INTRODUCTION
Alzheimer’s Disease (AD) is a progressive, irreversible, and incurable neurodegenerative disease. Its main characteristics include functional and cognitive alterations such as memory deficit, apraxia, aphasia, visual-spatial issues, posterior and anterior cortical atrophy, loss of independence, and behavioral changes. AD is further categorized into mild or early onset, moderate, advanced, or late stage. It affects 10% of older adults aged over 65 and 50% of those aged over 85, making it the most common type of dementia (Zvěřová, 2019). Although the scientific literature is still unclear as to the exact cause of the disease, the hypotheses currently under evaluation include extracellular aggregation of neuritic plaques with beta-amyloid peptides (Aβ), neurofibrillary tangles, synaptic loss, microglial activation, loss of pyramidal neurons, and dominant autosomal genetic alteration (Srivastava et al., 2021).
As AD progresses, individuals become increasingly dependent, requiring assistance with both basic and complex daily activities. Caregiving for these individuals results in caregiver burden, with major contributing factors including the sex of the caregiver, lack of free time, number of hours spent caregiving, years of caregiving, caregiver self-esteem, and the severity of the patient’s AD (Pudelewicz et al., 2019). A significant increase in caregiver burden ranging from 47.4% to 56.8% was observed in those looking after dementia patients over a period of three years (Connors et al., 2019).
Historically, women have been the primary caregivers of older adults, particularly those with AD, due to ingrained cultural and social factors (Yakubu & Schutte, 2019). This pattern is influenced by cultural norms that often associate caregiving responsibilities with the female sex, reflecting the expectation that women will assume caregiving roles within the family and society (Rosende-Roca et al., 2022).
In addition, social aspects such as the unequal division of domestic labor and women’s lower participation in high-status professional positions may exacerbate this responsibility (Yakubu & Shutte, 2019). This caregiving model can significantly impact on the quality of life of caregivers, as they often experience physical and emotional overload, leading to high stress levels and negative mental health effects. Insufficient social support coupled with a lack of caregiving resources can further compound these challenges, highlighting the need for policies that acknowledge and support caregivers (Delfino et al., 2018).
Regardless of their sex, caregivers experience high rates of depression and mental health issues including reduced emotional well-being, disruption of social life, feelings of loss of control over their personal lives, and physical stress, all of which affect their quality of life (Family Caregiver Alliance, 2020; Shafizadeh et al., 2020).
The concept of Quality of Life (QoL) is diverse and subjective. Multidimensionally assessed through an individual’s perception of aging and personal identity, it is related to both physical and mental health (Fagerstrom et al., 2020). QoL and caregiver burden are key variables to be considered in elder care, requiring the implementation of effective strategies to enhance the QoL of caregivers of older adults with Alzheimer’s Disease to prevent further deterioration of their conditions (Kawaharada et al., 2019).
It is therefore crucial to understand the challenges faced by caregivers of older adults with AD. Understanding how caregiver burden affects their QoL is essential for developing support and intervention strategies. In addition, the results of this study can inform resource allocation, and the development of public policies designed to support caregivers, recognizing their importance in the health and well-being of the older population. This study therefore seeks to analyze whether increased caregiver burden among caregivers of older adults with AD negatively impacts their perceived QoL.
METHOD
Study Design
This quantitative, analytical, observational, cross-sectional study was developed according to the guidelines of Strengthening the Reporting of Observational Studies in Epidemiology (STROBE).
Participants
A non-probability sample was intentionally and conveniently chosen, consisting of 126 formal (professional) or informal (family) caregivers of older adults with AD residing in various regions of Brazil. In this country, formal caregivers are professionals who have at least completed secondary education and undergone specialized training. They may also include professionals with higher education, such as nurses, who have received additional caregiving training.
Only caregivers of older adults diagnosed with AD (as reported by the caregivers themselves) of either sex, aged 18 years or older, residing in all regions of Brazil, were included. Caregivers of institutionalized or hospitalized older adults were excluded.
