INTRODUCTION
Coronavirus disease (COVID-19) forced people and groups worldwide to be more responsible after the World Health Organization (WHO) declared it a pandemic. Unprecedented restrictions were imposed to prevent transmission of the disease throughout communities and control the number of cases. In addition, a number of socially isolating policies were implemented, including the closure of gyms, nursing homes, schools, and universities as well as restrictions on mobility in the most severely affected areas (Romero-Blanco et al., 2020). In addition to measures such as lockdown, weekend curfews, and the closure of social areas such as restaurants, cafeterias, and gyms, business and education models changed, and working from home and online education were implemented (Birmingham et al., 2021) This process, which dramatically affected daily life, negatively impacted both physical and mental health (Timurtaş et al., 2022). The main COVID-19 effects on mental health include stress, worry, fear, depressive symptoms, and sleep disturbance (Rana et al., 2020; Restubog et al., 2020; Shigemura et al., 2020; Xiao et al., 2020).
Among the general population, sleep problems are relatively common and significantly linked to morbidity and mortality (Grandner et al., 2017). It is estimated that over 60% of university students experience poor sleep quality on a regular basis (Lund et al., 2010). During the pandemic, people were reported to be extremely stressed, anxious, and afraid after seeing videos, reading news stories, and watching TV shows on COVID-19. This made it difficult for them to fall asleep and altered their sleep habits (Savitsky et al., 2020). It has also been observed that intensive smart phone and Internet use has adversely affected the circadian rhythm, causing insomnia and other sleep disorders. One study found that changing sleep patterns in health education students leads to poor performance, behavioral modifications, and dietary changes (Tahir et al., 2021). According to several studies, students under stress are more likely to experience health issues, depression, and sleep disorders, negatively affecting their academic performance and quality of life (Köktürk et al., 2021; Sharififard et al., 2020; Shigemura et al., 2020; Silva, et al., 2020; Timurtaş et al., 2022).
Physical activity plays a pivotal role in health. Several studies have confirmed that physical activity levels affect mood and well-being (Kosendiak et al., 2022; Lin et al., 2020; Zhang et al., 2020). Among healthy people, physical activity and exercise have been linked to better sleep quality and fewer sleep disruptions. Work-related behaviors, lifestyles, and leisure activities have changed as a result of the pandemic. During the COVID-19 lockdowns, people began spending more time at home, contributing to a sedentary lifestyle and increasing the time spent sitting. During this period, a significant decrease in physical activity levels was observed in students. The closure of swimming pools, gyms, and fitness centers limited students’ access to physical activity, causing them to become almost completely sedentary (Kosendiak et al., 2022).
The research questions to be addressed within the scope of the study are as follows:
What is the level of physical activity in young adults?
What is the sleep quality level in young adults?
What factors affect how well young people sleep and how much they exercise?
Is there a link between how active young people are and how well they sleep?
METHOD
Study design
The study has a descriptive, correlational, cross-sectional design. It was planned and reported in accordance with STROBE (Strengthening the Reporting of Observational Studies in Epidemiology), a checklist for registering descriptive studies.
Participants
This study was conducted at the Vocational School of Health Services of a university in the Central Anatolia Region of Turkey between April and July 2022. This institution offers a two-year, four-semester associate degree, completed with a total of 120 European Credit Transfer System (ECTS) credits. The target universe of the study comprises first- and second-year students (n = 1800) studying in the departments of Operating Room Services, Medical Imaging, Medical Laboratory Techniques, First and Emergency Aid, Anesthesia, Eldercare, Physiotherapy, Dialysis, Audiometry, and Child Development, enrolled at this institution during the 2021-2022 academic year. According to Cohen’s sample size calculation formula for known target populations, the minimum number of participants was calculated as 485, with a 99% confidence interval and a 5% margin of error (α = .05 table value 1.96) (Daniel & Cross, 2018). The sample was obtained using the random sampling method. Invitations to participate in the study were sent to randomly selected students from each department from the official university e-mail address, and students were also invited to participate through class announcements. A participation rate of approximately 37.2% was achieved with 670 students who agreed to participate in the study.
