INTRODUCTION
Although there is no clear consensus over the definition of shame, it is commonly described as a self-conscious, aversive emotion related to negative self-evaluation and a desire to escape or hide from certain experiences (Tangney & Dearing, 2002). Gilbert (1998) describes it as the experience of being in the world as an undesirable self with lower social value. From an evolutionary perspective, it has been posited that shame serves a survival function within a social context of interdependence, where it constitutes a response to a social threat to prevent rejection and exclusion (Fessler, 2004; Gilbert, 2007). In addition, a distinction is made between internal and external shame: internal shame refers to negative self-perception, whereas external shame is related to the social world and the way an individual assumes they exist in the minds of others, with the belief that others perceive them negatively (Gilbert, 2007; Matos & Pinto-Gouveia, 2010).
Gilbert (2022) notes that shame is the most common transdiagnosis phenomenon and may be the most difficult to manage. Its impact on the psychotherapeutic process is evident because people with high levels of shame assume that by disclosing information, they will be evaluated negatively by others, including therapists, which is why they may not go to psychotherapy or omit information relevant to the process (DeLong & Kahn, 2014; Griffin et al., 2022; McElvaney et al., 2022).
External shame has also been associated with various disorders, such as depression (Matos et al., 2013; Nikolić et al., 2022), anxiety (Cândea & Szentagotai-Tătar, 2018), posttraumatic stress disorder (Cunningham et al., 2018), dissociative disorder (Dorahy et al., 2017), psychosis (Brand et al., 2022; Martins et al., 2020), and borderline personality disorder (Göttlich et al., 2020; Rüsch et al., 2007).
Shame plays a key role in complex posttraumatic stress disorder (C-PTSD). The most recent version of the International Classification of Diseases (ICD-11; World Health Organization, 2019), distinguishes between PTSD and C-PTSD.
PTSD requires the presence of three symptoms constituting the PTSD cluster: re-experiencing, avoidance, and a sense of current threat. A C-PTSD diagnosis requires the presence of the cluster symptoms of PTSD, together with three additional symptoms comprising the disturbances in self-organization (DSO) cluster: affective dysregulation, negative self-concept, and alterations in relationships. This distinction has been widely validated, and it has been posited that one of the main differences between these disorders is that C-PTSD can be conceptualized as a shame disorder (Salter & Hall, 2022) and that shame plays a moderating role between the traumatic experience and the symptoms associated with C-PTSD (Rushforth et al., 2022).
Scales have been developed to evaluate external shame because of its association with various disorders and its impact on the psychotherapeutic process. One of the most widely used instruments is the Other as Shamer Scale (OAS), (Goss et al., 1994) an adaptation of the Internalized Shame Scale (ISS) (Cook, 1987). In the original study conducted of a sample of British students, three factors were identified: 1) being seen as inferior, 2) emptiness and 3) how others behave when they see me make mistakes. Being seen as inferior explained the highest proportion of the variance, while emptiness had the greatest association with psychopathology. This factorial solution showed adequate psychometric properties, as a result of which the scale has been used in various studies (see for example Castilho et al., 2017). However, despite the identification of these three factors, it is common for the instrument to be scored using a global score that combines the three factors into one (see for example Carter et al., 2021).
There is now a brief version of the OAS developed by Matos et al. (2015), and both the original and the abbreviated scales have been translated into several languages. Balsamo et al. (2015) evaluated the original version in 687 Italian students, finding that a hierarchical model with three first-order factors provided the most adequate fit. Likewise, they found that the emptiness factor was associated with depression. Hiramatsu et al. (2020) evaluated this same version in 199 Japanese students using item response theory (IRT), concluding that the instrument adequately discriminates between groups with high and low levels of shame.
The OAS-2, the shortened version developed by Matos et al. (2015) containing eight of the 18 items in the original version, was evaluated in Portugal with 312 students and 378 participants from the general population. This version was organized into a single factor and showed similar fit and reliability indices to those for the original version. These results were replicated in later studies, such as those by Saggino et al. (2017) with Italian students, Satici and Deniz (2020) with Turkish students, Gull et al. (2022) in Pakistan with the general population and Vagos et al. (2016) for the adolescent version.