Measurements
A questionnaire developed by the authors was used to assess the sociodemographic, health, and care profile of older adults with AD, with questions regarding age, age group, sex, family income, educational attainment, retirement status, and length of time since diagnosis. Another questionnaire containing questions on the caregiver’s age, age group, sex, family income, educational attainment, length of time and number of hours a day spent providing care for the older adult with AD, and whether they reside in the same household as the older adult was used to evaluate the caregivers.
The Zarit Caregiver Burden Interview was employed to assess caregiver burden. This instrument evaluates caregivers’ perceived burden, focusing on how their caregiving activity impacts their personal, social, financial, physical, and mental health. The instrument comprises 22 items to be answered by the caregiver using a 5-point Likert scale ranging from 0 points (never) to 4 points (always), with a total score of 0 to 88 points, with higher scores indicating more significant caregiver burden (Taub et al., 2004).
The WHOQOL-Bref, a shortened version of the World Health Organization Quality of Life assessment questionnaire, was used to evaluate caregivers’ QoL. It consists of 26 questions, two of which concern individual perceptions of QoL and health, while the rest are subdivided into physical and psychological aspects, social relationships, and environmental domains. Each domain ranges from four to 20 points, with higher scores indicating better QoL in the domain evaluated (Fleck et al., 2000).
Procedures
A link was created to host the electronic questionnaire developed for the study, and quantitative data were collected through an online form provided by the Survey Monkey platform. Contact was established with the Brazilian Alzheimer’s Association (ABRAz) so that they could send the research form link to registered caregivers. To broaden the scope of the national sample, assistance was requested from elder caregiver training course instructors and the directors of caregiver training schools.
The survey link was also distributed through the authors’ social media platforms (Facebook™, Instagram™, and WhatsApp™). The platform remained open to receive responses from participants for 90 days (from February to May 2023). Before completing the questionnaire, participants received brief instructions containing information on the research objectives, target audience, and the estimated time required to complete the questionnaire (approximately 15 minutes). Interested participants were first required to fill in the Informed Consent Form (ICF) on the online platform, indicating their agreement.
There was no pre-selection of who would receive the invitation to participate. The invitation was widely shared on the authors’ social media platforms, with a link containing the ICF and research instruments. In the posts, we asked those who knew caregivers of older adults with Alzheimer’s disease to share the link with them to identify potential participants.
There was no direct contact between the researchers and potential participants. Those who were interested, met the inclusion criteria, and accepted the ICF were allowed to access the link and complete the questionnaire. Since the questionnaires were hosted on Survey Monkey, the responses were automatically saved in an Excel spreadsheet at the end.
The exclusive use of the authors’ social media for dissemination allowed us to reach a broad, varied network, enabling the research team to reach caregivers of older adults with AD in various regions of Brazil.
Statistical Analysis
Data analysis was performed with SPSS 25.0 software using descriptive and inferential statistical approaches. Frequency and percentage were used as descriptive measures for categorical variables. Data normality was assessed using the Kolmogorov-Smirnov test, and skewness and kurtosis coefficients were used for numerical variables. Bootstrapping procedures (1000 re-samplings; 95% BCa CI) were also performed to enhance result reliability, correcting for potential deviations from sample normality and differences between group sizes, and to achieve a 95% confidence interval for the means (Haukoos & Lewis, 2005). Pearson correlation was used to explore the association between caregiver burden levels and caregivers’ QoL domains. Simple linear regression analysis was employed to determine whether caregiver burden level (independent variable) predicts caregivers’ perceived QoL (dependent variables). Five simple linear regression models were used with the enter method. There were no sufficiently strong correlations between variables to indicate multicollinearity issues (Variance Inflation Factor/VIF < 5.0). Pearson’s Chi-square test (X2) was used to analyze sociodemographic, health, and professional performance factors associated with caregiver burden levels. One-way Anova, followed by Tukey’s Post-Hoc, was used to compare QoL domains based on caregiver burden levels. A significance level of p < .05 was used.
Ethical guidelines
The study was approved by the Cesumar University Research Ethics Committee (Unicesumar), with approval number 6.001.701/2023, and followed the research standards in human subjects established in Resolution 466/12 of the National Health Council. All participants signed the Informed Consent Form.