Inclusion Criteria
Being currently enrolled as an active student at the university.
Being between the ages of 18 and 25.
Voluntarily agreeing to participate in the study and provide informed consent.
Having good overall health at the time of enrollment in the study, with no known chronic diseases, serious health conditions or acute medical problems.
Exclusion Criteria
Declining to participate in the study.
Presence of a severe health condition (chronic diseases such as diabetes, cardiovascular diseases, cancer, or neurological disorders) that could significantly affect participation in the study or interfere with the study.
Having a physical or mental health issue, including acute illnesses, mental health disorders (such as depression or anxiety), or personal issues that could affect the ability to comply with the study requirements, such as attending study sessions or completing surveys.
Pregnancy or any other condition that may involve specific medical risks or restrictions during the study period.
Data Collection and Instruments
During the study period, data were collected using the Introductory Information Form, Pittsburgh Sleep Quality Index (PSQI), and International Physical Activity Questionnaire- Short Form (IPAQ-SF).
Introductory Information Form
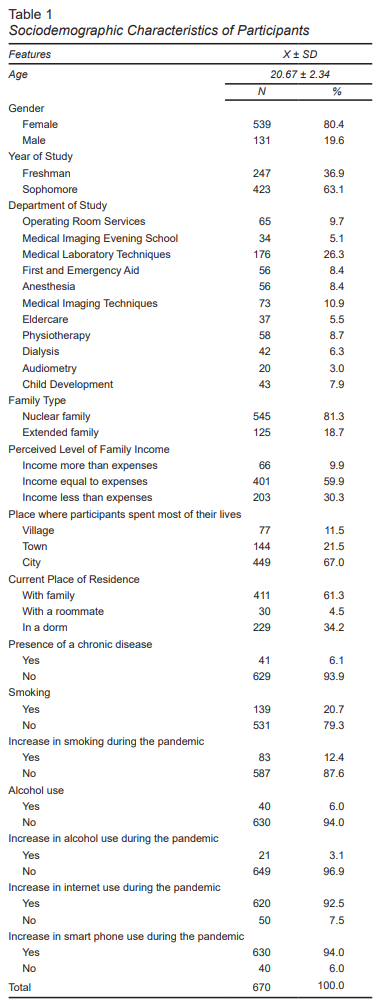
This form, prepared in line with the literature, comprises questions regarding the sociodemographic characteristics of the students participating in the study. The form comprises 15 questions including factors such as participants’ age, area of study, year of study, family structure, perceived income status, the place where they spend most of their lives, current place of residence, smoking status, alcohol use, increase in smoking, alcohol use, internet and smartphone use during the pandemic period, and presence of chronic diseases (Köktürk et al., 2021; Romero-Blanco et al., 2020; Silva et al., 2020).
PSQI
PSQI is a self-rate questionnaire providing information on sleep quality and the type and severity of sleep disturbances over a one-month period. The 18 items in the index make it possible to assess the parameters affecting sleep quality, sleep duration, sleep latency, and the frequency and severity of sleep-related problems. Items are grouped into seven components (subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction). Each item in the scale is rated with a score between 0 (no disturbance) and 3 (severe disturbance). The sum of the scores for the seven components yields the total PSQI score. The score for each component ranges from 0 to 3, with the total PSQI score ranging from 0 to 21. A total score of 5 or less indicates good sleep quality. The Turkish validity and reliability study of the scale was conducted by Agargün et al., and the Cronbach’s alpha was reported as .80 (Agargun, 1996; Buysse et al., 1989).