Matos et al. (2015) note that the OAS-2 is an efficient, economical instrument of great use in research. However, it loses some of the information associated with the three factors in the original version, which could be useful in clinical practice. Understanding these factors can enhance the therapeutic process by identifying the impact of shame on various populations, making it possible to tailor interventions more effectively. Taking this into account and considering that most of the previous research was conducted with students, we decided to evaluate the original version by comparing the responses provided by a general population sample and a sample of the population with symptoms associated with PTSD, Disturbances in Self- Organization (DSO), and C-PTSD.
METHOD
Participants and Procedure
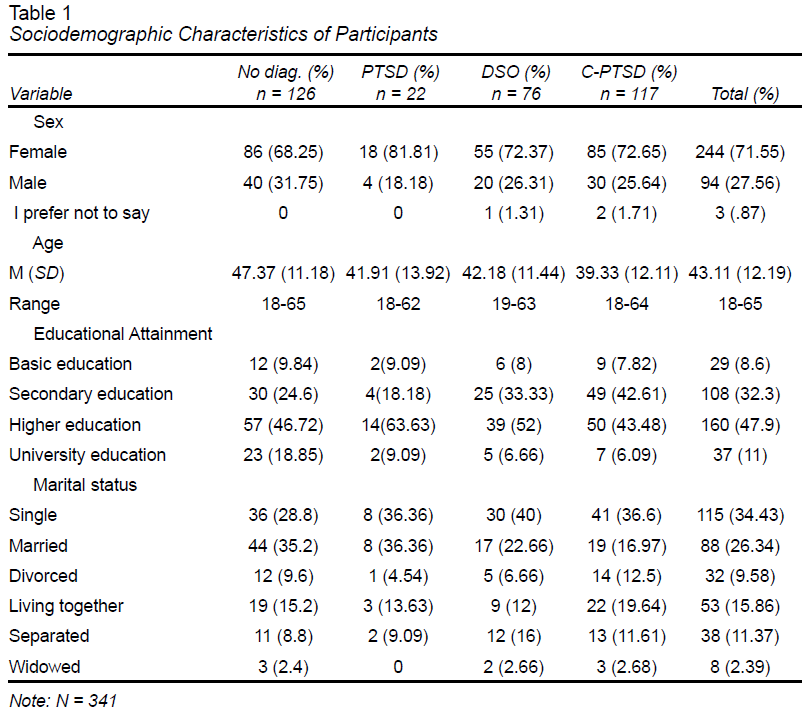
Convenience sampling was used to recruit 341 Mexican participants, who were asked to complete an online survey on the LimeSurvey platform from November to December 2021. The characteristics of participants are shown in Table 1.
Although no personal information was collected, all participants provided their informed consent in the consent section on the first page of the survey and were informed that they could drop out whenever they wished. In addition, the principal investigator’s contact email was provided in case they wished to obtain more detailed information on the study. Sociodemographic data were requested on the second page, after which the OAS and the International Trauma Questionnaire were presented sequentially.
Based on the results, four groups were identified: (1) C-PTSD, comprising individuals who met the diagnostic criteria for both the PTSD and DSO clusters; (2) PTSD, including individuals who met the criteria for PTSD but not for DSO; (3) DSO, consisting of individuals who met the criteria for the DSO cluster but not for PTSD; and (4) No Diagnosis, referring to individuals who did not meet the criteria for either PTSD or DSO.
Instruments
The Others as Shamer (OAS) (Goss et al., 1994) is a self-report scale with 18 items assessing the shame derived from how people believe others see them. A 5-point scale is used to collect responses (ranging from 0 = “Never” to 4 = “ Almost always ”). The scale comprises three factors: 1) being seen as inferior (“I feel other people see me as not good enough”), 2) emptiness (“Others see me as fragile”) and 3) how others behave when they see me make mistakes (“Others are critical or punishing when I make a mistake”). The sum of all the items serves as the final score, which ranges from 0 to 72; the higher the score, the greater the external shame. In the original study conducted of a sample of students from two universities, the scale showed adequate internal consistency (α = .92). The Latin American translation provided by the author was used.
International Trauma Questionnaire (ITQ) (Cloitre et al., 2018). The ITQ is a 12-item, self-report scale used to evaluate PTSD and C-PTSD based on the ICD-11 criteria. Participants indicate how much each of their central symptoms has bothered them in the last month, considering their most traumatic event, using a typical five-point scale ranging from “not at all” (0) to “extremely” (4).