RESULTS
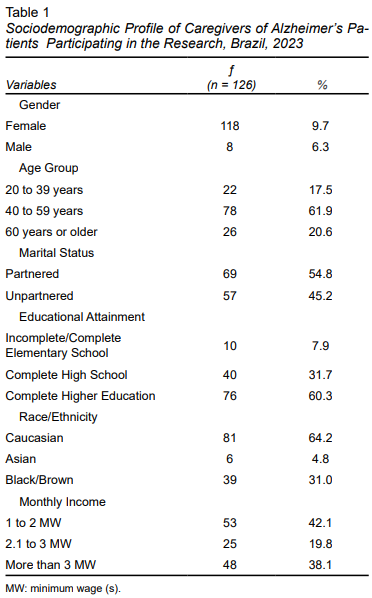
A total of 126 caregivers participated in the research, comprising 118 females and eight males, with ages ranging from 22 to 80 years (M = 51.36; SD = 10.90). The data in Table 1 reveal a predominance of caregivers who were in the 40 to 59 year age group (61.9%), partnered (54.8%), had completed higher education (60.3%), were Caucasian (64.2%), and earned a monthly income ranging from one to two minimum wages (42.1%).
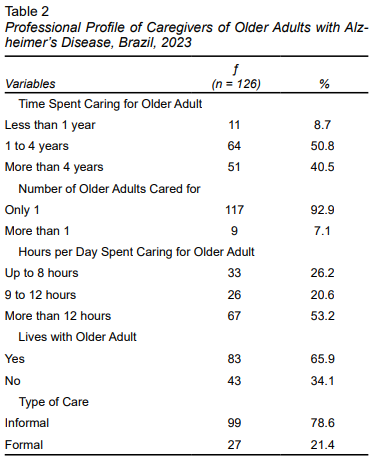
According to the results shown in Table 2, most caregivers reported having cared for only one older adult with AD (92.9%) for a period ranging from one to four years (50.8%) and for more than 12 hours per day (53.2%). Most of them also lived with the older adults (65.9%) and provided informal care (78.6%). The mean age of the older adults reported by caregivers was 81.48 (SD = 7.91) years.
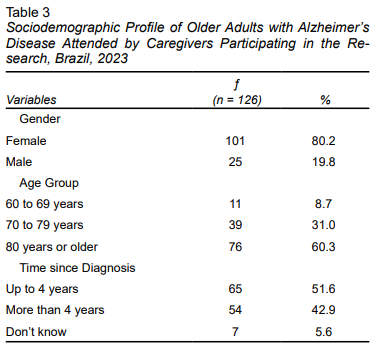
According to the caregivers (Table 3), most of the older adults with AD they cared for were female (80.2%), aged over 80 years (60.3%), and had been diagnosed with AD less than four years earlier (51.6%).
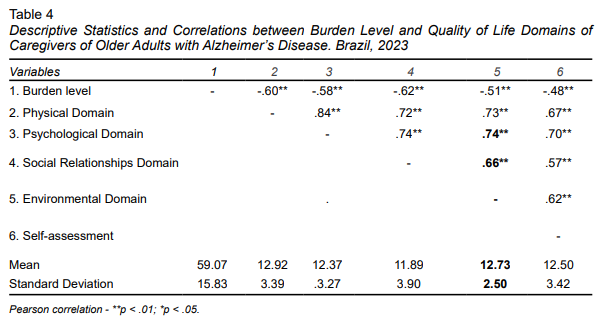
Table 4 shows that caregivers exhibited a slight burden overall (Md = 59.07; SD = 15.83). Regarding QoL, higher scores were observed in the physical domain (M = 12.92; SD = 3.39), followed by the environmental (M = 12.73; SD = 2.50), self-assessment (M = 12.50; SD = 3.42), psychological (M = 12.37; SD = 3.27), and social relationships domains (M = 11.89; SD = 3.90).
An analysis of the correlations between caregiver burden levels and QoL domains (Table 4) found that the burden levels perceived by caregivers had a significant (p < .05), negative, and moderate correlation (r = -.48 to -.62) with all QoL domains, indicating a moderate, inversely proportional association between caregiver-perceived burden and QoL. The QoL domains showed significant (p < .05), positive, and moderate to strong correlations (r = .57 to .84) with each other.