IPAQ-SF
The IPAQ-SF was used to assess participants’ physical activity levels. This self-reported questionnaire consists of seven items exploring three different types of physical activities: walking, moderate-intensity activities, and vigorous-intensity activities over the past seven days. The duration and frequency of each activity are assessed within three intensity ranges. The energy expenditure for each type of activity is measured using multiples of metabolic equivalents (METs). Total activity is expressed as MET-minutes, calculated by multiplying the MET score by the number of minutes performed. To determine the walking score, the duration of walking in minutes is multiplied by 3.3 METs. The moderate-intensity activity score is obtained by multiplying the duration of moderate-intensity activity in minutes by four METs, while the vigorous-intensity activity score is calculated by multiplying the duration of vigorous-intensity activity in minutes by eight METs. A total of 3000 MET-minutes per week or less indicates that participants are considered physically inactive (Craig et al., 2003).
Data Collection
After the necessary official permissions had been secured, students were informed of the purpose of the study from the university’s official e-mail address, with those choosing to participate signing informed consent was. Exclusion and inclusion criteria were clearly stated in the informed consent form, and students who did not give consent were excluded from the study. To minimize physical contact due to the COVID-19 pandemic, data were collected through an online survey. The survey allowed participants to provide information on topics such as their health habits, COVID-19 knowledge, precautions taken, and the effects of the pandemic on their mental health.
Statistical Analysis
The data were examined using SPSS Statistics 22.0, with six hundred and seventy students taking part in the survey. Table 1 shows the frequency and percentage distributions of demographic data. The Pearson Chi-Square test was used to examine the relationships between the variables. The Kolmogrov-Smirnov Test of Normality was performed to determine whether the data showed normal distribution and whether the test would be parametric or non-parametric. The Levene test was used to examine the homogeneity of variances. The parametric test was conducted for the variables that met assumptions, and the non-parametric test was used for those that did not. An independent, two-sample t-test was used to assess the difference between the two groups. The Tukey Test or the Mann Whitney U Test was used in post-hoc tests to compare the groups with differences. A significant value of .05 was used. Comparative analyses used one-way ANOVA and Pearson correlation. In the Pearson correlation, the absolute values of r were classified as follows: 0-.19 indicates a very weak correlation, .2-.39 indicates a moderate correlation, .40-.59 indicates a moderate correlation, .6-.79 indicates a strong correlation, and .8-1 indicates a very strong correlation. Data was considered statistically significant at p < .05.
Ethical Considerations
For all studies conducted during the COVID-19 period, the necessary permissions were obtained from the Turkish Ministry of Health. Permission was also obtained from the institution where the scientific research was conducted. The Selçuk University Faculty of Medicine received approval from the non-invasive ethics committee (IRB: 2022/07). All the procedures in this research were carried out in accordance with The Declaration of Helsinki, with informed consent being obtained from all students.
RESULTS
Sociodemographic Characteristics of Participants
Eighty-four percent of the students in the study were female, with an average age of 20.67 ± 2.34. Most participants (26.3%) were studying medical imaging and medical laboratory techniques; 63.1% were second year students, and 61.3 lived with their families. A total of 81.3% of the participants had nuclear families; 59.9% had an income equal to their expenses; 93.9% did not have a chronic disease; 20.7% reported that they smoked, and 94.0% stated that they did not use alcohol. In addition, most students reported an increase in their Internet and smart phone use during the pandemic (92.5% and 94%, respectively) (Table 1).