Three items are used to evaluate each of the PTSD symptoms: re-experiencing (“Do you have upsetting dreams that replay part of the experience or are clearly related to the experience?”), avoidance (“Do you avoid internal reminders of the experience?”) and sense of current threat (“Are you “hyper-alert,” watchful, or on guard?”).
Three statements are used to evaluate the symptoms of disturbances in self-organization (DSO): affective dysregulation (“When I am upset, it takes me a long time to calm down”), negative self-concept (“I feel like a failure”), and alterations in relationships (“I feel distant or cut off from people”). Positivity for symptoms requires a score of ≥ 2 (“moderately”) for at least one of the items for each of the symptoms and a score of ≥ 2 for at least one of the three items for functional impairment due to PTSD and DSO (“In the past month, have the above problems affected your relationships or social life?”).
Both PTSD and DSO criteria must be met for a C-PTSD diagnosis. For a PTSD diagnosis, PTSD symptoms must be present, with no DSO symptoms. It is therefore possible to have a PTSD or a C-PTSD diagnosis but not both. Although the scale offers a categorical main result, a score can be calculated for each of the PTSD and DSO clusters by adding the items in each subscale.
The Latin American translation provided by the author was used.
Statistical Analysis
Confirmatory factor analysis (CFA) was performed with the total sample to obtain evidence of the construct validity of the scale. The fit of the models was evaluated from the adjusted chi-square (χ2), the Tucker‒Lewis Index (TLI), the Comparative Fit Index (CFI), the Root Mean Square Error of Approximation (RMSEA) and the standardized root mean square residual (SRMR). An absolute fit between the observed and expected covariance matrix is considered when χ2 p < .05, χ2 /df ≤ 2, TLI ≥ .95, CFI ≥ .97, SRMR ≤ .05 and RMSEA ≤ .05, and an acceptable fit is considered when χ2 p < .05, χ2/df ≤ 3, TLI ≥ .90, CFI ≥ .95, SRMR ≤ .10 and RMSEA ≤ .08 (Browne & Cudeck, 1992; Hu & Bentler, 1998; Schermelleh-Engel et al., 2003; Tucker & Lewis, 1973). McDonald’s Omega was used to evaluate the internal consistency of the factors as well as the full scale, given the ordinal nature of the items, where values ≥ .80 reflect adequate internal consistency (Cicchetti, 1994).
Finally, the ITQ was used to evaluate discriminant validity. One-way analysis of variance (ANOVA) was performed to analyze the differences in OAS scores between the ITQ-derived groups (no diagnosis, PTSD, DSO, and C-PTSD). Tukey’s post hoc test was subsequently used to compare the shame scores for the four groups. The Pearson correlation coefficient was also calculated between the subscales of the OAS and the subscales of the ITQ. Data analysis was performed using RStudio Version 1.4.1717C.
Ethical Considerations
This study was approved by the Ethics Committee of the Department of Psychology of the Universidad Iberoamericana with registration number 2022-02-005 in the 2022-2 ordinary session, held on April 28, 2022.
Participants whose results on the ITQ were consistent with PTSD, DSO, or C-PTSD were invited to participate in a second phase of the study, during which they could either receive treatment or be referred to mental health institutions in their area, as they wished.
RESULTS
Before performing CFA, a descriptive analysis of the items comprising the OAS was performed. The results confirmed that the 18 questions have a normal univariate distribution, while the bias and kurtosis were well below the cutoff points that would suggest a need to transform the data (Kim, 2013). In the corrected item-total correlation, since the lowest value corresponded to the OAS item 15 (ritc = .64) and the highest to the OAS item 08 (ritc = .86), none of the items were eliminated. The Mardia coefficients were significant (MKurt = 23.33, p < .001; Mskew = 2146.26, p < .001), suggesting that the data did not follow a normal multivariate distribution. Given the above and the fact that the items corresponded to an ordinal measurement level, it was decided that diagonally weighted least squares (DWLS) was the most appropriate estimator (Li, 2021; Shi & Maydeu-Olivares, 2020).