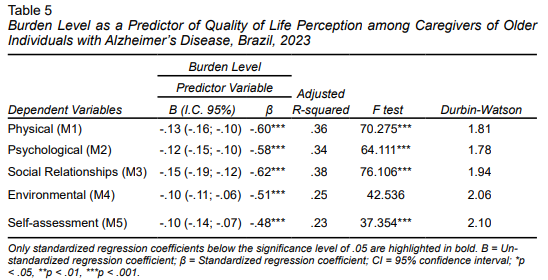
Table 5 shows the simple linear regression models of perceived caregiver burden level as a predictor of perceived QoL. The burden level explained a significant (p < .01) and moderate amount (R² between .23 and .38) of caregivers’ perceived QoL. Caregiver burden levels showed a significant (p < .01) and negative prediction (β = -.48 to -.62) across all QoL domains, showing that higher caregiver burden levels affect perceived QoL.
DISCUSSION AND CONCLUSION
The results of this study indicate that higher caregiver burden is linked to lower perceived QoL, showing that caregiver burden exists. The physical domain of QoL was identified as the most satisfactory, while the social relationships domain was considered the least favorable among caregivers. These findings underscore the interconnection between the various components of QoL.
It should be noted that 93.7% of the participants in our study were women, reflecting the predominant trend in the caregiving field. This result could have significant implications for understanding and managing sectoral demands. First of all, it points to the need to promote policies and initiatives to include and train male caregivers, foster greater diversity in the workforce, and potentially achieve a more balanced distribution of caregiving responsibilities (Furegato & Santos, 2012).
The fact that men are a minority in caregiving roles can be explained by cultural and social factors, such as the traditional association of caregiving with women, rooted in gender norms assigning the role of care and emotional support to women (Cruz & Handam, 2008). Additionally, barriers such as the perception of a lack of skill or empathy among men and the lower flexibility of work schedules associated with traditionally male-occupied professions could discourage their participation in this field (Hellis & Mukaetova-Ldinska, 2022).
At the same time, according to Luzardo, Gorini, and Silva (2006), the predominance of women also reflects family dynamics in which women often assume responsibility for caring for relatives, due either to their perceived availability or cultural expectations. These factors underscore the need for social interventions to challenge this cultural norm and promote more equitable participation by both sexes in caregiving.
The results indicating the predominance of caregivers aged 40 to 59 years, with higher education and a monthly income of one to two minimum wages, are due to several factors. According to Gutierrez et al. (2021), this age group coincides with a stage of life where many individuals have achieved a certain level of professional and personal stability, which could facilitate their involvement in caring for elderly family members. Moreover, higher educational attainment suggests that these caregivers may be better informed about the complexity of the disease and more willing to assume specialized caregiving roles (Farina et al., 2017).
Conversely, the limited monthly incomes of caregivers reflect the financial burden many families face, indicating that despite having academic qualifications, caregivers may experience financial challenges in balancing paid work and prolonged caregiving. This situation highlights the need for greater government and community support (Cheng, 2017).
The results show that most caregivers focus on caring for only one older adult with AD, which could be interpreted as a care management strategy, given the physical, emotional, and cognitive demands involved in this type of assistance. The period of one to four years reflects an early to intermediate stage of disease progression (Pinyopornpanish et al., 2022), in which symptoms still allow for a degree of autonomy albeit under constant supervision.
The fact that the caregiving workload exceeds 12 hours a day highlights the heavy dependence of older adults and the burden faced by caregivers, who often balance these demands with other responsibilities such as work and family life. Providing care 12 hours a day for one to four years can place a physical and emotional strain on caregivers, increasing the risk of burnout and health problems (Kim, Noh, Kim, 2021).
This scenario reinforces the need for social support and public policies to prevent physical and psychological exhaustion among caregivers and improve the quality of life of both the latter and older adults (Falcão et al., 2018).
Regarding older adults with AD, the results showed that over 80% were women aged over 80, who had been diagnosed with the disease less than four years earlier. It is important to note that the higher prevalence among women reflects their longer life expectancy, making them more likely to develop the disease, as the risk of AD increases with age (Paschalidis et al., 2023). Furthermore, according to Zhang et al. (2021), the predominance of older adults over the age of 80 aligns with the fact that Alzheimer’s disease (AD) typically manifests at advanced stages of life. Conversely, recent diagnoses may be related to increased awareness and efforts to promote timely diagnosis over the past few years, enabling symptoms to be identified in the early or intermediate stages of the disease (Khan, Barve, & Kumar, 2020).
