning the risk of bias analysis, the vast majority of reviews (11) reported the results in detail, only two reviews did not (Amirani et al., 2020; Zagórska et al., 2020). The majority (10) of these 11 reviews that did present the details of the analysis reported at least one study that was evaluated as having a “high risk of bias” in one of the evaluation categories. The evaluation category in which the highest frequency of evaluations with “high risk of bias” was usually reported was “Incomplete outcome data” (attrition bias).
In regard to the evaluation of heterogeneity, out of a total of 20 overall meta-analyses reported in the 13 selected systematic reviews, three (15%) overall meta-analyses reported “low” heterogeneity, eight (40%) overall meta-analyses reported “Moderate” heterogeneity, and seven (35%) overall meta-analyses reported “Substantial” heterogeneity. This high frequency of substantial heterogeneity could be because most of the reviews included studies with populations of different groups (with a variety of age categories and health conditions such as healthy, diagnosed with chronic diseases and varying levels of depression). They also included different treatment modalities (prebiotic, probiotic or symbiotic, of various durations, single-strain/multi-strain, monotherapy/add-on therapy). Most reviews performed subgroup analyses that may have decreased the overall heterogeneity, as shown in the I2 reported for subgroup meta-analyses (Table 3). In addition, some studies performed sensitivity analyses to exclude studies that could affect heterogeneity or had a risk of bias issues.
DISCUSSION AND CONCLUSION
The present meta-review offers a comprehensive overview of systematic reviews investigating the efficacy of probiotics, prebiotics, and symbiotics to improve depressive symptoms across diverse depression levels and age groups. It is the first meta-review to synthesize key findings from recent systematic reviews of this issue.
Thirteen systematic reviews exploring probiotics as an alternative approach to alleviating depressive symptoms were included. Most of these systematic reviews were rated as poor. Some of the factors contributing to this result were the absence of protocol registration, insufficient clarity in reporting the studies excluded and funding sources, and lack of sensitivity analysis concerning the risk of bias.
Main findings
In general terms, the meta-review found evidence confirming the efficacy of prebiotics, probiotics, or symbiotics in addressing depressive symptomatology or diagnosed depression across varying clinical stages. As expected, reviews that included studies involving healthy individuals showed non-statistically significant evidence of treatment efficacy or minimal effect sizes (evaluated as MD or SMD).
Prebiotics efficacy was only demonstrated in one systematic review, specifically in a meta-analysis for the population with depression, with statistically significant evidence being obtained, except in one meta-analysis for people without depression (Hofmeister et al., 2021). No statistically significant evidence was found in another review for the use of prebiotics (Liu et al., 2019).
Stronger evidence of probiotic efficacy was found in almost all the selected systematic reviews, characterized by statistically significant hypothesis tests in the meta-analyses. However, effect sizes were low: WMD = -9.60 (Amirani et al., 2020); MD ranging from -3.2 to -1.98 (Desai et al., 2021; El Dib et al., 2021; Lin et al., 2023); and SMD ranging from .19 to .78 (Goh et al., 2019; Halemani et al., 2023; Huang et al., 2016; Hofmeister et al., 2021; Le Morvan de Sequeira et al., 2022; Liu et al., 2019; Nikolova et al., 2021; Zagórska et al., 2020; Zhu et al., 2022). These effect sizes may vary depending on factors such as demographic composition (age group, pregnancy), severity of depression (healthy population, those with depressive symptoms, or diagnosed depression), formulation type (single strain or multi-strain), treatment duration, and treatment modality (adjunctive or monotherapy).
Some reviews found greater efficacy of probiotics compared to prebiotics, as evidenced by hypothesis testing and effect sizes (Hofmeister et al., 2021; Liu et al., 2019). For instance, higher effect size for probiotics compared to prebiotics in the population with depression was reported in one review (SMD = .31 and .13, respectively) (Hofmeister et al., 2021).
In regard to symbiotics, a review found statistically significant evidence supporting their efficacy, even when implemented in a population without diagnosed depression. This suggests that the combined use of probiotics and prebiotics could yield an additive effect, despite one study conducted in individuals with depression revealing a non-statistically significant difference. However, an analysis of the effect size obtained in the meta-analysis of symbiotics in a healthy population (SMD = .68) found that it exceeded those obtained for probiotics or prebiotics (SMD = .31 and .13, respectively) (Hofmeister et al., 2021). Moreover, it is worth noting that some meta-analyses conducted for probiotics included studies using symbiotics, as they incorporated prebiotic substances in their formulation.
Significantly, a specific review conducted a subgroup analysis to compare the efficacy of probiotics or symbiotics as monotherapy or as adjunctive therapy to pharmacological treatment. The analysis found a statistically significant effect in the latter group only, with a substantially higher effect size (SMD = .83 and -.02, respectively), although the monotherapy subgroup comprised only two studies (Nikolova et al., 2021).