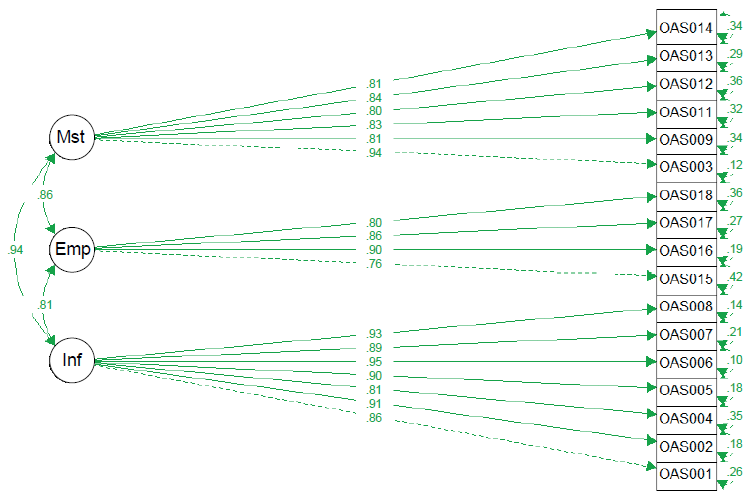
Two models were evaluated, with Model 1 being derived from the original study (Goss et al., 1994). This model comprised three factors: being seen as inferior (Items 1, 2, 4, 5, 6, 7 and 8), emptiness (Items 15, 16, 17 and 18) and how others behave when they see me make mistakes (3, 9, 11, 12, 13 and 14). Model 2 was composed of a single factor comprising all the items, since the total score was used to evaluate the scale (Hiramatsu et al., 2020).
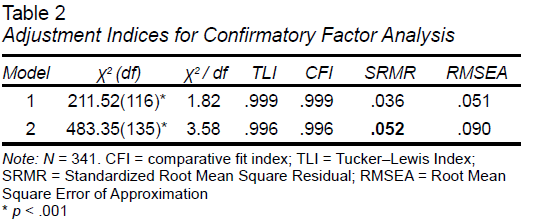
Table 2 shows the fit indices for the models. Model 1 (Figure 1) presented an adequate fit, whereas the adjusted χ2 criteria and the RMSEA were not met for Model 2.
Since CFA was conducted with the total sample, which included participants with and without clinical post-traumatic symptoms, invariance testing was performed between the group with clinical symptoms and the general population group. Model 1 achieved configural invariance, showing that the constructs measured by the OAS can be quantified using the same items across both samples.
After this level of psychometric equivalence had been established, factor loadings were constrained. A comparison of the fit indices of the constrained model with the configural model revealed no significant loss of fit, suggesting evidence of metric invariance between the samples (Δχ2 (14) = 22.59, p = .07).
The next step involved constraining item intercepts between the samples. In this case, a significant loss of fit was observed (Δχ2 (14) = 26.82, p = .02), indicating that this configuration of the OAS does not achieve scalar invariance. This result is due to the differences in symptom levels between the samples.
Internal Consistency
Total internal consistency was ω = .96 (95% CI = .96 - .97). For being seen as inferior, ω = .95 (95% CI = .94-.96), for emptiness, ω = .87 (95% CI = .85-.89), and for making mistakes, ω = .91 (95% CI = .90-.93).