Caregiver burden can be explained by the increased physical and emotional demands often accompanying this role. The constant physical and mental exhaustion can decrease available energy, contributing to a negative perceived QoL (Peixoto et al., 2022). These results are in line with previous research, such as the study conducted by Ibrahim et al. (2024) in Egypt, identifying an intense physical burden among caregivers of older adults with AD, whereas the psychological burden was considered to be lower, with approximately 30% of the sample reporting poor QoL.
It is important to note that caring for a person with AD requires significant time and energy, restricting the caregiver’s social and personal activities, and resulting in feelings of isolation and lower perceived QoL (Sklavou & Sarathanou, 2022). This is borne out by the research of Vu et al. (2022), in which 43% of 200 caregivers of older adults with AD reported feeling more isolated from their families, and 35.5% did not seek help from third parties. These data highlight the challenges caregivers face and the importance of addressing their social and emotional needs during caregiving.
It is also essential to note that caregiver burden is likely to harm caregivers’ interpersonal relationships, including those with their families, friends and intimate partners. The additional stress caused by this burden could presumably trigger conflicts and social distancing, compromising the quality of these relationships (Zahed et al., 2020; Duplantier & Williamson, 2023). These findings are consistent with the study by Nascimento and Figueiredo (2019) highlighting the difficulties caregivers of people with AD experience in their social relationships due to the additional fatigue and stress resulting from daily caregiving. This information underscores the need for support and adequate interventions for caregivers to preserve and enhance their interpersonal relationships despite the challenges of caregiving.
It is crucial to emphasize that caregiver burden is directly associated with mental health problems, such as anxiety and depression (Keklikçi, 2023), which has the potential to significantly impact perceived QoL (Pinyopornpanish et al., 2021). Moreover, in the context of informal caregivers, the financial burden associated with caring for a person with AD can cause additional concerns, potentially contributing to a negative perception of QoL. These financial worries can intensify existing stress and negatively influence caregivers’ perception of their well-being. In this respect, addressing these financial concerns and providing emotional support is essential to improving caregivers’ QoL and ensuring proper care for patients with AD.
Caregivers often devote so much effort to caring for patients with AD that they neglect their own needs (Alonso-Cortés et al., 2020). This was corroborated by a qualitative study conducted by Mattos et al. (2020), which, through focus group discussions with caregivers of older adults with dementia, found that the caregiving burden directly influences their self-care.
The lack of time for self-care, exercise, and enjoyable activities can result in a decline in caregivers’ physical and emotional health and contribute to a sense of lack of control over their own lives. This perception of lack of control can cause hopelessness and dissatisfaction (Talib et al., 2021; Villarejo-Galende et al., 2022). These findings highlight the importance of recognizing and addressing caregivers’ needs, promoting self-care strategies, and offering emotional support to counteract the adverse effects of the caregiving burden.
There are several hypotheses and possible explanations for the scenario in which caregivers of older adults with AD experience greater satisfaction in the physical than the social relationships domain. Caring for a person with AD often involves a series of physical tasks, such as assisting with mobility, bathing, and feeding (Chandran, 2021). It is important to note, however, the significant gap in studies exploring actions performed in the family caregiving context for these older adults, as highlighted by the scoping review by Silva et al. (2023).
Caregivers may indeed experience momentary gratification when performing these physical activities, resulting in a positive impact on the physical aspect of their QoL. These activities provide caregivers with a tangible sense of accomplishment, as they are concrete, measurable tasks. These achievements, in turn, can positively influence the overall perception of the physical domain of QoL (Bernardo & Raymundo, 2018). However, it is essential to note that while caregivers may derive satisfaction from performing the physical tasks associated with caregiving, there may be a need for additional support and intervention to strengthen caregivers’ social relationships. This is essential to promoting a more balanced, satisfactory QoL, and addressing caregivers’ physical and social needs.