Moreover, the efficacy of probiotics or symbiotics in the treatment of depression appears to be greater when formulations include multiple species, as noted in two systematic reviews (Goh et al., 2019; Le Morvan de Sequeira et al., 2022; Zhu et al., 2022). Additionally, optimal efficacy may be achieved within the initial eight weeks of treatment, although a favorable impact could persist beyond this timeframe (Le Morvan de Sequeira et al., 2022; Lin et al., 2023). Only one review contradicted this pattern, but it included studies involving a healthy population, potentially resulting in less visible effects of adjunctive therapy with probiotics or symbiotics (Zhu et al., 2022).
Moreover, systematic reviews revealed that the efficacy of probiotics or symbiotics in treating depression could be more pronounced in subjects over 40, as demonstrated by subgroup analyses within meta-analyses exclusively involving a population with depressive symptomatology or depression (Amirani et al., 2020; Lin et al., 2023). It is striking that other meta-analyses presenting a contrasting result included a population without depressive symptomatology or diagnosed depression, potentially making the impact of probiotic or symbiotic use less obvious (Huang et al., 2016; Zhu et al., 2022).
It should be noted that none of the selected reviews conducted subgroup analyses for children and adolescents, indicating limited evidence regarding the efficacy of these interventions in these age groups. In addition, subgroup analyses for older adults were only undertaken in two reviews, although depression assessment scales specific to this age group were not used (Huang et al., 2016; Zhu et al., 2022).
Another significant observation is that some reviews conducted special meta-analyses or subgroup analyses for certain specific depression assessment scales, obtaining similar results. Reviews using the Beck Depression Inventory (BDI) scores yield statistically significant evidence (El Dib et al., 2021; Le Morvan de Sequeira et al., 2022; Lin et al., 2023), except for one review that enrolled patients diagnosed with major depressive disorders, although the effect size was large (assessed using WMD) (Amirani et al., 2020).Conversely, a review using the Hamilton Depression Scale (HAMD) obtained statistically significant findings involving studies with a population exhibiting moderate to major depression (Amirani et al., 2020), while another review using this scale and comprising a population without a diagnosis of depression failed to yield statistically significant results (Le Morvan de Sequeira et al., 2022). However, as mentioned earlier, this could be because in this group of individuals, it might be more difficult to identify improvements in depressive symptoms.
Other psychometric depression scales, such as the Depression, Anxiety and Stress Scale (DASS), Montgomery-Asberg Depression Rating Scale (MADRS), and Hospital Anxiety and Depression Scale (HADS-D), underwent meta-analyses or specific subgroup analyses, yielding no statistically significant results (El Dib et al., 2021; Le Morvan de Sequeira et al., 2022). This underscores the potential variability in the performance of different scales in assessing depressive symptomatology, meaning that it would be important to analyze their documented history of validity and reliability.
Implications for Clinical Practice and Research
In terms of clinical practice, it is worth considering recommending an alternative use of probiotics or symbiotics as adjuvant or complementary approaches to conventional pharmacological treatments to relieve depressive symptomatology. This could have numerous implications for health systems, such as the incorporation of these treatments into formularies and clinical practice guidelines for managing depression. Additionally, proactive interventions for their implementation should be initiated to enhance prescription and utilization.
Research opportunities identified through this review include the following: 1) investigating the efficacy of probiotics, prebiotics, and symbiotics in specific age groups with limited evidence, such as children, adolescents, and older adults, which could require special psychometric instruments to assess depressive symptomatology in these groups; 2) exploring the efficacy of these interventions over a prolonged period of time(beyond six months); 3) conducting meta-analyses of efficacy for particular probiotic species or particular probiotic species combinations; 4) establishing and evaluating treatment protocols to determine optimal doses, types, and durations of probiotic, prebiotic, and symbiotic consumption; 5) assessing the safety profiles and potential adverse reactions associated with short- and long-term consumption; and 6) studying the efficacy of these treatments in preventing depression, especially in populations prone to this disease (with the exception of pregnant women).
Strengths and limitations
Several strengths were identified in the present meta-review: 1) A systematic search was conducted across diverse databases; 2) Numerous systematic reviews on the topic of interest were found in the literature, leading to a meta-review approach; 3) Only systematic reviews with meta-analysis were included, ensuring that conclusions are based on the quantitative synthesis of at least two studies; 4) An evaluation of the quality of the reviews included in the meta-review was undertaken.
However, certain limitations were acknowledged within this meta-review. The research question was limited to Patient Reported Outcomes (PROs) as outcomes. However, other potential results, such as biochemical markers and the frequency of adverse events, could be explored.
Conclusions
In this meta-review, after the synthesis of several published meta-analyses, it was found that probiotic or symbiotic consumption tends to improve depressive symptoms, as borne out by comparing results with depression assessment scales. However, there are certain limitations on available evidence, especially for particular age groups (such as children, adolescents, and older adults), as well as specific efficacy analyses for particular species and combinations, among other research opportunities discussed earlier.