Discriminant Validity
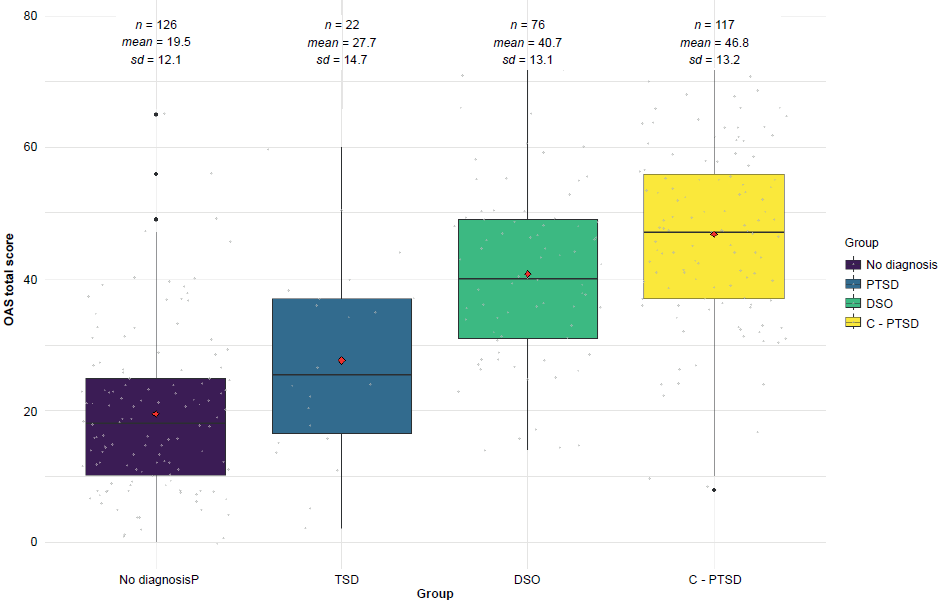
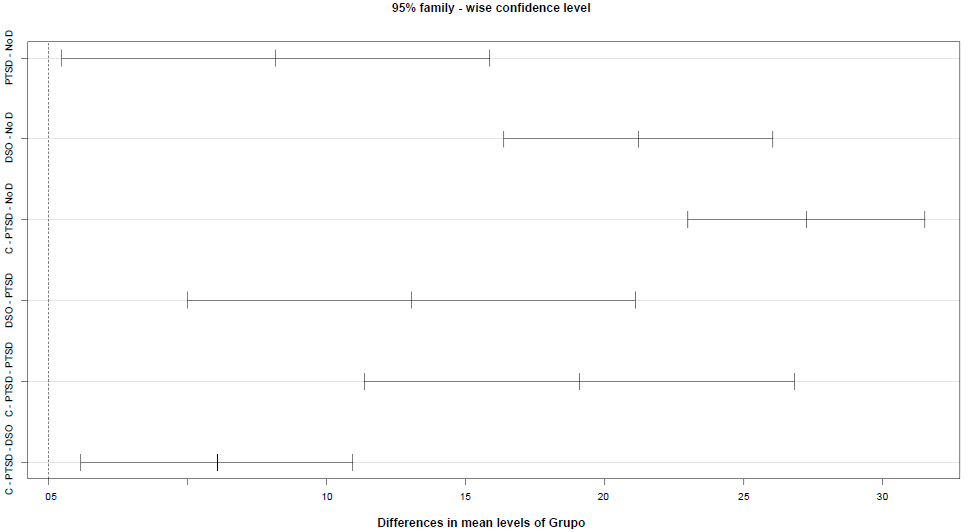
To evaluate the discriminant validity of the OAS, the differences in the OAS between the following four groups derived from the ITQ were evaluated: no diagnosis, PTSD, DSO and C-PTSD (Figure 2). One-way ANOVA showed that there was a statistically significant difference in external shame (F (3, 337) = 100.07, p < .001, η2 = .47) between the groups. Post hoc analysis using the Tukey test (Figure 3) found differences between all groups, with the greatest differences being observed between the group without a diagnosis and the C-PTSD group (p = .000, d = 27.27, 95% CI = 22.99 to 31.54).
DISCUSSION AND CONCLUSION
The aim of this study was to evaluate the psychometric properties of the OAS in the general population and a population with symptoms associated with PTSD, DSO and C-PTSD.
There is growing evidence of an association between external shame and various disorders, such as depression, anxiety, and posttraumatic stress disorder. Given that a moderating role of external shame has been identified in the effectiveness of the treatment, it is essential to evaluate instruments that allow the identification of this construct.
One of the most widely used scales to evaluate external shame is the OAS (Goss et al., 1994). This scale has been translated into several languages and has been used in various populations. However, no studies have evaluated its psychometric properties in a population with complex posttraumatic stress disorder.
Although there is an abbreviated version of the scale, we decided to evaluate the original version because although the former is a useful, economical resource in research, it loses some of the information on the dimensions of external shame explored in the original version that could be useful in clinical settings and research studies.
In addition, among the limitations commonly pointed out in previous studies, most of the analyses were conducted with student samples, the results of which may not be representative of other types of samples. We therefore decided to work with a sample of adults aged between 18 and 65 (with an average age of 43), unlike other studies in which the average age was approximately 20 (Balsamo et al., 2015; Hiramatsu et al., 2020; Saggino et al., 2017; Satici & Deniz, 2020).
Two models were evaluated: the 3-factor model of the original article and a model combining all the items into a single factor. The results suggest that the OAS is a valid, reliable instrument for the Mexican population and can be used to explore three factors: inferiority, emptiness, and mistakes.