PSQI Components and Mean Global PSQI Scores, Mean IPAQ-SF Score, and Mean MET Scores of Participants
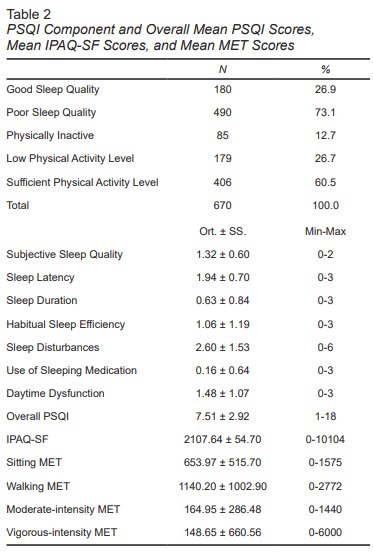
The Mean Global PSQI score of students was 7.51 ± 2.92. An examination of the mean scores for PSQI components revealed that 26.9% of students had a mean score above five in the following components: subjective sleep quality (1.32 ± .60), sleep latency (1.94 ± .70), sleep duration (.63 ± .84), habitual sleep efficiency (1.06 ± 1.19), sleep disturbances (2.60 ± 1.53), use of sleeping medication (.16 ± .64), and daytime dysfunction (1.48 ± 1.07). After analyzing participants’ physical activity levels, we found that 12.7% were not physically active, 26.7% had low levels of physical activity, and 60.5% had sufficient activity levels. The mean IPAQ-SF score of participants was 2107.64 ± 54.70 MET-min/week. The sitting MET score was 653.97 ± 515.70, the walking MET score was 1140.20 ± 1002.90, the moderate-intensity activity MET score was 164.95 ± 286.48, and the vigorous-intensity activity MET score was 148.65 ± 660.56 (Table 2).
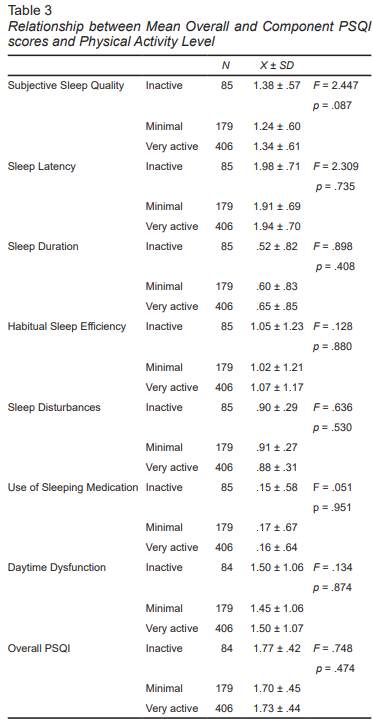
Relationship between Overall and Component Mean PSQI Scores and Physical Activity Levels of Participants
The relationship between PSQI components and each participants’s mean overall score and their degree of physical activity was examined. No appreciable difference was observed in the quality of sleep between students who were physically active and those who were not (Table 3).
Correlation between the Mean PSQI Component Score, PSQI and Overall MET Score of Participants
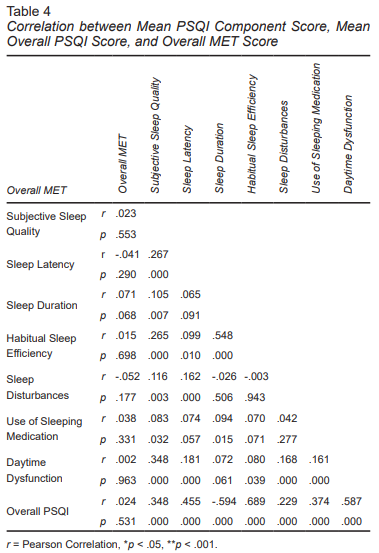
The overall PSQI-score and overall MET score showed a weak, non-significant correlation (r = -.024, p = .531). A somewhat positive correlation was found between sleep duration and habitual sleep efficiency. We found that sleep length increased with habitual sleep efficiency. A moderate positive correlation was identified between the overall PSQI score and the components of sleep latency and daytime dysfunction, indicating that as the overall PSQI score increased, so did sleep latency and daytime dysfunction levels. In addition, a moderate negative correlation was observed between the overall PSQI score and sleep duration, suggesting that higher PSQI scores were associated with shorter sleep duration. It was found that sleep duration decreased as the overall PSQI score increased. Moreover, a significant correlation was observed between habitual sleep efficiency and the overall PSQI score. As the overall PSQI score increased, so did habitual sleep efficiency. Although the associations with other variables were statistically significant, they were found to be weak, low, or very low in strength (Table 4).