Advancing AD can result in behavioral changes in patients, including social isolation and difficulties with social interactions (El-Haj et al., 2016; Zhang et al., 2022). Conversely, as observed in the publication by Shea et al. (2020), social isolation, particularly during the COVID-19 pandemic, exacerbated psychological and behavioral symptoms, such as mood changes and aggression, in three older adults with AD. This was due to the disruptions in their normal routines and lack of social interaction.
These changes can restrict caregivers’ opportunities to participate in social activities, negatively impacting the social relationships domain in their QoL, as observed in the present study. This dynamic underscores the importance of addressing both the social needs of patients with AD and those of caregivers by ensuring adequate support and interventions to promote a socially stimulating, supportive environment for all involved.
Additionally, the stigma associated with AD may lead caregivers to avoid social situations for fear of being judged or stigmatized (Monfared et al., 2023). In this regard, the study conducted by Gale, Acar and Daffner (2018) shows that the stigma associated with dementia, including AD, leads to negative consequences such as social isolation, difficulties in rehabilitation, and impacts on the caregiver’s health. This fear can contribute to an unfavorable perception of the domain of social relationships. These findings emphasize the importance of combating the stigma associated with AD and providing adequate support for caregivers to enhance the QoL and well-being of all those involved.
The positive correlation between all domains of QoL (physical, environmental, social relationships, psychological, and self-assessment) among caregivers of older adults with AD can be attributed to a series of interrelated factors. Caregivers who adopt a holistic approach to care, considering both the physical and psychosocial aspects of the patient, tend to experience improvements across all domains (Elagamey et al., 2022; Jayakodoy & Arambepola, 2023). Moreover, studies such as the one by Rozani et al. (2022) demonstrate that interdisciplinary programs encompassing physical, psychoeducational, cognitive, behavioral, and health education components have the potential to reduce caregiver burden and improve health-related QoL. This comprehensive approach can contribute to a positive perception of QoL.
It is important to note that caregivers who develop personal resilience and adopt effective coping strategies tend to cope better with the stress associated with caring for people with AD (Rosa et al., 2020; Han et al., 2019). These positive characteristics have the potential to positively influence all domains of QoL. However, it is interesting to note that the research by Durán-Gómez et al. (2020), conducted of 120 caregivers of people with AD in Spain, concluded that those reporting higher levels of resilience displayed indicators of moderate to intense caregiver burden. However, they also demonstrated fewer depression and anxiety symptoms. These results suggest that resilience may play a role in protecting against the negative impacts of caregiving, despite the perceived burden.
Notwithstanding its important findings, this study has certain limitations. First, the fact that it is an observational, cross-sectional study means that it is not possible to infer causality. Moreover, the nature of this study limits the ability to establish temporal relationships between the variables, making it challenging to determine whether the observed associations are a cause or a result of the phenomena analyzed. Findings should therefore be interpreted with caution, acknowledging these limitations.
The sample may not be representative enough of the general population of caregivers of patients with AD, as it only includes a particular demographic group. Additionally, the use of self-reported questionnaires may introduce biases of self-assessment and subjectivity into the results. The lack of control over potentially confounding variables, such as the severity of the patient’s AD or the social support available to caregivers, may also limit the generalizability of findings. Another possible limitation is the absence of longitudinal follow-up, which could provide deeper insights into changes in caregiver burden and QoL over time. These considerations underscore the need for future research with more comprehensive methods and more representative samples to corroborate and expand the results of this study.
Another limitation of the study is the inability to confirm whether the individuals under care have AD, due to the type of methodology used. The study relies on self-reported data and does not include molecular studies or precise etiological diagnoses for dementia, meaning that the AD diagnoses could not be conclusively verified. Further, this study only focused on the psychological domain associated with chronic stress on caregivers, since it did not explore the importance of the professional and sociodemographic variables in the association between burden and quality of life. Future research should therefore explore this gap.
Based on the research results, there is significant evidence of a correlation between perceived caregiver burden and all domains of QoL, suggesting an inversely proportional relationship. Additionally, it was found that increased caregiver burden compromises caregivers’ perceived QoL. These conclusions highlight the need for interventions designed to reduce the burden and enhance the QoL of caregivers of older adults with AD.