The CFA showed that the 3-factor model has an adequate fit in terms of all the indicators. Despite having an adequate fit in terms of the CFI and the TLI, the 1-factor model had an acceptable but not excellent fit based on the normalized chi square and RMSEA values. The 3-factor model is therefore considered to be more appropriate although the use of the total score is justified.
The adjustment indices were similar to those obtained by Balsamo et al. (2015) and Vagos et al. (2016), who evaluated the 3-factor model of the original study with Italian adults and Portuguese adolescents respectively, obtaining similar results to those obtained in studies evaluating the OAS-2.
Regarding internal consistency, the use of the alpha coefficient to evaluate reliability is associated with a high probability of obtaining biased data. The omega coefficient is therefore recommended as a substitute, particularly when the items on a scale are scored with a Likert-type scale and the data are presented in a multidimensional way (Flora, 2020). Regardless of the use of a different coefficient, the value obtained (ω = .964) was higher than that reported in previous studies (Balsamo et al., 2015; Gull et al., 2022; Hiramatsu et al., 2020; Matos et al., 2015; Saggino et al., 2017; Satici & Deniz, 2020; Vagos et al., 2016).
To evaluate the discriminative validity, we decided to use PTSD, DSO and C-PTSD since a significant association has been found between external shame and posttraumatic symptoms (Brand et al., 2022; Dorahy et al., 2016; La Bash & Papa, 2013). Shame predicts more severe posttraumatic symptoms (Cunningham et al., 2018; Puhalla et al., 2021) as well as reducing the effectiveness of treatment. One element distinguishing C-PTSD from PTSD is the presence of DSO, which have been shown to be related to interpersonal factors (Bachem et al., 2021) in which shame plays an important role (Dorahy et al., 2009).
The differences in means show that there are differences in the levels of external shame when the presence of posttraumatic symptoms is considered. Results are consistent with those described by Dorahy et al. (2017), who found that people with C-PTSD symptoms have higher levels of shame than those without PTSD symptoms. However, a key fact is that according to the ICD-11 categorization, people who only presented symptoms of DSO (and did not meet the diagnostic criteria for PTSD or C-PTSD) had higher levels of shame than those in the PTSD group, followed by those in the C-PTSD group.
These results could indicate greater difficulties in people with C-PTSD as well as those with DSO, which could prevent help-seeking behavior or the disclosure of information in psychotherapy by these populations. Conversely, addressing these problems could increase the effectiveness of psychotherapy.
Regarding the limitations, the results may not be generalizable to all clinical populations. Likewise, although the differences were analyzed in relation to a sample that meets the diagnostic criteria for PTSD, DSO and C-PTSD using the ITQ, which has shown adequate psychometric properties and the ability to discriminate people with CPTSD, the results need to be supported by a clinical interview. Subsequent studies should therefore examine the validity of the OAS in people with a diagnosis confirmed through a clinical interview. Moreover, our sample size prevented us from performing an invariance analysis between symptom groups, which would have provided valuable information for those working with clinical samples.
Finally, it is essential to consider the cultural factor. Although some studies suggest that the experience of shame is similar across cultures (Matos et al., 2021), authors such as Kollareth et al. (2018) suggest that cultural aspects may influence the experience and expression of shame. For example, in shame research, it is often assumed that words associated with shame are equivalent across languages. However, differences exist between the meaning of the word “shame” in English and its Spanish translation "vergüenza". Whereas the term “shame” is associated with moral failure and has a stronger link to guilt, this association is less pronounced in its Spanish counterpart. It is therefore crucial for future research to integrate the cultural perspective when assessing the construct of shame to achieve a more comprehensive understanding.
Conclusion
The results of this study allow us to conclude that the OAS is a valid, reliable instrument for assessing external shame in the Mexican population and helps identify differences between the general population and individuals with post-traumatic symptomatology.
The clinical implications of this study are significant, as identifying shame as an issue to be addressed could help mitigate its impact. High levels of shame, for instance, may indicate the presence of comorbidities requiring evaluation, greater symptom severity, or potential obstacles in the therapeutic relationship, such as clients withholding information. Moreover, addressing shame could improve social interactions and foster the development of a positive self-concept, among other benefits.