DISCUSSION AND CONCLUSION
This study examined the sleep quality and physical activity levels of young adults during the COVID-19 pandemic and evaluated the relationship between these two variables.
Sleep Quality of Young Adults
In our study, the mean PSQI score of participants was 7.51 ± 2.92, with 73.1% being found to have poor sleep quality. An examination of sleep quality showed that sleep disturbances (2.60 ± 1.53) and sleep latency (1.94 ± .70) had the highest mean scores. This rate is higher than the mean sleep quality scores reported in previous studies in Turkey, in which the PSQI was used as a data collection tool: 6.15 ± 1.90 (Aysan et al., 2014), 7.89 ± 2.36 (Kucukgoncu et al., 2010), 6.90 ± 2.4 (Saygılı et al., 2011), and 6.28 ± 3.05 (Şenol et al., 2012). Given that the rates of students with poor sleep quality reported in the literature generally vary between 50% and 60%, the 73.1% rate in our study clearly demonstrates how conditions during the pandemic negatively affected sleep quality. It has been reported that COVID-19 negatively affected individuals’ sleep quality by 7.88 ± 3.43 (Xiao et al., 2020). The study conducted by Ramos Socarras et al., (2021) on 583 adolescents and young adults in Canada revealed that the COVID-19 pandemic negatively affected sleep patterns, delaying the onset of sleep, and leading to an increase in waking up early at night and in the morning, and the frequency of nightmares (Ramos Socarras et al., 2021). In the study conducted by Pinto et al., (2020) in Portugal, 69.6% of participants reported at least one sleep difficulty, with frequent waking up being identified as the most common problem (Pinto et al., 2020). A study conducted by Oliveira Souza et al., (2023) found that 40% of middle-aged adults experienced sleep quality deterioration during the pandemic, with 30% of participants experiencing sleep disorders due to social isolation (Oliveira Souza et al., 2023). These studies show that the anxiety and stress caused by the pandemic significantly reduced sleep quality by increasing the difficulty of individuals in initiating and maintaining sleep. However, sleep problems can also trigger other problems. In a study evaluating the sleep problems of young adults, irregular sleep habits, insufficient sleep duration, and poor sleep quality were identified as common problems. It also reported that young adults use substances such as alcohol and non-prescription drugs to maintain their sleep patterns and use stimulants to stay awake (Işık et al., 2015; Cheng et al., 2012). It was observed that these sleep problems affected students’ daily life activities and safety, and in some cases, they fell asleep while driving and caused accidents. It was observed that poor sleep quality not only caused health problems in participants, but also poor academic performance, distraction, and lack of motivation. It has been reported in the literature that poor sleep quality causes problems such as falling asleep in class, low grade point averages, and general sluggishness in daily life (Aysan et al., 2014). These findings show that young adults tend to use risky strategies for sleep management and that this situation has reached levels that can jeopardize their health and safety (Köktürk et al., 2021).
Smartphone, Internet, and Smoking Habits of Young Adults
Certain routines and habits of individuals changed during the pandemic. This study found that alcohol and cigarette use increased among young adults. In addition, 92.5% of participants reported an increase in internet use and 94% in smartphone use. A similar increase in these habits in young adults was also reported in the literature during this period (Rabia & Fazlıoğulları, 2021; Capdevila-Gaudens et al., 2021; Cardoso et al., 2022). Tahir et al., (2021)found a link between internet addiction and insufficient sleep. The same study revealed that internet addiction accounts for 13.2% of the variance in poor sleep quality and is a significant predictor of poor sleep quality. In particular, it has been observed that increased screen time suppresses melatonin secretion, making it difficult to fall asleep and reducing sleep quality (Tahir et al., 2021). A systematic review and meta-analysis examining the prevalence and risk factors of mental health problems among medical students during the COVID-19 pandemic revealed that individuals in this group were more prone to health problems linked to conditions during the pandemic. The same study showed that the increase in smartphone and internet use, in particular, had negative effects on health by increasing the risks of problematic use and addiction among young people. These effects were more pronounced and jeopardized the quality of life in groups under academic and professional pressure, such as medical students (Peng et al., 2023). Our study also emphasizes this increase in screen time during the pandemic, highlighting its indirect effects on sleep quality.
Physical Activity of Young Adults
In this study, the physical activity levels of the students were evaluated using IPAQ-SF. It was found that 60.5% of participants had sufficient physical activity levels, 26.7% showed low-level physical activity, and 12.7% were completely physically inactive. The average MET score was found to be 2107.64 ± 54.70 MET-min/week. In addition, the MET sitting time score was 653.97 ± 515.70, the MET walking score was 1140.20 ± 1002.90, the moderate-intensity MET score was 164.95 ± 286.48, and the high-intensity MET score was 148.65 ± 660.56. These findings show that the physical activity levels of the participants were largely based on low- and moderate-intensity activities. The lockdown and social isolation measures implemented during the pandemic significantly affected physical activity levels. Our study observed that physical activity was largely concentrated in low-intensity activities (such as walking). According to the literature, this situation was related to the restriction of outdoor activities, forcing people to engage in indoor activities requiring less movement during the pandemic. In particular, the fact that high-intensity physical activities were quite low (148.65 ± 660.56%) may reflect the restrictive effect of the pandemic on physical activity. It has been reported in the literature that high-intensity physical activities have a more pronounced effect on sleep quality (Erdogan & Revan, 2019). This effect may not have been seen in our study since the majority of participants engaged in low-intensity activities. Other factors related to the pandemic, such as increased screen time and internet addiction, may offset the positive effects of physical activity on sleep (Tahir et al., 2021).
In conclusion, this study examined the sleep quality and physical activity levels of young adults during the COVID-19 pandemic, revealing the complex effects of conditions during the pandemic on these two major health indicators. A significant proportion of participants (73.1%) had poor sleep quality, associated with the uncertainty, stress, and changing life habits caused by the pandemic. In addition, it was found that low- and moderate-intensity physical activity accounted for most of the physical activity and although physical activity levels were generally found to be sufficient, this did not show a significant relationship with sleep quality. This situation indicates that increased screen time, psychological stress, and social isolation during the pandemic may offset the positive effect of physical activity on sleep. The significant increase in internet (92.5%) and smartphone (94.0%) use during the pandemic is a key factor indirectly affecting sleep quality. This finding is consistent with the literature showing that excessive use of digital devices is associated with circadian rhythm disorders and difficulty falling asleep. In addition, problems observed in sleep components such as sleep latency, sleep duration, and daytime dysfunction reveal how poor sleep quality negatively affects young adults’ daily lives and academic or occupational performance. These findings clearly demonstrate that both the physical and mental health of young adults should be supported in crisis situations such as the pandemic. Health authorities and educational institutions can provide online exercise programs to encourage young adults to engage in regular physical activity, awareness campaigns to develop healthy sleep habits, and guidance for limiting screen time. In addition, encouraging high-intensity physical activities and strengthening young adults’ stress coping mechanisms are critical to improving their overall health and well-being. Although this study provides relevant information on understanding the health behaviors of young adults under pandemic conditions, causal relationships cannot be established due to their cross-sectional design. Future studies could examine the relationships between physical activity, sleep quality, and other psychosocial factors more comprehensively. In addition, the long-term effects of digital addiction and post-pandemic lifestyle changes on sleep and physical activity should also be explored. These studies could provide a significant foundation for developing health policies and supporting the health of young adults.